Playlist
Show Playlist
Hide Playlist
Testicular Torsion: Examination & Management
-
Emergency Medicine Bord Torsion.pdf
-
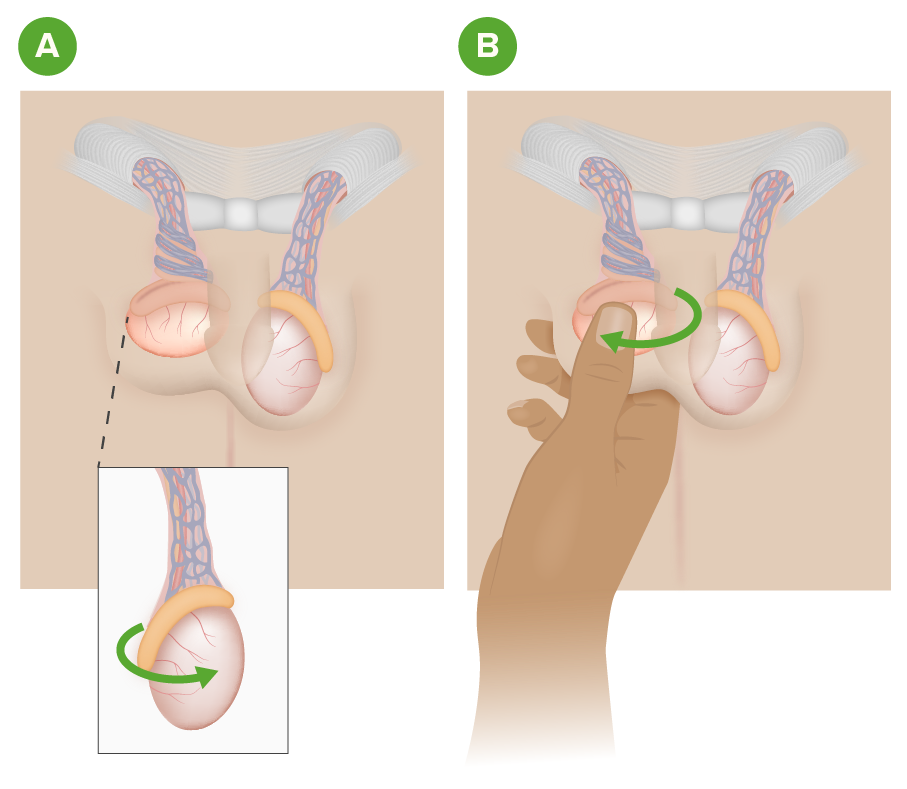
Download Lecture Overview
00:01 Now, what are you gonna see on your physical exam? An absent cremasteric reflex is one of the big diagnostic features here. 00:09 So what that basically means is that you stroke the inner thigh of the patient and what should happen in a normal patient is the testicles should elevate. 00:17 In a patient who has an absent cremasteric reflex, you would do that maneuver and the testicle wouldn’t move at all. 00:23 You also might see a swollen and tender testicle. 00:28 The testicle may be high riding, so it might be located in a higher position than normal for the patient. 00:33 The testicle may be in a transverse lie, so as you could see in this picture, the testicle sort of has turned on its side rather than being in an up and down position, and it’s important to remember that whenever you perform a genital urinary exam whether it be on a woman or a man, that you have a chaperone in the room with you. 00:52 Now, our differential diagnosis. 00:56 One of the things that can present very similarly is testicular appendix torsion. 01:01 On the testicle, there is a small piece that’s called a testicular appendix, and this as well can twist upon its blood supply. 01:09 While it’s helpful to know that, that’s not something that is a big surgical emergency. 01:14 That’s something that generally can be treated conservatively, and with pain medications, and does not have any effect or implications for fertility in the future. 01:23 Epididymitis is the other big thing on our differential diagnosis here. 01:27 Epididymitis can present very similarly to testicular torsion, and can have a similar kind of an exam. 01:34 In epididymitis, the cremasteric reflex should be present. 01:37 So that’s one of the big distinguishing features. 01:40 In epididymitis also, the testicle may just be present in a posterior portion and the testicles should also be in the normal lie, it shouldn’t be turned in any way. 01:49 A hernia can present in this way with pain and swelling in the testicular area and in the groin area. 01:56 Patients may have had trauma. 01:58 There may be a tumor in that area, as well as a hydrocele which is water or fluid around the testicle. 02:06 So how do we evaluate for this? Firstly, we can do a urinalysis and a urinalysis helps you rule out other processes. 02:15 So the urinalysis being infected can potentially point you in the direction of epididymitis or a prostatitis kind of a picture. 02:22 With the urinalysis, if you’re worried about epididymitis, you can also send off gonorrhea and chlamydia testing on the urine. 02:30 And then you wanna do a scrotal ultrasound. 02:33 This is one of those things where you wanna make sure you do this on almost all patients who are coming in with testicular pain and swelling, and the main reason that you’re doing it is to rule out testicular torsion. 02:45 It might be that the patient has epididymitis. 02:47 It might be that there is a hydrocele or a hernia, but you wanna rule out the highest thing or the thing that has the most serious implications moving down the line, and ultrasound is your test here. 02:58 Ultrasound will show a hypoechoic enlarged testicle. 03:02 It will show that there’s not good blood flow to that testicle. 03:05 It’s important to note that there are false negatives as well as false positives associated with this test. 03:11 So while it’s the test of choice, you wanna know that it has certain limitations. 03:16 So what are those limitations? So you can have false negatives early in the disease course. 03:22 So early in this disease process, it might look like that the flow is normal. 03:26 It might also depend on the degree of twisting, so if the testicle isn’t twisted full 180/360 degrees, then the blood flow might still be present a little bit. 03:39 And the other thing to remember is that sometimes patients can have intermittent torsion, so torsion that comes and goes, and all of those can make the ultrasound look potentially normal, so that’s a false negative ultrasound. 03:51 There are also some false positive ultrasounds. 03:54 In prepubertal patients, 50% of them have decreased or absent testicular blood flow at baseline. 04:02 So for those patients, the ultrasound may look positive, so it might look like there is no blood flow to that testicle but that’s just their normal state at that time in their development, so that will be a false positive ultrasound. 04:17 So what do we do for patients with testicular torsion? We wanna get an urgent urologic consultation. 04:24 For patients with significant concern, so the patient who comes in and the testicle looks swollen, the pain started suddenly, the patient is very uncomfortable, the testicle is in an abnormal lie, there’s an absent cremasteric reflex, any of those things that really point you in that direction, go ahead and get that consultation prior to imaging. 04:45 The other thing that we can do in the Emergency Department is we can do manual detorsion and what that means is that we are going to externally attempt to rotate that testicle back on its blood supply, so it’s restored. 05:02 Now, when we’re doing manual detorsion, the classic thing and the classic way you wanna do it is you wanna do it in opening the book, so it’s basically that you’re rotating the testicle externally almost, so it’s away from the midline. 05:14 You may need to actually twist the testicle more than 360 degrees though depending on the amount of twisting. 05:21 It’s important to remember RAPID diagnosis and treatment is key. 05:26 The longer the time goes on from when this condition develops to when it’s treated, the worse outcomes the patient can have.
About the Lecture
The lecture Testicular Torsion: Examination & Management by Sharon Bord, MD is from the course Abdominal and Genitourinary Emergencies.
Included Quiz Questions
What is the cremasteric reflex?
- Elevation of the ipsilateral testicle upon stroking of inner thigh
- Swelling of the testicle from fluid extravasation
- Bell-clapper deformity in the scrotum
- Engorgement of scrotal sac
- Depression of the scrotal sac upon stroking ipsilateral thigh
What imaging modality is recommended in all patients complaining of testicular pain?
- Scrotal ultrasound
- MRI
- CT scan
- Abdominal ultrasound
- Plain film x-ray
Which age group often has a false positive test for testicular torsion on scrotal ultrasound with doppler blood flow?
- Prepubertal
- Infant to toddler
- Pubertal
- Reproductive
- Elderly
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |