Playlist
Show Playlist
Hide Playlist
Testing on Patients and Therapy – Heart Failure
-
Slides 08 Cardiology Alpert.pdf
-
Reference List Cardiology.pdf
-
Download Lecture Overview
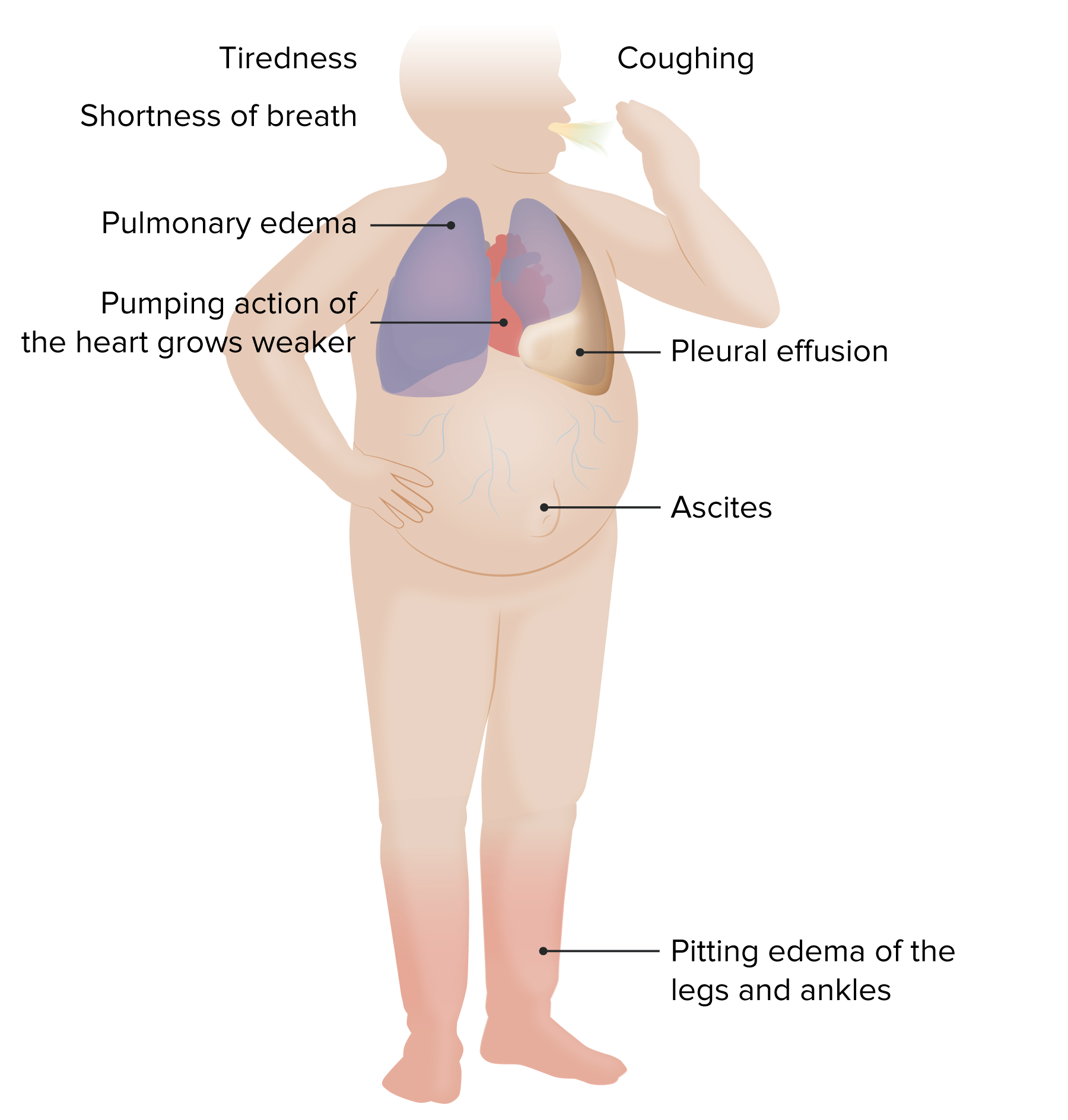
00:00 So, of course, we’re going to do some tests to confirm our clinical impression. We’ve had the history, oh, this suggest heart failure, the patient is short of breath, they have peripheral edema. Oh, we listen to the heart and we hear an extra sound, the S3 gallop. 00:14 Okay, we’re now pretty sure the patient has heart failure, then we do a chest x-ray. 00:18 You can see the two examples here. The one… on the one side is normal and the one on the other side shows an enlarged heart. Sometimes we will even see evidence of fluid in the lungs. Pretty obvious on this chest x-ray, this is called pulmonary edema. The left ventricle has failed significantly and what we see is fluid throughout the lungs. 00:39 And of course, this patient is very short of breath. They might be breathing at 30 or 40 times a minute. Normal is about 12, 13, 14 times a minute and they may… you may actually hear gurgling from this fluid that’s collecting in the small alveolar sacs in the lung and being transmitted into the… into the bigger bronchial tubes. This can drop the oxygen saturation in the blood, can lead to fatal arrhythmias and people can die from this. And this… this is a medical emergency that requires urgent therapy. 01:14 And here is a chest x-ray showing a variety of findings of a little less serious heart failure. One can see edema in the lymphatics, so called curly lines. One can see fluid collecting in the pleura, you can see in the little angle there where the heart meets the chest that there’s a little sort of rounded area. That’s actually fluid in the pleural space, the space that surrounds the lungs. There’s a variety of other findings that the radiologist will often call you up and say, “Your patient has heart failure.” We often do an echocardiogram to see how bad the heart failure is. For example, is it left ventricular? Is it right ventricular? Is it very advanced? Does the ejection fraction, that is the percentage of blood squeezed out by the heart very low? Or is it only modestly reduced? This is an echocardiogram from a patient with a very advanced heart failure. The left ventricle is markedly dilated, we don’t see the film with it, but I’m sure if we saw the film, instead of the ventricle squeezing normally like this, it’s doing this. Hardly squeezing at all and you can see also, in this echo, the left ventricle is enlarged. So, this is a patient with longstanding heart failure. 02:31 So, let’s talk a little bit about treatment. Clearly, treatment goals are to reduce the edema, to reduce the excess fluid volume and to make the patient much more comfortable and able to have full activity. You’d also like to increase the pumping ability of the heart. Sometimes, if it’s, for example, in the patient we talked about in the last lecture, somebody with aortic stenosis, taking away the stenotic valve and putting in a good valve allows the ventricle to recover. In other settings, if it’s due to severe ischemia - lack of blood flow in the heart, coronary bypass or angioplasty may improve the blood flow on the heart and may, not always, but may improve the function of the ventricle and again, lead to resolution of symptoms. And there’s a variety of drugs that help increase the removal of fluid from the body. For example, diuretics that increase renal excretion of water and salt will reduce the excess volume of salt and water in the body and often lead to marked improvement in the symptoms. 03:38 Patients with heart failure, particularly new heart failure, require hospitalization. 03:43 They require a number of tests to determine why they're on heart failure and they also require a number of drugs that are used to improve, if possible, the function of the heart and to decrease the work of the heart and to increase fluid and salt excretion. 04:01 And what you do… this step diagram is a complicated one. I’m not anticipating that anybody needs to learn this right away, but it shows you as the heart failure increases, the aggressiveness of our therapy increases. So, in the beginning, we use ACE inhibitors that is they vasodilate the arterioles, they decrease the blood pressure a bit and they decrease the work of the heart. In a sense, what we’re trying to do is rest the heart. Make the heart’s job, the left ventricle’s job a little easier, but as you go along, there’s a variety of other interventions that are used. Both improving blood flow, for example, with angioplasty. We also use drugs that rest the heart a little bit by decreasing the heart rate - beta blockers. And then eventually, you may even progress to devices that increase the pumping ability of the heart while you’re getting ready to do something more aggressive. For example, change a heart valve or even in the most severe stages, do a heart transplant - give the patient a new heart. 05:09 It‘s important that patients have lifestyle changes, particularly with the milder forms of heart failure because what we’re trying to do is prevent heart failure from progressing. 05:20 So, what are those lifestyle changes? Clearly, somebody who’s obese, you’ve got a lot of extra weight around. If you have a big belly that has 40 or 50 pounds of extra weight, it’s like you’re carrying a 40 or 50 pound knapsack on your back and you’re asking the heart to do that extra work. You can imagine, that’s a bad idea. So, dieting and reduction of obesity is important. Number two, cutting back on salt because the more salt you take in, the compensatory mechanisms of the body hold on to that salt and of course, increase blood volume. So, restriction of salt. It turns out that regular, particularly in the beginning, supervised exercise or physical activity actually improve the whole cardiovascular system and enable patients to do more work with the same cardiac output that they had before. So, and of course, stopping things like cigarette smoking which are damaging to the blood vessels and which can cause acceleration of atherosclerosis, just as in we talked about in patients with a heart attack or coronary artery disease. There’s a whole variety of lifestyle changes and often, these are integrated between the cardiologist and a good cardiac rehabilitation program. 06:36 Medication management is. 06:38 Tailored to the type of heart failure that a patient has, whether they have heart failure with preserved ejection fraction as we already heard called half HFpEF, or whether the heart failure patient has a reduced ejection fraction, so called HFrEF. 06:54 And of course medication management is tailored to the patient's symptoms and signs. 07:00 If a patient has volume overload with dyspnea or peripheral edema, of course they need diuresis, usually with a loop diuretic to remove excess fluid. 07:10 For patients with a compelling indication for a. 07:13 Specific type of anti-hypertensive medication for example, if a patient has diabetes or chronic kidney disease, then an ACE inhibitor or an energy tension receptor blocker should used before starting HFpEF specific therapies such as mineral coracoid blockers or ACL two inhibitors. 07:33 Of course, you have to look carefully at the patient's renal function. 07:37 If it is quite impaired, then ACE inhibitors or ARB's are contraindicated because they might make the renal failure worse for patients without diabetes, then heart failure, specific medications are indicated. 07:52 The next step is to add a sodium and glucose co transporter to inhibitor, SGLT2 inhibitor, I like to call them flows arms because that's part of their generic name or of course, and or a mineral, a court acquired receptor antagonist. 08:10 SGLT2 inhibitors are medications like empagliflozin and or dapagliflozin. 08:16 And you notice the term flows in in the middle of those terms, a mineral, a quarter receptor antagonist or a mineral or MRA, as it's often known, such as spironolactone or eplerenone . 08:27 Known can be. Added if the. 08:29 Patient has a systolic blood pressure below 100 or symptoms of. 08:33 Hypertension, such as dizziness. 08:35 or other orthostatic Symptoms. 08:37 Then other antihypertensive drugs should be decreased or discontinued. 08:41 Otherwise you're liable to have severe symptomatic hypertension. 08:42 Otherwise you're liable to have severe symptomatic hypertension. 08:45 That's the primary therapies for heart failure with reduced ejection fraction are ACE inhibitors. 08:50 Angiotensin receptor. 08:52 Angiotensin receptor blockers called ARB's or the combination medication of an angiotensin receptor blocker and a neprilysin inhibitor put together are called and ANRI`s and the neprilysin inhibitor, is known as sacubitril and it's a blocker of the break down enzymes for atrial peptides. 09:13 enzymes for atrial peptides. 09:15 Thus the ANRI drug is a double vasodilator. 09:19 And again, you have to be careful about the blood pressure beta blockers should be added if there are no contraindications and the specific three that have been demonstrated. 09:29 To benefit patients with heart failure are Carvedilol, Bisoprolol and Extended-release metoprolol succinate. If patients have contraindications to any of the renin angiotensin systems and tarragon is. 09:42 An alternative is hydrolyzed impressive long acting nitrates, a typical contraindication to the. 09:48 Renin angiotensin system. 09:49 Antagonist is advanced renal failure because these drugs could increase the level of renal insufficiency In patients who still have symptomatic heart failure. 10:00 Secondary therapies may be added in. 10:03 Addition to the initial medivations. 10:05 And there's considerable current debate about the order that we give these drugs, which one should be first. 10:11 Which one second, and that. 10:13 Is the subject of current ongoing heart failure research. 10:17 These include the additional drugs These include the additional drugs that could be used, for example, mineral of course called receptor blockers. 10:24 As we've already said, sporran lack tone in a player known on or SLGT2 inhibitors Just mentioned in certain symptomatic patients. 10:34 We may need to consider Cardiac risk synchronization therapy done with a special Cardiac risk synchronization therapy done with a special form of pacemaker that also stimulates the left ventricle as well as the right ventricle or transcatheter mitral valve replacement repair, for example, clipping a loose mitral leaflet, this allowing for severe mitral regurgitation. 10:55 You clipped that to another a leaflet and thereby you decrease the amount of mitral further secondary therapies. 11:04 Newer medications include Vericiguat or Ivabradine. 11:09 So Vericiguat is indicated for patients with New York Heart Association class two to four heart failure with. 11:15 An ejection Fraction less than 45% who were either hospitalized in the last six months or require outpatient IV diuretics. 11:24 Ivabradine is a very interesting new class of medication called hyper polarization activated cyclic nucleotide gated channel blockers, what they do is they actually decrease the rate at which the sodium channel leaks. 11:39 And that results in slowing of the Heard rate It's indicated for patients with an ejection fraction. 11:46 Of 35% or less who are in sinus rhythm with arresting heart rate, that's at least 70 beats per minute. 11:52 If beta blockers are either contraindicated or have caused problems, then you can substitute a slowing drug using Ivabradine. 12:00 Digoxin can be added to patients with end stage heart failure who are not doing well despite optimal other pharmacologic therapies as well as cardiac synchronous zation therapy. 12:11 Lastly, mechanical circulatory support devices such as left ventricular bypass pumps and inferiority balloons and even cardiac transplantation may be considered in so highly selected patients with refractory heart failure. 12:28 And again, there’s patient counseling. We already talked about the lifestyle. Alcohol is a depressant on the heart so we want patients drinking as little as possible. Smoking has to stop, we want weight control, we want regular exercise. All of the lifestyle things, again, repeated to work with the medicines what we’re giving or to work with the interventions. 12:52 For example, opening up a coronary artery or replacing a heart valve. 12:57 And further patient counseling, of course, involves the medications. Are the patients taking the medications? And are they taking them regularly and as appropriately prescribed? This is a huge problem. In the United States, many patients fail to take their medications. 13:12 If there are surgical or catheter interventions, what these contain and what they can do and what the potential complications are; one wants to reduce stress in the patient’s life, one wants the patient to keep track of symptoms. Are they getting better, are they getting worse, is there weight gaining all of a sudden because of a marked increase in fluid retention? And of course, we would like patients to not overdulge in fluid intake and certainly, come for follow up visits with the doctor or the nurse clinician in order for us to monitor how things are going with therapy and if we have to make further adjustments in therapy. So, in conclusion, heart failure is a growth industry particularly in older individuals. It’s caused by many diseases, but in particular, by atherosclerotic heart disease that causes damage to the left ventricle. Again, left ventricular systolic heart failure is the commonest. The left ventricle doesn’t squeeze as well and the commonest cause of that, ischemic heart disease. 14:13 Prevention, of course, is better than cure. I don’t have to tell you that. And how do we prevent that? By controlling atherosclerotic risk factors before they put the patient in the heart failure situation. Of course, there’s a whole variety of diagnostic test that we use when the patient presents with heart failure, but remember, the clue is in the patient’s symptoms, with confirmation by the exam and then we do some sophisticated tests to see what’s the cause of the heart failure and how severe is the ventricular damage and then we introduce a whole variety of therapies, both drugs and even some of the newer device therapies. For example, we can open up blood vessels and even in extreme cases, we can take over with little pumps for the heart while we’re trying to get it to respond and come back to normal. And of course, then we’re going to have to do lifestyle changes. There’s a new pacing protocol with a special pacemaker that, in some selected patients, can improve the pumping of the heart. 15:18 All of these are fairly extreme things done right at the end. And again, we talked about the fact that there’s a lot of technology here. But, the best deal is to stop the heart failure before it starts with reduction in risk factors or identifying it early and getting all of those things including the lifestyle changes implemented before the patient progresses to a point that they need things like biventricular pacing and heart lung machines and so forth. 15:48 Thank you for listening to this lecture. I look forward to seeing you with the next one.
About the Lecture
The lecture Testing on Patients and Therapy – Heart Failure by Joseph Alpert, MD is from the course Cardiac Diseases.
Included Quiz Questions
Which of the following studies is the most appropriate to provide an initial diagnosis of pulmonary edema in a patient with known left ventricular failure?
- Chest X-ray
- Nuclear heart scan
- Electrocardiogram (EKG)
- Echocardiogram
- Central venous pressure
Which drug is not typically used in the therapy of heart failure?
- Glucocorticoids
- Angiotensin converting enzyme inhibitor (ACEI)
- Beta blocker
- Diuretics
- Statins
Which of the following is not considered a compensating neurohormonal system in heart failure?
- Parasympathetic nervous system
- Renin-angiotensin-aldosterone system
- Sympathetic nervous system
- Anti-diuretic hormone
- Vasoactive substances
Which of the following is not part of the initial combination therapy for patients with heart failure with reduced ejection fraction?
- Clonidine
- Metolazone
- Carvedilol
- Losartan
- Furosemide
Which of the medical treatments is added in the treatment of heart failure with prominent symptoms?
- Inotropes
- Diuretics
- Angiotensin receptor blockers
- Beta blockers
- Angiotensin-converting enzyme inhibitors
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
4 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Professor Joseph Albert is awesome. The lectures are super elaborated, and every video has a lot of relevant questions. He is one of your best teachers.
a very global and complete series about heart failure lectured by a very good professor
I really like it, was the perfect words and way to use them
Explained everything in simple terms and I finally understand based on previous lectures and this one why we would use such drugs and when. Maybe more details into the mechanism (extra lecture) on such medications. I wished there were explanations on the questions. I'm not quite sure why aspirin would not be used if it could treat coagulating factors.