Playlist
Show Playlist
Hide Playlist
Thoracic Injuries
-
Slides ThoracicInjuries Surgery.pdf
-
Download Lecture Overview
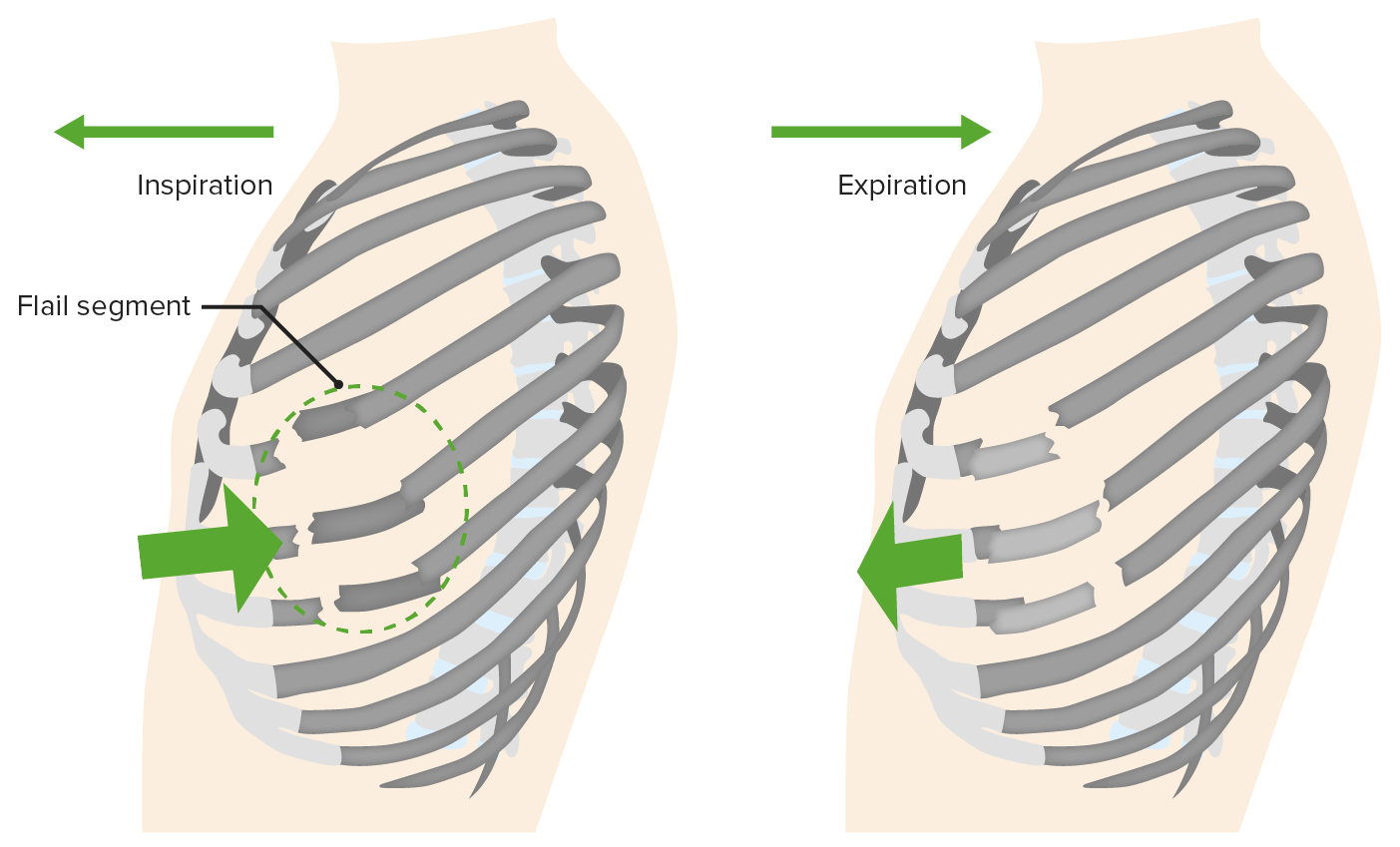
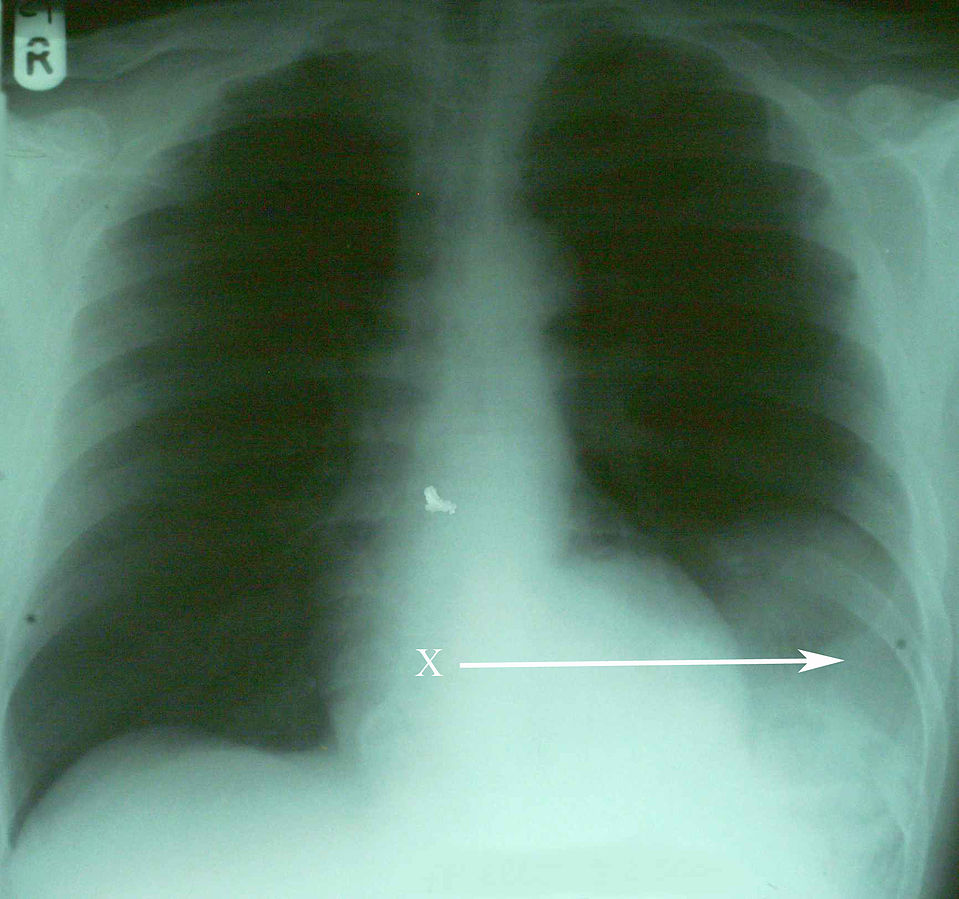
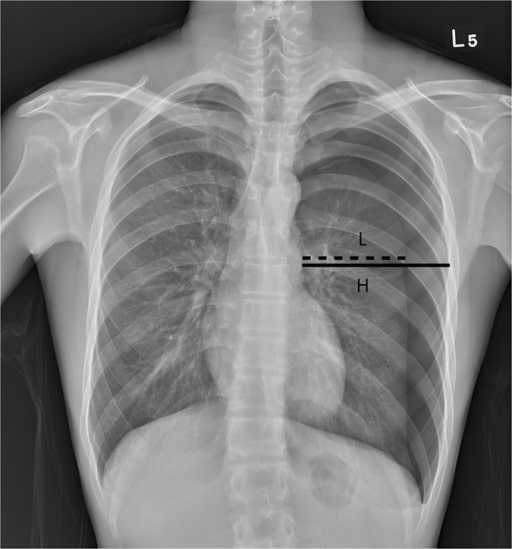
00:01 Thank you for joining me on this discussion of thoracic injury in the section of trauma. 00:07 Just as a reminder, trauma-related principles are extremely high-yields or a common place for questions on USMLE examinations. 00:15 So pay particular attention to the trauma series. 00:19 Let’s start with a clinical scenario. 00:22 You have a patient who is 24 years old. 00:24 He is at a night club and engages in a verbal confrontation with another patron. 00:29 When he exits, unfortunately he is stabbed in the back. 00:33 Emergency medical services are called and rushes to the scene. 00:37 They find a patient who is alert, complains of difficulty breathing. 00:41 The patient is intubated in the field by EMS and arrives at your trauma bay. 00:46 And upon arrival this is what you find. 00:50 Pretty startling. 00:51 What’s going on in your mind? How are you going to manage this patient? Let’s start with a question. 00:58 What’s the next step in management? Remember, many USMLE questions end with this very question. 01:04 What is the next step in management? I’ll give you a second to think about this. 01:10 Of course, ABCs. 01:12 That’s the beginning of every trauma patient. 01:15 Airway, breathing, circulation. 01:18 As you can imagine, with the stab wound to the chest, airway and breathing are particularly important. 01:26 Remember, just because the EMS intubated the patient doesn’t mean that the ET tube is actually in the correct place. 01:34 You must begin with ABCs again and not assume that the patient has a definitive airway. 01:40 Now, do you remember from our initial assessment lecture module how to quickly check if the patient has an intact airway? Of course this doesn’t apply to our patient because he is already intubated. 01:51 I’ll give you a second to think about this. 01:54 That’s right. 01:56 I simply go up to the patient and say, “Hello sir, I’m Dr. Pei. Please tell me your name.” And if your patient was able to tell you their name, you know they have an intact airway and they’re moving air through this conduit. 02:12 Now, let’s get to B. 02:15 Let’s say that you’ve confirmed the ET tube by end-tidal CO2. 02:20 Again, let me repeat that. 02:22 Placement of an ET tube is confirmed by end-tidal CO2, not breath sounds. 02:28 You’ve moved on to B for breathing. 02:30 And as this picture depicts, you don’t hear any breath sounds on the left side where the stab wound was. 02:38 What’s going on in your mind? And what are you going to do next? I’ll give you a second to think about this. 02:46 Of course, it’s time for a chest tube or thoracostomy. 02:51 Don’t get confused. 02:52 This is an ostomy, thoracostomy not a thoracotomy. 02:56 So we put the chest tube in when there are decreased breath sounds. 03:00 And remember, absent or decreased breath sounds in the trauma bay is presumed a pneumothorax. 03:07 You should not have additional studies and do not delay placement of a chest tube particularly if the patient is unstable. 03:16 When presented with this clinical scenario and you don’t hear breath sounds, assume that there is a pneumothorax. 03:22 Of course, there’s always the option of needle decompression. 03:25 Needle decompression is performed in the midclavicular space about the second intercostal space. 03:31 This draws the air out, but sometimes you need a bigger bore chest tube like the one that’s shown in this image. 03:38 After chest tubes are inserted, it’s usually connected to a drainage system. 03:42 In the blue on the left side of the image, that’s what’s called a water seal. 03:47 The water seal prevents direct communication from the intrathoracic component to the atmosphere. 03:54 Now, let’s say you had time to get a chest x-ray. 03:58 Can you see the pneumothorax? That’s right, it’s on the left side. 04:03 Now, where is the pneumothorax on this one? Just for practice. 04:08 I’ll give you a second to take a look at this image. 04:12 That’s right. It’s on the right side. 04:15 Now, special cases where the chest x-ray clearly looks like there is no pneumothorax like the one on the left side of your screen but when you get a cross-sectional CT chest for whatever reason, you actually see that there is a small pneumothorax anteriorly. 04:31 This is not uncommon. 04:32 Remember, small pneumothoraces like this may not be clinically relevant unless the patient is about to undergo positive pressure ventilation. 04:42 For whatever the reason that the patient has a pleural disruption, positive pressure ventilation may actually make this pneumothorax worse. 04:49 So remember, if your patient’s going to the operating room for whatever reason, just keep a close eye on the patient. 04:54 He or she may need a chest tube at some point.
About the Lecture
The lecture Thoracic Injuries by Kevin Pei, MD is from the course Surgery: Trauma.
Included Quiz Questions
A 30-year-old patient is stabbed in the back. The patient is alert but complains of difficulty breathing. The patient is intubated en route to the hospital. When this patient presents to you in the trauma bay, what are your next steps in management?
- Assess airway, breathing, and circulation
- Obtain a chest x-ray and pelvis x-ray
- Assess breathing and circulation
- Obtain CT, ultrasonography, or aortic imaging studies of the chest
- Assess for signs of shock and obtain a blood pressure
A patient is stabbed in the back and presents to you in the trauma bay. How would you quickly assess if the patient has an intact airway?
- Ask the patient to say their name
- Look to see if the patient’s chest is rising and falling with respiration
- Listen over their mouth and nose for breathing sounds
- Perform an upper endoscopy
- Perform a jaw thrust procedure
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |