Playlist
Show Playlist
Hide Playlist
Toxic Shock Syndrome (TSS) in Children
-
Slides toxicshock Pediatrics.pdf
-
Download Lecture Overview
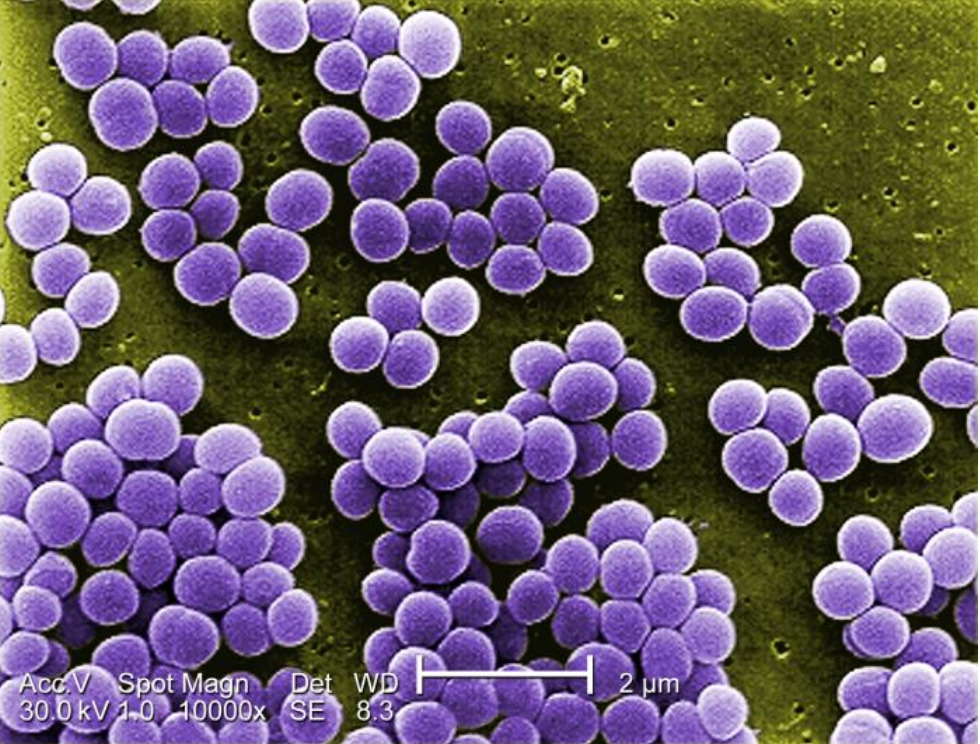
00:00 In this lecture, we’re going to discuss Toxic Shock. So, toxic shock is a distributive shock caused by an endotoxin released by bacteria. Most commonly, this is <i>Staph aureus</i>, which releases the toxin TSST-1 or group A beta-hemolytic strep. Basically, the bacterial toxin causes cell death, and toxins act as a super-energen. They overstimulate the immune system and cause a release of cytokines that causes vascular distributional problems such as dilatation and increased leakiness. Patients generally have systemic effects, typically from a small or insignificant seeming source. About half of cases are from tampons. So, women who leave a tampon in too long or use a hyperabsorbent tampon can have a <i>Staph</i> that colonizes that tampon and grows. The toxin is then released from where those <i>Staph</i> are growing, get into the systemic system and cause their effect. So, there are certain criteria for diagnosing toxic shock. Patients must have fever, they should have a blood pressure, which is below the 5th percentile and they should have a blanching erythematous rash or erythroderma, which is a diffuse red rash. Generally, patients will have involvement of 3 organ systems. This may be the GI system, they present with vomiting; they may develop a myositis and have an increased CPK, this can present as sore muscles. They often develop mucous membrane hyperemia generally of the eye, the mouth or the genitals, and they may develop renal dysfunction, and thus we can detect an increased creatinine on lab work. 02:00 Patients may develop a hepatitis or bumped LFTs, they often develop a thrombocytopenia or a low platelet count, and they can certainly have altered mental status. One thing that we find later in toxic shock that patients should be aware of is peeling hands and feet. Sometimes that clinches the diagnosis when we weren’t really sure earlier. There are other potential causes of patients presenting in this way that we should think about when we see patients. One is a systemic allergic reaction. Patients may develop serum sickness either from antibody use like horse antibodies for certain antivenoms or for example from amoxicillin. Scarlet fever can certainly create many of these symptoms especially the peeling of the hands and feet afterwards. There are a variety of tick-borne illnesses such as Rocky Mountain Spotted Fever or ehrlichia that can present similarly. Measles might be mistaken but measles does have the classic finding of conjunctivitis followed by the head-to-foot rash, and meningitis or encephalitis may look similar to this. Basically, these patients are very, very sick. So, if we see patients like this, we have to worry about disseminated intravascular coagulation. So, typically, we’re going to get a broad spectrum of labs to try and figure out what’s going on. This includes the CBC, coagulation studies like PT, PTT, and INR. We should get a chem-7 to look for the bumped creatinine in these patients. We should check a CPK because that will often cleanse the diagnosis, and we should look for bumped LFTs. We usually get a blood culture as well, because especially for group A <i>Strep</i> a huge percentage of these patients will have a positive blood culture and be bacteremic. 03:51 This is less likely in patients who have tampons or have a small abscess somewhere that is the source of the toxin. Also, if we do have an abscess, it’s useful to do an I&D and drain that and get a culture because it’s nice to know what antibiotic we should be using to target this particular bacteria. What’s critical in patients with toxic shock is we have to examine all post pubertal females immediately and remove possible retained tampon, even if there’s no history of a retained tampon. It absolutely happens that young women can forget that they left their tampon in, or it can go farther up in and they’ve lost it. So, you should always do a complete vaginal exam on all post puberty females who present with toxic shock. It’s important to treat all sources of infection: strep throat, drain any abscesses, etc., because if we don’t kill the bacteria that’s causing the toxic shock, the toxic shock will continue. We provide supportive care in the forms of IV boluses, dopamine therapy for recalcitrant or hard to treat hypotension, and of course airway support as well. In severe cases, some people use IVIg. IVIg acts as a competitive inhibitor for the immune system to fight off those extra FC regions as opposed to attacking the body. It may help a little bit, it’s not clear, but we certainly use it in severe cases. So, let’s talk about management of patients and if they come in in toxic shock, what antibiotics we use. 05:30 There’s a lot of different style practices but generally speaking, we tend to double or even triple cover for gram positives under these circumstances, and there’s an interesting reason why. 05:42 First off, most practitioners will start vancomycin. This is because a small percentage of bacteria such as MRSA may be resistant to other forms of antibiotics. Toxic shock patients are severely ill. We can’t afford to have even the slightest chance of a resistant organism because if we aren’t treating it, they’re going to get worse. So, we routinely give vancomycin for these patients. 06:11 However, vancomycin does not block the ribosome of the bacteria; clindamycin does. So, many practitioners will add clindamycin because of the theory that it will reduce toxin production by blocking the ribosomal activity of that particular bacteria. Remember, the toxin is really the part that’s causing the problem. So, sometimes people will do vancomycin and clindamycin. In addition, patients may be given a first generation cephalosporin, all 3. Now, the reason for the first generation cephalosporin is that it tends to kill things faster. The first generation cephalosporin here is bactericidal rather than bacteriostatic. Thus, because this patient is critically ill, we may give all 3 approaching different things: the vancomycin for resistant forms, the clindamycin for stopping toxin production and the first generation cephalosporin for killing these bacteria faster. Eventually, we need to transition to oral therapy and typically we will transition to either cephalexin, which is an oral first generation cephalosporin, or oral clindamycin, depending on what the organism is that has grown or what we might empirically think is most likely given the clinical circumstances of the patient. So, it’s important to prevent further toxic shock episodes and especially in women, further avoidance of hyperabsorbing tampons is advised. In fact, some providers recommend no tampons ever again for those women. The concern is is that the vagina may continue to harbour that organism in small numbers that's essentially just waiting for a tampon to grow up on. So, avoidance of tampons in these patients is critical certainly until they can be cleared for further tampon use and sometimes that’s not for years. I usually refer them to an obstetrician and gynecologist for further advice regarding this care. Vaginal colonization is important and so we have to prevent that from happening, and remember, tampon use is generally avoided in these patients. That’s all I have to talk to you today about Toxic Shock in Children. Thanks for your time.
About the Lecture
The lecture Toxic Shock Syndrome (TSS) in Children by Brian Alverson, MD is from the course Pediatric Infectious Diseases. It contains the following chapters:
- Pathology of Toxic Shock
- Diagnosis of Toxic Shock
- Management of Toxic Shock
Included Quiz Questions
Which of the following is a treatment option for toxic shock syndrome?
- All of the given therapies are indicated.
- Prompt removal of the source of infection (abscess, retained tampon, etc.)
- Clindamycin
- Vancomycin
- Cefazolin
Which of the following is a common cause of toxic shock syndrome?
- Superabsorbent tampons
- Intrauterine devices
- Sanitary pads
- Tight undergarments
- Genital piercing
Which of the following organisms is known to cause toxic shock like syndrome?
- Group A beta hemolytic streptococcus
- Group B hemolytic streptococcus
- E. coli
- Candida
- Pseudomonas
Which of the following drugs is thought to decrease toxin production in toxic shock syndrome?
- Clindamycin
- IV Ig
- Vancomycin
- Cefazolin
- Tetracycline
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I particularly liked the focus on understanding and recognising the disease.