Playlist
Show Playlist
Hide Playlist
T-Cell Lymphomas: Pathophysiology
-
Reference List Pathology.pdf
-
Slides T-Cell Lymphomas Pathophysiology.pdf
-
Download Lecture Overview
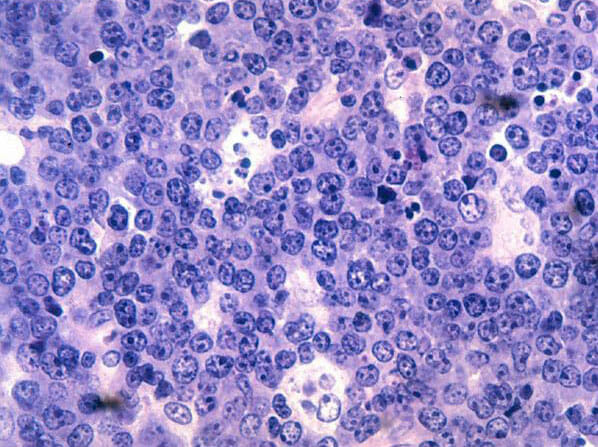
00:00 Welcome. This talk is going to focus on lymphomas of the skin which are characteristically T cell lymphomas. 00:09 So cutaneous T-cell lymphoma also known as Sézary syndrome, are non-Hodgkin lymphomas that primarily present in the skin. They're not always systemic. 00:21 And in fact, the majority of cases, they are just found with an interesting tropism in the skin. So the epidemiology of this it is relatively infrequent, but the incidence does increase with age. 00:34 And it's more common in men. 00:36 The pathophysiology. So overall for all lymphomas anywhere in the body and whether they start in spleen or lymph node or skin, the causes the underlying cause is unknown. 00:48 We do know, however, that there are spontaneous acquired genetic mutations, and these can occur in tyrosine kinases. 00:55 They can occur in jak-stat cytosolic activating pathways. They can occur in notch pathways. 01:04 These are all a variety of ways by which we can drive lymphocytes to become more proliferative and then acquire additional mutations. 01:13 Interestingly, and it kind of makes sense chronic inflammation. 01:16 If we have a chronic inflammatory state, we're getting a repetitive activation and proliferation of T cells. 01:23 And those may in turn acquire mutations that allow them to become malignant lymphomas. And also in the same general vein, infections. So bacterial infections, viral infections, etc. can give rise to chronic activation of certain T cell populations and give rise then to additional mutations in proliferating cells that give rise to lymphoma. 01:49 Initially in CTCL (cutaneous T-cell lymphoma Sézary syndrome), activated CD8 positive T cells and CD4 positive Th1 cells control the tumor growth, and so the abnormal cells are those kind of darker cells in the middle. 02:08 And you don't may not have any manifestations. 02:10 However, as tumor progression occurs due to additional mutations, increased proliferation, and as the host over time may become exhausted and have a change to a predominant Th2 response. That's when we begin to see manifestations in the skin. 02:29 The clinical presentation. 02:31 We get these rounded patches of raised or scaly skin. 02:34 They may be itchy or not. 02:36 That's kind of that look kind of nonspecific. 02:39 It can be a variety of things. 02:41 Um, when it's really intense and rash, like in more diffuse and we demonstrate that it's going to be, in fact, cutaneous T cell lymphoma, we'd call that entity mycosis Fungoides again, someone decided that that looked like a fungal infection. 02:57 It's not. It's due to a dense infiltrate of the lymphoma cells within the skin. There may be lighter colored patches of skin that are also equally involved with the lymphoma, just not exhibiting as much inflammation. 03:14 On the scalp we may see hair loss. 03:16 There may be involvement of both the planter and palmar surfaces. So the palms and soles of our hands and feet may have thickening, and that is due to a leukemic, a lymphomatous infiltrate there and the lymph nodes. 03:33 Even though the disease is primarily manifesting in skin, the lymph nodes may also show lymphadenopathy. 03:39 We may have cells that are tracking into the draining nodes. 03:43 To make the diagnosis, so the micrograph shows dermal lymphoid follicles with a follicular growth pattern. 03:51 The inset highlights atypical large lymphoid cells with irregular nuclei and prominent nucleoli consistent with lymphoma. 04:00 It's seen the lesion being suspicious and then sending material off for, uh, immunohistochemistry and for histopathology. A complete blood count will often give a hint that we have a lymphoma, although you may not necessarily have elevated significantly elevated numbers of lymphoma cells within the circulation. 04:24 CT and PET scans are going to be helpful to see whether there is nodal involvement. 04:29 And clearly you want to do a biopsy of the lesional skin. 04:33 There the epidermis looks pretty good. 04:36 It looks pretty normal, but underneath it is a rather dense collection of blue nuclei representing the lymphoma cells. 04:44 Those can be further examined and we can phenotype them. We can look for genetic mutations, etc.. 04:52 How do we manage it? Once you've made the diagnosis. 04:55 Now we have to give chemotherapy. 04:57 And although you can do topical because the disease can also be in lymph nodes, that may not be sufficient. 05:05 So you may want to give more systemic therapy for the topical targeted therapies for specific vulnerabilities. 05:12 If you know that a certain tyrosine kinase is driving it, you give that tyrosine kinase inhibitor, you can do puva light therapy and put on topical kind of agents that get activated in the setting of ultraviolet light. You can do radiation. 05:28 You can do extracorporeal photopheresis if there's a significant component of the lymphoma that's present within the bloodstream. 05:35 And you can do bone marrow transplant after significant systemic chemotherapy. 05:43 With that, we've discussed an interesting manifestation in skin or an interesting disease process in skin, cutaneous T cell lymphoma.
About the Lecture
The lecture T-Cell Lymphomas: Pathophysiology by Richard Mitchell, MD, PhD is from the course Tumors of Cutaneous Lymphoid Cells.
Included Quiz Questions
Which change in immune response is associated with progression of cutaneous T-cell lymphoma?
- Shift from CD8/Th1 predominant to Th2 predominant response
- Shift from Th2 to Th1 predominant response with increased cytotoxic activity
- Complete loss of CD8 response only with preservation of other immune components
- Increased neutrophil response with subsequent macrophage recruitment
- Enhanced NK cell activity combined with upregulation of perforin expression
Which pathogenic mechanism can lead to T-cell lymphoma development through repetitive lymphocyte activation?
- Chronic inflammation with repeated T-cell proliferation
- Acute viral infection with subsequent immune dysregulation and cytokine storm
- Single exposure to ionizing radiation causing DNA damage and chromosomal aberrations
- Direct toxic effect on lymphocytes leading to apoptosis resistance and clonal expansion
- Bacterial endotoxin exposure triggering polyclonal activation and inflammatory cascade
Which finding characterizes the skin involvement pattern in mycosis fungoides?
- Rounded patches of raised or scaly skin with possible involvement of palms and soles
- Deep subcutaneous nodules only with occasional erythematous presentation
- Vesicular eruptions with umbilication and surrounding erythematous halo
- Linear streaks along blood vessels with occasional peripheral desquamation
- Targetoid lesions with central clearing and raised inflammatory borders
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |