Playlist
Show Playlist
Hide Playlist
Unstable Tachyarrhythmia and Rhythm Identification
-
Emergency Medicine Tachyarrhythmia.pdf
-
Download Lecture Overview
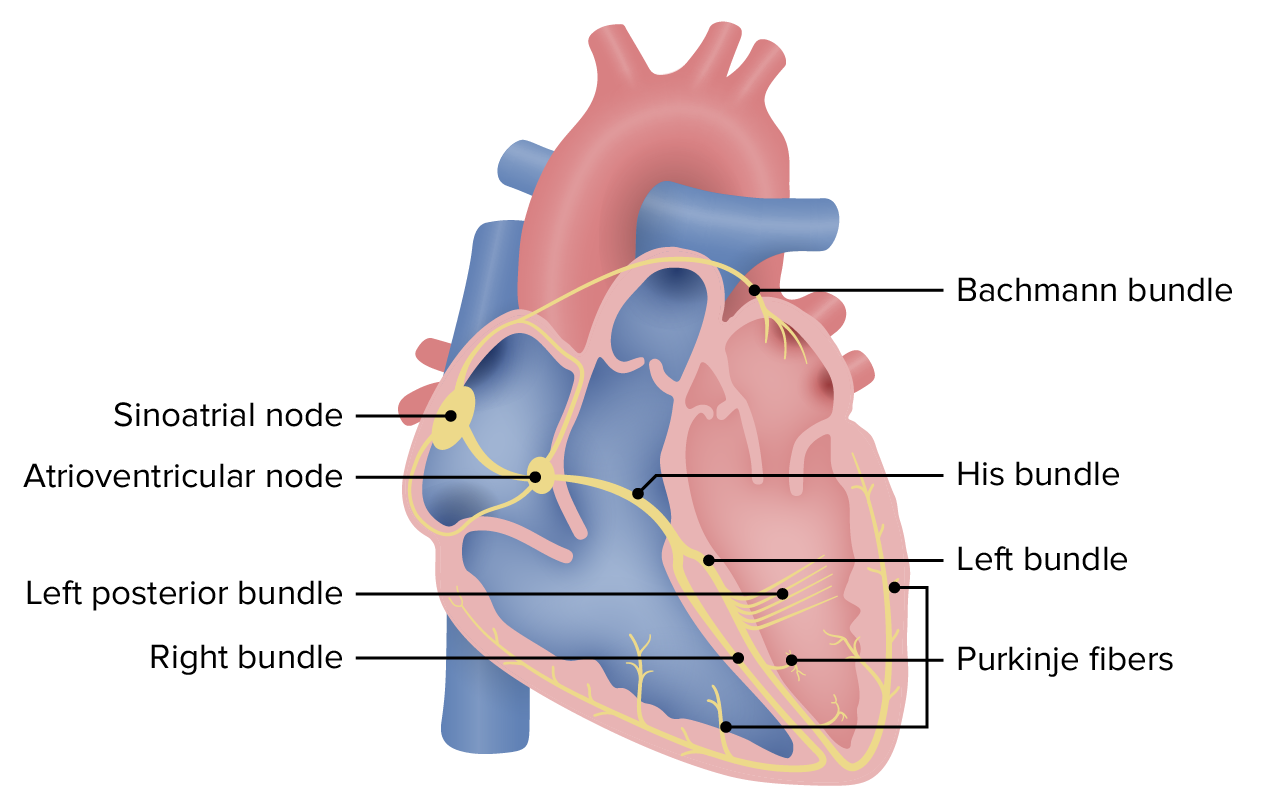
00:01 Hello. In this lecture we're gonna talk about common tachyarrhythmias. So, what is a tachyarrhythmia? Very simply, to have a tachyarrhythmia, you must be first tachycardic, meaning your ventricular rate must be over a hundred. 00:15 Secondly, you have to be having an arrhythmia, so you have to be in a non-sinus cardiac rhythm. 00:21 Now, the term tachyarrhythmias incorporates many different cardiac rhythms and they might be stable or unstable. 00:28 And we're gonna talk about the differences and how you manage the two. 00:31 So, unstable tachyarrhythmias, are situations in which a tachyarrhythmia is present and the patient has some stein of hemodynamic instability or hypo-perfusion. 00:45 So, this is gonna include hypotension or shock, altered mental status or loss of consciousness, ischemic chest pain or dyspnea, or acute decompensated heart failure. 00:58 Basically, any situation in which lack of systemic perfusion is causing end organ damage. 01:05 The treatment of all tachyarrhythmias is the same when the patient is unstable. 01:14 Unstable tachyarrhythmias are life threatening events and you have to assume that the patient is in danger of cardiac arrest. 01:20 So, we're gonna do the same thing for all of these patients. 01:23 We're gonna give them all oxygen. We're gonna monitor them. 01:26 We're gonna establish IV access and do frequent blood pressure checks. 01:29 We're gonna address our ABC's. So we're gonna manage the airway, if we need to. 01:34 And provide any support that's necessary for respiratory distress. 01:39 But the most important thing we're gonna do is perform emergent synchronized cardioversion. 01:45 If a patient is having an unstable tachyarrhythmia the most important thing you can do for that patient is to terminate that rhythm and get them back into a normal perfusing rhythm. 01:56 So, electricity is gonna be the answer for all unstable tachyarrhythmias. 02:01 Now, if possible we wanna provide sedation or analgesia for our patient before performing cardioversion. 02:07 Because you can just imagine 200 Jules to the chest is not really comfortable. 02:12 So, if you have time and the patient's condition permits it, it's definitely better to provide sedation, but if the patient is too unstable for that, terminating the rhythm is the most important thing you can do. 02:23 So, again, cardioversion is indicated for all unstable tachyarrhythmias regarding of what the underlying rhythm is. 02:31 If the patient's unstable and they're gonna tachyarrhythmia, you need to shock them. 02:36 So, it's really important when you're confronted with the tachyarrhythmia to identify specifically what cardiac rhythm your patient is in. 02:45 The reason for that is that you're gonna manage different rhythms in different ways. 02:49 So, you have to understand what rhythm you're dealing with in order to provide the right treatment for the patient. The approach to rhythm identification is always the same. 02:57 Whenever you're looking at a cardiac rhythm, the first question you're gonna ask yourself is, is this a fast rhythm or a slow rhythm? Now, if it's a slow rhythm, you're dealing with sinus bradycardia or maybe a bradydysrhythmia. 03:09 In which case we're gonna cover all of that in another lectures. So, don't worry about that right now. 03:15 If it's a fast rhythm which is what we're talking about in this lecture, the two possibilities are sinus tachycardia or a tachydysrhythmia. 03:25 Now, if it is sinus tachycardia, we're not gonna treat that as a rhythm disturbance. 03:29 Our goal is gonna be to identify the underlying cause and address that. 03:33 But if the patient is having a dysrhythmia during a non-sinus rhythm, then we need to identify specifically what rhythm they're in. 03:42 The next question we're gonna as ourselves in order to do that is, is it a wide complex rhythm or a narrow complex rhythm? Now, when I talk about wide or narrow, I'm talking about the QRS complex and just as a reminder from basic cardiology, a wide complex rhythm is any situation in which the QRS complex is more than 3 millimeters wide or a 120 milliseconds on the ECG. 04:07 So, if it's a wide complex rhythm that suggest ventricular origin of the rhythm. 04:14 It has to be coming from some place below the AV node, typically within the ventricles. 04:20 The other possibility is that it could be a supraventricular rhythm with abnormal conduction through the heart. And we'll talk a little bit more about that shortly. 04:30 The possibilities for wide complex rhythms are either ventricular tachycardia or supraventricular tachycardia with aberrant conduction Now, if we're dealing with a narrow complex rhythm that tells us that the origin of the rhythm is supraventricular. 04:49 It's above the level of the ventricles because in order to produce a narrow complex rhythm the heart has to use the fast conduction pathways which allow rapid depolarization of the heart producing a narrow QRS complex. 05:04 The next question if we identify a supraventricular rhythm is, is this a regular rhythm or is it an irregular rhythm? If it's irregular we're gonna be thinking it out things like atrial fibrillation or atrial flutter with variable conduction. 05:19 If it's a regular rhythm we're gonna ask ourselves whether or not there are normal P waves present, if there are we're back to sinus tachycardia. 05:28 And again, we're not dealing with the primary rhythm disturbance. 05:32 But if there are no normal P waves present, we're dealing with the paroxysmal supraventricular tachycardia and we're gonna talk a lot more about that in slides to come. 05:43 Sinus rhythm or tachyarrhythmia, if you're looking at a fast rhythm. 05:48 Next question, if you have a tachyarrhythmia, is it wide or is it narrow? If it's wide we're dealing with a ventricular origin. 05:58 So, again, wide complex rhythms are those that have QRS duration of longer that 120 milliseconds or 3 millimeters If the QRS rate is greater than 100, you have a tachycardia. 06:12 So, wide complex, wide QRSs, plus fast heart rate equals wide complex tachycardia. 06:19 So, the pathophysiology of wide complex tachycardia is pretty easy to understand. 06:25 Narrow QRS complexes originate above the level of the AV node. 06:30 And these narrow complex rhythms use the His-Purkinje system, which as you recall is a normal conduction system in the heart that allows very rapid depolarization of the entire myocardium, producing a narrow QRS complex. 06:47 Simply put, the impulses move quickly through the system, the depolarization of the heart is efficient. 06:53 It happens quickly and that gives you a nice sharp narrow QRS complex. 06:59 By contrast, when the QRS complex is wide, the rhythm could be originating either above or below the AV node. 07:07 In both cases, however, the normal conduction pathways, the His-Purkinje system is not being used. 07:15 The electrical impulses are sort of travelling from one myocyte to the next in a very inefficient manner. 07:22 This takes a long time to depolarize the entire heart. It's a slow process. 07:27 Meaning that the QRS complex takes longer to be completed. So, it appears as wide on the ECG. 07:35 The vast majority of wide complex tachycardias are ventricular tachycardia. 07:40 So, 90% of patient who you see with wide complex rhythms are gonna be in Vtach. 07:46 There is a small percentage of patient though about 10% who have supraventricular rhythms with abnormal or aberrant conduction. 07:55 Now, the easy way to understand this is to think about bundle branch blocks. 07:58 If you have a baseline bundle branch block, you're gonna have a wide QRS complex even when you're just hanging out in normal sinus rhythm. 08:08 Clearly, if you go into rapid atrial fibrillation or sinus tachycardia, your QRS complexes are still gonna be wide, right? Now, that's a supraventricular rhythm with abnormal conduction because of your bundle branch block. 08:22 So, it's a sort of an easy way to think about it, although, there are definitely other situation which we're gonna cover where you can see wide complex supraventricular rhythms.
About the Lecture
The lecture Unstable Tachyarrhythmia and Rhythm Identification by Julianna Jung, MD, FACEP is from the course Cardiovascular Emergencies and Shock. It contains the following chapters:
- Tachyarrhythmias
- How to Approach to Rhythm Identification
Included Quiz Questions
Which of the following is not a feature of tachyarrhythmia?
- Atrial rate < 100 bpm
- Ventricular rate > 100 bpm
- Presence of arrhythmia
- Includes many different cardiac rhythms
- Can be stable or unstable
What is the most important management for unstable tachyarrhythmias?
- Emergent synchronized cardioversion
- Oxygen supplementation
- Airway control for respiratory distress
- Sedation
- Placement of IV access
Which of the following is always associated with a wide QRS complex?
- Ventricular tachycardia
- Sinus tachycardia
- Atrial fibrillation
- Atrial flutter
- Supraventricular tachycardia
In an ECG tracing, what is considered a wide QRS complex?
- QRS duration > 120 ms
- QRS duration > 90 ms
- QRS width of 2 mm
- QRS width of 1 mm
- QRS rate of > 100
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |