Playlist
Show Playlist
Hide Playlist
Blunt Abdominal Injuries
-
Slides AbdominalInjuries Surgery.pdf
-
Download Lecture Overview
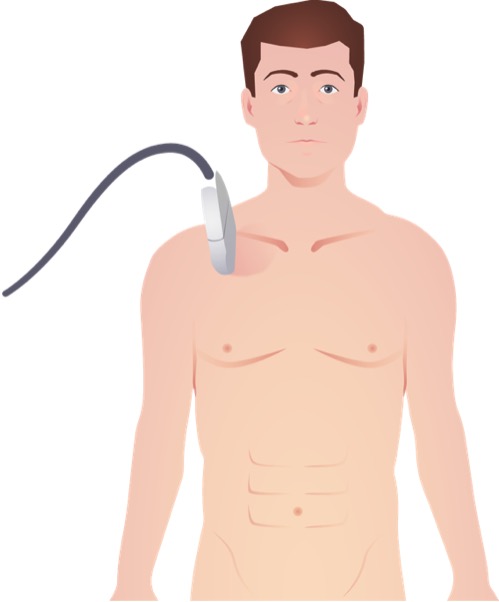
00:01 Now, let’s discuss blunt abdominal injuries. 00:04 Lots of organs are in the abdomen clearly and anything can be injured in a blunt, particularly high-speed motor vehicle accident. 00:11 So we’ll just limit it to the most common and high-yield information. 00:16 We’ll talk about duodenal injuries, liver injuries, spleen injuries, kidney injuries. 00:22 Let’s start with the duodenum. 00:26 Now, in this image, you see a clear classic seat belt sign. 00:31 There was a time that many of us don’t remember where there was only a waist belt when you sat in a car. 00:37 That was actually more dangerous than not having a belt at all because oftentimes the patient had these hyperflexion injuries because their chest and their backs were not belted into the car. 00:48 With the seat belt sign, however, you have to be suspicious that there may be intra-abdominal injury, whatever the viscous or solid injury may be. 00:58 Now, let’s talk about very high-yield topic, a chance fracture. 01:03 A chance fracture is a hyperflexion injury, kind of like when you’re only wearing a waist belt. 01:09 It’s associated with a proximal, usually L1 spine fracture as you see highlighted in this image. 01:16 Now, do you remember what bowel injury might be associated with a chance fracture? These are some classic associations. 01:22 I’ll give you a few moments to think about this. 01:27 That’s right, duodenal injury and small bowel injury, and in fact the pancreas as well. 01:34 Remember, anatomically, that the duodenum is fixed in the retroperitoneum in certain portions. 01:39 The pancreas is completely retroperitoneal. 01:42 These organs abut the upper lumbar lower thoracic spine. 01:46 Therefore, a chance fracture is associated with these injuries. 01:52 Now, here’s an image of a traumatic duodenal perforation. 01:56 It can only be found on exploratory laparotomy or exploration. 02:01 In fact, if your patient has pneumoperitoneum on work-up during the trauma, you should take the patient to the operating room as your next step in management. 02:11 Depending on the severity of the duodenal injury, multiple surgeries can be performed, either primary repair or some sort of a bypass surgery. 02:19 What I mean by bypass surgery is how the stomach juice is drained into a small bowel by making another connection, leave lots of drains around the duodenum and let it heal. 02:28 Another common scenario you may encounter on examinations is a young patient who is riding their bicycle or an ATV. 02:36 They may flip over and hit their upper abdomen on the handlebar. 02:40 This is called the handlebar injury. 02:42 Usually, these patients don’t present right away. 02:45 They pick themselves up, dust themselves off and just keep going. 02:48 But days later, they may come in with nausea, vomiting, abdominal pain. 02:55 And if you have a suspicion of a duodenal injury, you might get an upper GI swallow study which will show a gastric outlet obstruction. 03:04 This is likely because the handlebar injury when they made impact cause swelling or injury to the duodenum. 03:11 Subsequent edema because of the injury has now caused a gastric outlet obstruction. 03:17 Very importantly, your next step in management should not be surgery. 03:21 Many, many of these patients resolve completely with a trial of non-operative management. 03:26 So that’s what you should choose. 03:28 Now, let’s move on to the liver. 03:33 Here, on this cross-sectional image, you can see a pre-macerated liver in the right lobe. 03:42 But despite its appearance, we’re quite successful on non-operative management. 03:47 Why is non-operative management so important in liver? Well, unlike some other organs like the spleen, you can’t remove the liver. 03:55 Therefore, if the patient is stable and responsive to blood transfusion, try non-operative management. 04:01 Particularly if there is a blush or active bleeding, you can try IR embolization. 04:07 However, if your patient is hypotensive and deteriorating, that’s not a patient that goes to the interventional suite or tries non-operative management. 04:16 Always choose surgery in exploratory laparotomy. 04:19 Pack the liver and depending on the actual injury, there are multiple mechanisms to stop bleeding. 04:26 It’s likely to be beyond the scope of the USMLE examination. 04:32 Now, let’s move on to spleen, a favorite topic. 04:37 The spleen of course is in the left upper quadrant of your abdomen. 04:40 On this cross-sectional image of the abdomen and pelvis, you not only see a major hematoma laceration of the spleen in the left upper quadrant, you also see a fair amount of intraperitoneal fluid around the liver as well as around the spleen. 04:54 Remember when I made a comment that when you do a FAST examination and you see blood or fluid in a certain quadrant doesn’t always mean that the injury was in that quadrant. 05:03 In this scenario had you done a right upper quadrant ultrasound, you would’ve found blood in the hepatorenal space and yet the injury is demonstrated by the CT abdomen and pelvis was actually a spleen injury. 05:15 Just as a side up, remember, any time you see an image of the patient, it’s presumed that the patient was hemodynamically stable. 05:22 Because again, a very important high-yield fact is you never want to take an unstable patient to the radiology suite. 05:31 So, how do we manage spleen injuries? Well, for hemodynamically stable patients, we have had great success with non-operative management and we continue pushing the envelope for even higher grade splenic injuries. 05:45 So splenic salvage rates are incredibly good. 05:49 This is what you should offer your patient if they’re stable. 05:53 If, however, the patient is hypotensive like our patient and has a positive FAST, your next step in management should be exploratory laparotomy and in this situation a splenectomy. 06:08 Now, I’d like to pose a question. 06:10 After splenectomy, vaccines are needed. 06:13 I’ll give you that. 06:14 But do you know what the vaccines are? I’ll give you a second to think about this. 06:22 Before I give you the answer, remember vaccinations are most ideal two weeks prior to surgery, clearly not possible in a trauma patient. 06:29 Therefore, practically speaking, we give it right before discharge. 06:34 Vaccinations are again encapsulated organisms. 06:37 I hope you got these answers. 06:39 The specific organisms that we’re trying to cover is Haemophilus influenzae, Streptococcus, and Neisseria meningitidis also known as meningococcus. 06:52 We’ve discussed spleen, let’s move on to kidney. 06:58 Kidney injury noted here in a coronal section is usually found on the CT scan. 07:03 Unfortunately, neither hematuria or flank pain or necessarily the mechanism of injury usually gives you enough information. 07:11 Fortunately, the vast majority of the time, unless it’s a hilar avulsion, doesn’t result in hemodynamic instability and can be treated non-operatively. 07:21 Remember, sometimes observation alone is okay for patients who are hemodynamically stable. 07:26 We oftentimes contact our interventional radiology colleagues to give the patient a shot of contrast to see whether or not there’s active bleeding and a potential for embolization. 07:35 Remember, though, embolization of the kidney can cause ischemia. 07:40 Sometimes urologists actually need to place stents because your urethral system or the kidney itself may be obstructed with a clot. 07:47 This can lead to renal failure or acute kidney injury. 07:51 Typically, given this likelihood of bleeding, we put these patients in the intensive care unit for close monitoring and what’s called a serial H and H. 07:59 We get a blood draw and look at the hemoglobin and hematocrit every few hours. 08:04 Unfortunately, in a small patient population, nephrectomy is necessary, but make sure you check that there’s another kidney first and it’s functional prior to removing the kidney. 08:16 In the emergency situations with massive hemorrhage, you do what you have to do.
About the Lecture
The lecture Blunt Abdominal Injuries by Kevin Pei, MD is from the course Surgery: Trauma. It contains the following chapters:
- Blunt Abdominal Injuries
- Liver
- Spleen
- Kidney
Included Quiz Questions
Which of the following describes a Chance fracture?
- Flexion injury of the spine
- Vertical fracture through the anterior elements of the vertebra
- Hyperextension injury of the spine
- Transverse fracture through the anterior elements of the vertebra
- A fracture through the anterior portion of the vertebral body
Chance fractures most commonly occur at what region of the spine?
- Upper lumbar spine
- Lower thoracic spine
- Lower lumbar spine
- Upper thoracic spine
- Cervical spine
What is the best time for administering vaccination in a trauma patient who had a splenic injury requiring splenectomy?
- Before discharge
- 2 weeks after discharge
- After surgery
- Immediately on presentation
- Before starting the splenectomy
After splenectomy, a vaccine against which of the following organisms is required?
- Neisseria meningitidis
- Eikenella corrodens
- Fusobacterium nucleatum
- Actinomyces naeslundii
- Streptococcus sanguinis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Dr. Pei has a lot of knowledge about surgery and he is able to transmit it to the students. also he focus on high yield question and that always important.