Playlist
Show Playlist
Hide Playlist
Type I Hypersensitivity Reaction
-
Slides Immune-mediated Diseases Type I.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
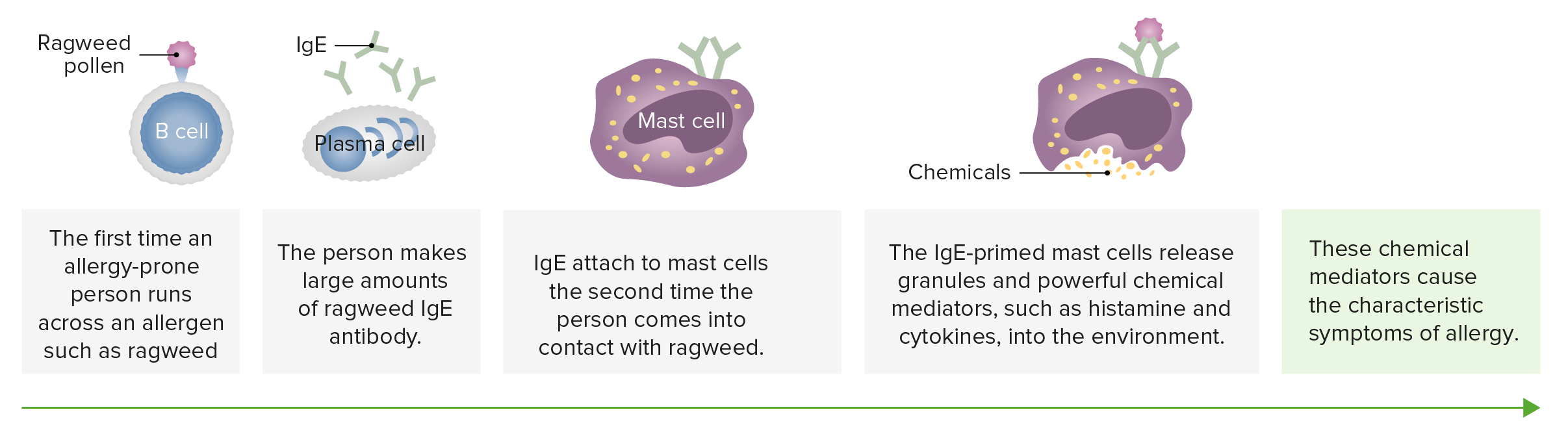
00:00 Welcome back. 00:02 We've laid the groundwork for talking about immune mediated diseases by talking about innate and adaptive immune components. 00:10 We've talked about macrophages and neutrophils and complement and natural killer cells as part of the innate response. 00:18 We've talked about helper T cells and killer T cells. 00:22 And B cells produce the antibodies as part of the adaptive immune response. 00:27 And now we're going to put them together and start talking about immune mediated diseases. 00:33 There are kind of four general categories as we'll see on the next slide. 00:36 This one is just type 1. 00:38 We're gonna emphasize just type one on this slide, which is IgE allergen mediated. 00:47 So, there are various mechanisms of immune mediated diseases, and these are generically called hypersensitivity reactions. 00:54 And for purposes of board examinations and other things, they're classically broken down into four basic types. 01:02 Type One is hypersensitivity response driven by Immunoglobulin E by IgE. 01:09 This is so called immediate type hypersensitivity, because the initial effects happen almost instantaneously once we've had a particular stimulus. 01:19 And these are going to be the hypersensitivity reactions that underlie allergy and anaphylaxis. 01:25 Type 2 that will come up in a subsequent talk that you're also going to enjoy famously, is type 2. 01:33 And this is antibody that is generated against a fixed antigen. 01:38 So an antibody that somehow recognizes the surface of a red cell because it binds to one of the surface molecules. 01:45 That will be type 2. 01:47 Type 3 is due to antigen antibody complexes. 01:51 Immune complexes that form with circulating proteins and antibodies. 01:57 And type 4 is cell-mediated. 02:00 And that could be cytotoxic T cells or it can be things related, diseases related to hypersensitivity from helper T cells. 02:10 A so called delayed type hypersensitivity, since it takes a while to get an accumulation of the the necessary effector cells and for them to elaborate their cytokines. 02:22 Once we have understood, which you now have understood, the fundamental kind of toolkit of the way that the immune system can respond with innate and adaptive immunity, the consequences of each of these types of hypersensitivity become completely predictable. 02:41 Okay, and so hopefully by is having said the predicate before, the details we're going to go into now we'll be just like, "Yeah, I got that." "Okay, I completely understand." As I said, we're going to emphasize type 1 hypersensitivity reactions in this talk. 02:57 So type one is mediated by IgE. 03:00 It's immediate type hypersensitivity. 03:02 We're looking at in the middle of the screen there a mast cell, a stylized version of a mast cell. 03:08 And on its surface, as you can see, on the upper right hand side, there are a number of IgE Fc receptors, so called Fc epsilon receptors. 03:17 Those are pre-loaded with immunoglobulin E. 03:21 So it's circulating antibody of a particular isotype that has bound to those receptors. 03:27 And basically, now it's it's a little landmine. 03:31 If allergens come along, and bind to the surface of the IgE that's already on its receptors will crosslink those IgE molecules and their receptors, and we'll get activation of the mast cell. 03:45 So that's exactly what happens with allergens. 03:48 And whether that's cockroach droppings, or cat dander, or pollens, they all have a polyvalent. 03:57 So multiple antigens lined up on a backbone that can crosslink the bound IgE. 04:03 Once that happens, that's a signal immediately for degranulation. 04:08 And release a various mediators. 04:11 So the granule contents include histamine and proteases, and various chemotactic factors. 04:17 That happens immediately. 04:19 That's why it's called immediate type hypersensitivity. 04:22 And histamine, for example, would cause increased vascular permeability, and vasodilation. 04:28 That's why if you have an allergy, you take an antihistamine. 04:32 That's to block the effects of the histamine causing the vasodilation increased vascular permeability. 04:39 It turns out that in the vessel bed, you get vasodilation, but in the airway beds and along the bronchioles, you'll get bronchoconstriction. 04:50 So you can begin to understand how asthma is going to happen, due to the effects of mast cell degranulation. 04:57 But that's not all the mast cells do once they've been activated through their Fc receptors. 05:02 They will also make a variety of arachidonic acid metabolites. 05:09 So once we've activated the mast cell, we activate phospholipids A2, which will break down various lipids present in the nuclear membrane, and will release arachidonic acid. 05:21 That's a 20 carbon with four unsaturation molecule that can then be converted into a variety of additional molecules, including leukotrienes and prostaglandins. 05:34 And we've talked about these previously when we talked about acute inflammatory responses. 05:39 Those membrane phospholipids breaking down will also make platelet activating factor, which is a very potent bronco constrictor and also vasodilator. 05:49 So we get PAF on the right hand side, we get arachidonic acid metabolites on the left hand side. 05:55 The effects of these take a little while. 05:58 It's not just I'm releasing granules. 06:00 Here, I actually have to activate an enzyme, it has to cleave, I have to get new synthesis. 06:05 So over the course of a couple hours, we're going to see the effects related to now, this membrane phospholipid metabolism. 06:15 Those effects that take minutes to hours are going to include bronchoconstriction. 06:21 And there will be inflammatory cell recruitment as a result of the effects of say, for example, leukotriene B4. 06:28 So we have an immediate effect, we have an intermediate effect. 06:31 And now we also have a longer term effect. 06:34 So at the same time, we're activating these other pathways, we're also activating the cell to make additional cytokines. 06:42 Those cytokines are going to have late effects. 06:44 To hours to even a couple days. 06:47 And they're going to be important for recruiting inflammatory cells and for secondary effects on the epithelial cells that are in the vicinity. 06:58 So the late effects include inflammatory cell recruitment, just as I said. 07:02 They're going to be chemokines and cytokines that will drive and recruit neutrophils, macrophages, eosinophils, for example. 07:11 There will also be a more prolonged effect on vasodilation and edema. 07:16 So the longer term effects of the mast cell degranulation, or the mast cell activation, are going to be prolonged visit dilation and edema. 07:25 As I said, cytokines will increase mucus production in areas such as the airways. 07:32 And there's potential for epithelial injury. 07:34 So some of the inflammatory cells that are coming in are going to themselves release their proteases or release mediators that are going to cause potential epithelial injury. 07:47 So you're thinking to yourself, "Why would I have an immune response like this," "that could potentially be so damaging?" Well, in fact, probably, IgE mediated responses, including the recruitment of eosinophils and cells of that nature, were probably evolutionarily developed, to deal with worms, to ailments and things like that. 08:11 So this is not just to keep the allergist in business. 08:15 There's probably a real reason that this occurred over time.
About the Lecture
The lecture Type I Hypersensitivity Reaction by Richard Mitchell, MD, PhD is from the course Immune-mediated Diseases.
Included Quiz Questions
What type of cells are mainly involved in type IV hypersensitivity reactions?
- T cells
- Mast cells
- Alpha cells
- B lymphocytes
- Macrophages
In IgE-mediated hypersensitivity reactions, mucus production is classified as what type of an effect?
- Late
- Immediate
- Intermediate
- Moderate
- Instantaneous
What causes the immediate effects of IgE-mediated hypersensitivity?
- Allergens cross-linking IgE receptors on mast cells
- Mast cell degranulation releasing arachidonic acid
- Phospholipase A2 breaking down histamine
- Cytokines produced by mast cells
- PAF produced by membrane phospholipids
What causes the intermediate effects of IgE-mediated hypersensitivity?
- Leukotrienes and prostaglandins
- Chemotactic factors
- Eosinophils
- Proteases
- Cytokines
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |