Playlist
Show Playlist
Hide Playlist
Systolic Dysfunction
-
Slides CongestiveHeartFailure CardiovascularPathology.pdf
-
Download Lecture Overview
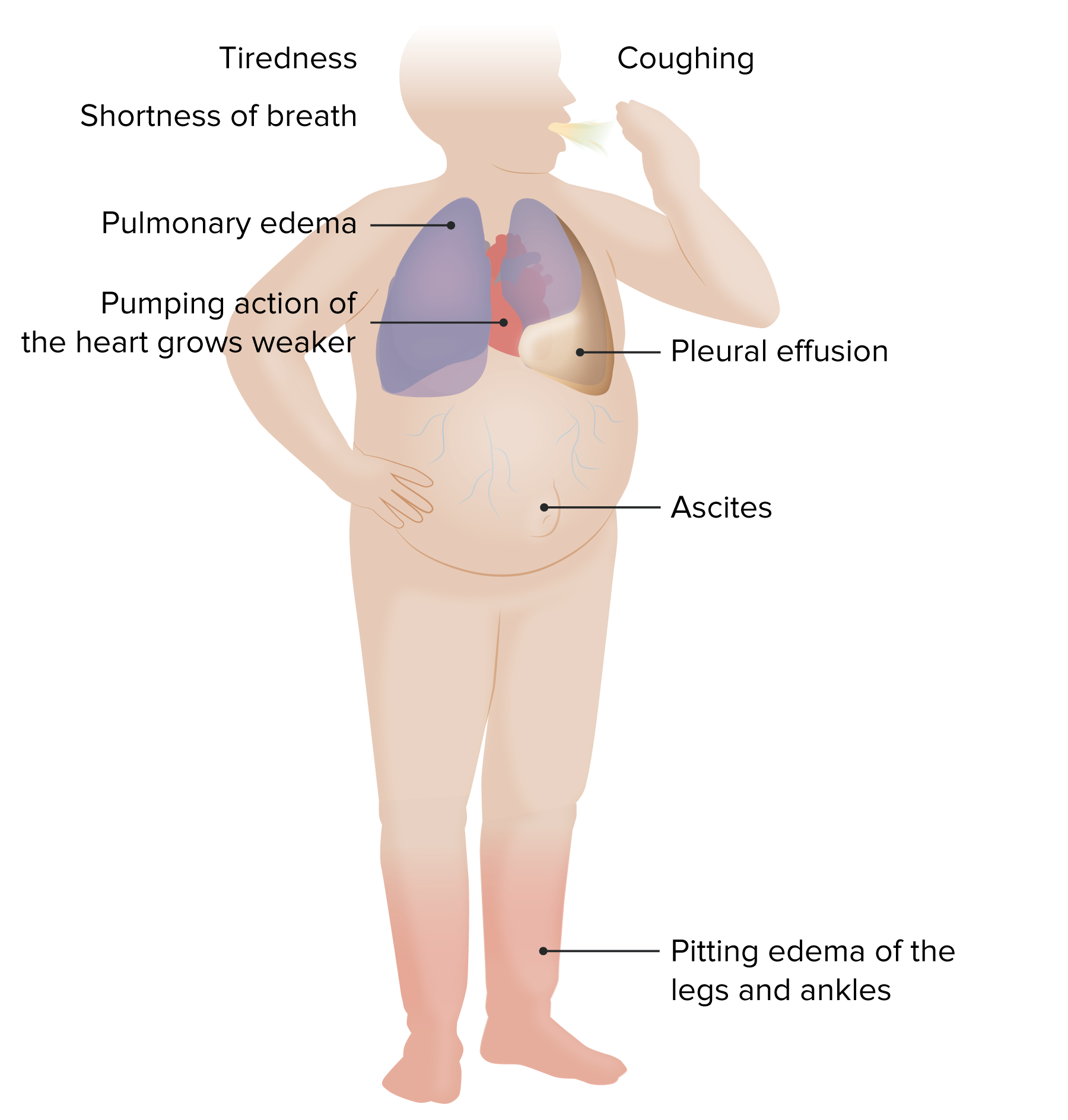
00:00 Let us take a look at the two parameters of dysfunction in further detail. In systolic dysfunction, it is the fact that well the heart is not pumping. Now with that said, there is the all important graph in physio that explains the pathology beautifully. Along with this, well, you want to start thinking about what kind of pharmacologic agents you want to plug in here. So, with this graft that you seen in every single medical text book, clinicians and professors of all type have been discussing this matter for years. Let us put all this together so that you have a firm understanding as to how this graph operates. Well before we do any of this, take a broadside view of the cardiovascular system. 00:49 It is the only way that any of this graft will make any sense to you and not sitting there just memorizing like you would perhaps with physics because that is not what medicine is. Yes sure you can incorporate it but ultimately it is what is going on in the body. So three-dimensionally, broadside view of the heart, is a continuous circuit, isn't it? A continuous circuit, what does that mean? From the left ventricle, blood is being ejected out, but it is completely dependent on the amount of blood that is returning to the heart, isn't it? So, therefore, the venous return to the heart, let it be from the pulmonary veins for the left side or the superior vena cava and the IVC for the right side, is then going to equal the amount of blood that is being ejected out and that then gives you your steady state, doesn't it? How in the world could you possibly have an increase in ejection of the blood of cardiac output if you don't have enough blood that is returning to the heart? How is that even possible? It is not. So, therefore, the fact that you are looking at the cardiovascular system as being a circuit, in which everything is just a perfect circle of flow return is our graph. You will see exactly what I am referring to as we dissect this graph in great detail. 02:09 First and foremost, on the X-axis, remember any graph that you get in pathology, in physiology what have you to do? You have to dissect and take a look at the parameters. The X-axis represents what? Atrial pressure. In other words, this will be volume. Whereas the Y-axis here would represent two different things. It would represent the cardiac output. Number 2, represent the venous return. It has to. Remember I told you what blood comes into the heart is equal The heart creates circulatory flow by lowering the right atrial pressure and allowing the recoil pressure in the veins to drain blood back into the heart. 02:43 The heart then puts the volume back into the systemic circulation so that the stroke returns equal stroke volume. 02:49 The heart cannot pump out more volume than comes back. 02:52 Changes in cardiac output occur because of changes in arterial and venous resistance, which results in redistribution of the blood volume and changes pressure gradients across the vasculature. 03:02 Let's dive into this further so that you will. Next, the three questions that you want to ask yourself with this graph or the three parameters that you truly want to get a firm handle of from physio is performance is equal to changes in cardiac output or contractility and you have your volume. Is that clear? Where does performance come in on this graph? It is the Y-axis. You keep it separate from contractility, please. What do I even mean? I want you to take a look at that cardiac output curve versus normal. You see that. 03:41 Well, that cardiac output versus normal. Anywhere that you would be on that particular curve, answer this question for me, are you changing contractility if you move to the top of that curve by the plateau perhaps or down at the bottom? Are you changing contractility? No. 04:01 As long as you are on that curve and only on that curve without shifting of that curve, then contractility remains exactly the same. Is that understood? If it hasn't, then make sure that you understand it now. Does that curve where it represents cardiac output is that venous return? Not at all. It is strictly cardiac output. It is strictly contractility. 04:25 Now, performance. As we go up and down that curve, contractility remains the same, but then what changes? Performance, interesting. Remember that from physio. So performance will change as it moves up and down, but contractility remains the same. So what is the other parameter that you need to add in here so that all of this makes further sense. It is your vascular function curve. It is your venous return. Isn't it? So your vascular function curve would be represented by what you are seeing here as an intersection point. So where is this normal that your vascular function curve and that represents the venous return. 05:04 So now I want you to take a look at vector A. Vector A represents what? It causes a decrease in your Y-axis. So what are the three things that we were looking at? Performance, contractility, and volume. Performance equals contractility and volume. So, now, vector A shows a decrease. 05:27 A downward movement on your Y-axis, what happen to performance? It decreased. How do the performance decrease? Was it due to volume? I am sorry. Where was the volume on this graph? It was the X-axis and as we move from left to right, what happens to volume? It increased. If you increase volume, how in the world is I am going to decrease performance? What do you mean? Take a look at vector A then look at me yet. Everyone is smart perhaps, but vector A represents a decrease in performance, but that is not due to an increase in volume. 06:01 That doesn't make any sense because you know if you increase the volume, you should increase the stretch. If you increase the length, then you might increase the tension. Welcome to Mr. Frank Starling relationship. So what then cause a decrease in performance please, in vector A? Was there a shift in that contractility curve? Yes, there was. What kind of shift? A clockwise shift. Isn't that how they have described it? A clockwise shift. A negative inotropic effect. What causes this? Maybe myocardial infarction. And myocardial infarction has what type of effect on your heart? A negative inotropic effect. Is that clear? So a decrease in performance due to decreased contractility. Stop there for a second. Now look at me because we are going to predict a few things before you take a look at the graph. If your heart starts failing and it does not want to move forward, it doesn't want to eject the blood forward, what kind of dysfunction is this? What is the category? What is the topic? A systolic dysfunction, isn't it? It is a systolic dysfunction because it doesn't want to move forward. The blood doesn't. It can't because it lost the ability to contract. So now what do you do? What happens? There is increased amount of blood in your heart, isn't there? There is an increased amount of blood in your heart and when there is an increased amount of blood, what then happens to the pressures? It increases doesn't it? When there is increase in amount of blood and there is increase in pressure and it does not want to leave, then what happens to venous return? The blood is stuck in the heart. How could you possibly have more venous return? You don't. You have a decrease in venous return. 07:36 Let us take a look at the three changes that are taking place with vector A. Number 1, a decrease in performance due to decrease contractility. How can you confirm that? An actual shift of the cardiac output curve. Number 2, there is more blood left in the heart. How can you confirm that? The pressure in the heart should increase. Take a look at the X-axis moved from 2 and in which direction are you moving? From 2mmHg, you move to the right. That is number 2. You have increased the pressure. And what's number 3? Venous return. Think about this. More blood is left in the heart. So what happens to venous return? It decreases. Where is venous return? On this graph, on the Y-axis and if you take a look at vector A and you move down what happens to venous return? It decreased. You see that. Good. What are we referring to here? A systolic type of dysfunction. Now we are going to skip over into compensation a little bit and where is my actual fluid? "What do you mean Dr. Raj?" I mean to say that if you have congestive heart failure and you have left-sided heart failure where might my fluid be? You have heard of edema, have you not? Increased hydrostatic pressure, pulmonary edema and we will talk about signs and symptoms. What if there is right-sided heart failure? Then what are you looking for? Once again edema. Where am I? Positive JVD and then what might you have done in the lower extremity? Pitting edema. Transudate. 09:11 What is my point? The point is this, it is the fact that when you have a negative inotropic effect and that fluid is being shifted out, then how the kidneys are going to respond? If the fluid is moving out into the interstitium, there is less effective circulatory volume, isn't it? So when there is less effective circulatory volume heading through towards efferent arteriole, what is going to be released from juxtaglomerular apparatus? It is called renin. 09:40 And then we have the RAAS system, which is going to kick in and here comes mild aldosterone. 09:45 Why? This is the compensation we are paying attention to. Not the neural reflex, this is congestive heart failure. The neural reflex is at this point for all intentented purpose, it is null and void. So we get into aldosterone system. How could you confirm that? I will just show you the patient conceptually. So with this aldosterone, what is it trying to do? It is trying to restore some of that contractility. Let us ask the same questions again with aldosterone. 10:10 With aldosterone, where are we working? Working in the collecting duct. What is the name of that cell? It is the principle cell. What is it doing? It is stimulating sodium-potassium pump or maybe ENaC. Are you picturing that? In the collecting duct of your nephron, way distally in nephron, where are the principle cell? On the basolateral membrane with sodium-potassium pump. It will stimulate it so that we absorb sodium. On the luminal membrane or the apical membrane, it stimulates ENaC or epithelial sodium channel on the hopes of doing what? Reabsorbing your sodium. Is that what the aldosterone does? Of course, it does. It reabsorbs the sodium. In addition, what are you going to do with volume? You are going to retain it, aren't you? Then you have it. Now you have your volume that is increased. When you increase your volume, then now what will happen? Take a look at vector B. So now with vector B, we have an upward swing, we have an upward movement of your Y-axis. So what happen to performance? Increased, because it is the Y-axis. Performance increased, why? Was an increase in contractility? My goodness gracious. Take a look at that curve from vector A. As you go from vector A and where we just move down to a negative inotropic curve and we have moved up through vector B, have we changed or shifted your cardiac output curve? No, you haven't. So contractility remains the same. If you want to confirm that, go back and take a look at physio. This must be understood. So what in the world increase the performance in vector B? It is the fact that you increase the volume. How can you confirm that? Take a look at the X-axis. Vector B, you moved further to the right. You increase the volume thus you increase the performance. How can you confirm that further? Once again in physiology. 12:01 Isn't this amazing that you were able to integrate all this now, in the setting of systolic dysfunction? With all of this when we have an actual change, X intercept. When you have an actual change physically of the X intercept, then you know that you have an increase in volume because you shifted to the right. Thus in the process in this patient with what is known as compensatory congestive heart failure. We do have restoration for this time being of some of this performance. 12:33 But the contractility is still pretty much, overall contractility compared to normal? Decreased. What do you want to do now at this point? This patient has come in, maybe we starting thinking about giving? Drugs. What kind of drugs? Well, you want to try to give those drugs in which it decrease in mortality, it inhibits remodeling and that would be your point. So later on, at some point, we will do a little bit of pharmacology. We will take a look at those drugs depending as to what are they going to ask you? Maybe they will ask you well what kind of drug will increase inotropy and you will correctly say digoxin. 13:10 What kind of drug was going to take care of your preload because of pulmonary edema? Isn't that a symptom that you want to take care of? My goodness. My patient cannot breathe properly, especially at night, wakes up and says "Doc, I have to run to the window, open up the window, gasping for air." So you want to take care of some of the pulmonary edema, one are our diuretic such as furosemide. Or maybe perhaps you want to decrease mortality, increase survival. Welcome to metoprolol, beta-blockers? Be very careful and the reason I say that is because if you have decompensated type of congestive heart failure, you might kill your patient. So strict supervision is absolutely necessary.
About the Lecture
The lecture Systolic Dysfunction by Carlo Raj, MD is from the course Heart Failure: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following changes is associated with systolic heart failure?
- Negative inotropy
- Positive inotropy
- Negative chronotropy
- Positive chronotropy
- Negative dromotropy
Which of the following is NOT a result of decreased contractility of the heart (uncompensated), such as after an acute myocardial infarction?
- Decreased end-diastolic volume
- Increased atrial pressure
- Decreased venous return
- Decreased ejection fraction
- Decreased stroke volume
What change triggers renin release in congestive heart failure with decreased ejection fraction?
- Decreased effective circulating volume
- Decreased venous return
- Aldosterone receptor activation
- Aortic arch baroreceptor activation
- Increased hydrostatic pressure
Which of the following drugs improves contractility of the heart (positive inotropic agent)?
- Digoxin
- Metoprolol
- Furosemide
- Verapamil
- Enalapril
Which of the following drugs decreases preload?
- Diuretics
- Digoxin
- Beta blockers
- Calcium channel blockers
- Phenylephrine
Customer reviews
1,4 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
10 |
As always, Dr. Raj is helping me understand. Absolutely love it.
I have to repeat everything he says three times because of his way of expressing himself, I don't mean the accent, thats fine, but how he puts his sentences together for explaining something is confusing. This is being made way worse by the graphics and the fact that he can't point at what he actually means while he explains it. Also there is no legend to the curves that he explains.
the graphs are not at all explained and vague terms are used which confuses the concept
Terribly "explained". Convoluted. Not simplified at all. 0/10 would not recommend.