Playlist
Show Playlist
Hide Playlist
Syphilis – Treponema Pallidum
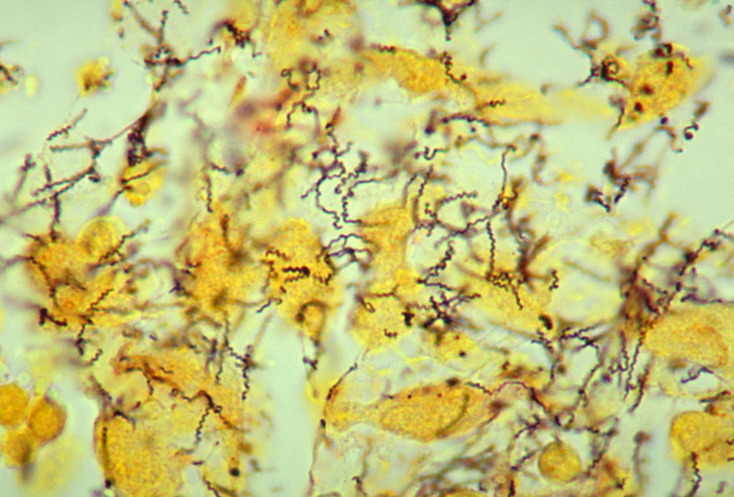
00:01 What or how does one get syphilis? Well, I think most people probably are aware of that but syphilis as a disease occurs in several different stages and the transmission or the contagiousness of the disease depends in part on at what stage the patients is in their syphilis progression. 00:22 In the primary stage, the very first set of disease manifestations, sexual contact is the principal mode of transmission. 00:30 There are many treponemes or many Treponema pallidum organisms present at the mucosal surfaces in the vaginal mucosal walls, in the semen at the tip of the penis - all of these are very contagious and easily transmissible to other sexual partners. 00:48 The image you see on this slide shows again, in beautiful living color, the treponemes, done in sort of an artist rendition along with some of the epithelial cells seen in vaginal mucosa. 01:01 In the secondary stage of syphilis - so after some dissemination has occurred, then any lesions any of the rashes which we’ll discuss in just a minute, are highly contagious because they too are filled with disseminated Treponema pallidum. 01:18 And mothers at any stage but especially in the first and second stages can transmit Treponema pallidum, can transmit the causative agent of syphilis to their unborn babies creating congenital syphilis and this too has a specific set of clinical findings which we’ll cover very shortly. 01:38 And then finally transfusion of blood from the patient who is actively infected with syphilis also can transmit the process. 01:46 So Treponema pallidum quite wily in escaping immune recognitions and quite wily at creating transmission via highly contagious skin findings and other contagious lesions to create additional victims. 02:00 So, before we even talk about the stages of syphilis, let’s talk about what we can do to prevent them. 02:08 Well, if the most likely mode of acquisition is being exposed to mucosal surfaces or to genital surfaces, then practicing barrier contraception via condoms is the most effective way of preventing transmission of syphilis. 02:23 Treatment however for those patient who have forgotten or been unable to avoid acquiring Treponema pallidum, is with penicillin; a lot of penicillin typically injected as a shot into the buttocks and it is a painful injection. 02:40 Talk about paying a penalty for having one night of fun. 02:44 Some patients pay an even higher penalty. 02:46 This is when they develop a reaction called the Jarisch-Herxheimer reaction in which the treatment of the Treponema pallidum kills the bacteria and releases so much antigen so much external toxin from the cell wall that it further induces an intense inflammatory reaction. Patients with the Jarisch-Herxheimer reaction will have high fevers, shaking chills or rigors and many times hypotension or even shock. 03:16 So now, without further ado, as I promised several slides ago, let’s talk about the stages of syphilis and we’ll start with primary syphilis, the first indication of a clinical response to infection with Treponema pallidum. 03:31 Patients with primary syphilis will may times have chancres, these are painless ulcerative lesions on the genitalia. 03:39 In here you can see a picture of the shaft of the penis and although it doesn’t show as well there are also some early lesions on the glands penis. 03:48 These lesions can occur throughout the genitalia and the perineal surfaces meaning around the vagina, around the anus. 03:55 They’re ulcerative lesions, typically with some amount of surrounding erythema or redness but they are painless, that’s the key thing. 04:04 Proximal to or draining from the site of the chancres, will be inflamed lymph nodes, buboes, very much like we have described in our other session about the plague with you Yersinia pestis. 04:18 Buboes are painless but swollen lymph nodes occurring several weeks after the initial infection occurs and they simply suggest that’s where the major immune reaction is occurring. 04:31 Where do you typically see signs of primary syphilis? Well, typically at site of the inoculation so external genitals as we said, the anus, the vagina or sometimes even the mouth. 04:45 Onset, up to three weeks after initial introduction of the Treponema, 21 days is actually fairly accurate and healing starts for the next 3 to 6 weeks afterwards but it can be a slow process. 05:00 At this stage, anytime during the incubation period certainly during the signs and presentation of clinical symptomatology, one can make a diagnosis through dark field microscopy looking at a swab from the base of one of these lesions, yes, it is somewhat exciting to acquire that but it’s how one can make the diagnosis. 05:19 One can also start to look for the serologic responses with the non-Treponemal and Treponemal tests. Treponemes certainly we found in chancre fluid if possible or even potentially in draining one of those buboes, those inflamed lymph nodes. 05:35 And if one obtains the non-Treponemal test, the VDRL or the RPR, those will be positive and up to 80% of patients but keep in mind that just as false positives occur so too do false negatives. 05:51 So a negative test in this situation does not exclude primary syphilis. 05:55 Moving on then to secondary syphilis, here the clinical manifestations are very much a flu-like illness. 06:03 It’s not specific, there may be low to sometimes high grade fevers. 06:07 The patients feel quite ill, they have anorexia, they have sore muscles with myalgias. 06:14 They have swollen lymph nodes in a generalized way so generalized lymphadenopathy. 06:18 Certainly they might have things like sore throat, headache if they didn’t know any better and many patients don’t, because their primary syphilis may have been silent, they might simply think they have the flu. 06:30 However development of the rash is starting to become a very specific sign of secondary syphilis. 06:36 The rash as described in the slides is a disseminated maculopapular rash and you can see two examples of that in the top two images on the slide, the one that shows the back, flat somewhat erythematous lesions which you're noticing. 06:51 The upper right however shows the hallmark of a syphilitic rash in the secondary stage that is presence of lesions on the palms and on the soles of the feet. 07:02 There are very few infections known to human medicine, human science that cause a palmar or plantar rash and secondary syphilis is absolutely one of them. 07:13 If one then finds a third finding, so flu-like illness, palmar or plantar rash along with a disseminated maculopapular rash and this third finding called Condyloma latum, these are flat lesions they look very much wart-like and that would be the bottom picture on the slide. 07:32 They’re smooth, they are moist they typically occur again at the scene or the site of initial inoculation, so the perivaginal area, the perirectal area, sometimes around the glans penis. 07:45 These along with the palmar and plantar rash should be screaming the diagnosis of secondary syphilis. 07:52 And as we’ve noted, the rashes and the lesions will easily be found in the anogenital area. 07:59 Onset. This typically occurs sometimes days to weeks to months rarely years after the primary syphilis starts. 08:10 The most typical time is four to ten weeks after the primary infection occurs and it lasts up to eight months or so. 08:19 The lesions themselves are highly contagious. 08:22 This is unfortunate because many patients of course will not recognize the significance of a palmar or plantar rash and as you, the unsuspecting clinician walk into the room to introduce yourself to the patient appropriately shaking hands, you may have just been exposed to millions upon millions of Treponema pallidum transferred by a simple hand shake. Unfortunate, but yet we are physicians and therefore very good hosts - sorry. 08:50 After resolution, then there’s another quiescent period before we get to the next stage but during any point of the stage, the active secondary syphilis or even as the lesions are resolving one can demonstrate Treponema pallidum through dark field microscopy and of course with the serologic tests which we’ve already talked about. 09:10 Moving then on to the final stage, tertiary syphilis. 09:15 Tertiary syphilis has a been associated with such lesions as called gummas which is represented in the scrotum of the patient in the picture on the slide. 09:27 Gummas are granulomatous lesions but they are very slow growing and they are very slowly destructive. 09:33 In fact, because they’re relatively asymptomatic, other than looking quite noxious if they’re on the surface of the skin, they can cause hollowed out or pitted lesions, especially in bone and connective tissue. 09:46 In looking at archeologic specimens in patients from certain parts of the world where syphilis was quite prominent, one can see these hollowed out pits or cavities in the flat bones and even the long bones of those patients suggesting that syphilis is very much disease of the old world. Columbus wasn’t the only one who was associated with syphilis. 10:10 Also present in this tertiary stage of syphilis can be very severe systemic manifestations, one of which is neurosyphilis. 10:20 This is a very bad player because it can create a demyelinating or inflammatory lesion of the dorsal horns and posterior columns of the spinal cord and it can be slowly progressive, so patients may start with loss of sensation, they may start to be ataxic in their gait. 10:39 They may develop a broad based gait which has also been called sometimes a sailor’s gait like a sailor on a ship. 10:47 They also may develop the Argyll Robertson pupil which has been unfortunately nicknamed the prostitute's pupil. 10:55 This is the pupil that when you ask the patient to look afar and then up close, their pupil does constrict with accomodation but it does not react to light, the afferent light reflects has been systematically destroyed by neurosyphilis. 11:09 Patients may also developed cardiovascular syphilis in which they can get inflammation any of the blood vessels but especially the aorta along with aortic dissection and aortic aneurysmal rupture, not a good player at all. 11:23 So you can see a variety of signs under the clinical manifestations described for tertiary syphilis. 11:29 The broad base, the ataxia, as noted for neurosyphilis; having a positive Romberg sign meaning that they have ataxia, they’re unbalanced, developing Charcot joints along with contractures. 11:42 Even having stroke without hypertension - due to the aortitis, due to the vascular inflammation. 11:49 So, this process after the secondary syphilis can take years to decades and it’s not everybody but in effect it may not be anybody for even decades until they eventually pass away, but in those few who do develop tertiary syphilis, it is quite a diagnostic dilemma because most of these signs are nonspecific and most of these signs are hidden under the surface of the skin so diagnosis can still be made serologically with the non-Treponemal and the Treponemal antibodies as well as performing specialized molecular diagnostics such as the PCR on spinal fluid, but it takes diagnostic suspicion to think of tertiary syphilis before one even sends the proper tests. 12:34 Let’s spend a little time talking about congenital syphilis mostly because this is about as frequent as are the primary and secondary syphilis cases we just discussed with adults in large part because mothers who may be carrying child may not be aware that they have a primary or secondary syphilis. 12:53 Transmission can occur at any stage of syphilis. 12:58 It occurs most clinically significantly in terms of the fetus, the baby, when it occurs during the first trimester and this makes sense because infection and transmission by any infectious agent will always have greater impact the earlier in the life of the fetus that it occurs. 13:16 It can affect tissue progress, it can affect tissue development, so that then is the time to test the mothers; the earlier the better and in fact, most parts of the states in most parts of the world, recommend testing pregnant mothers at least twice and in fact three times during the pregnancy. 13:35 The first time upon discovering of the pregnancy to get an initial status, the second time during the late second or early third trimester and the third time at the time of delivery because infection or reactivation of syphilis can occur at any of these times and every single one of those times would be an opportunity to treat the mother and potentially to treat the baby. 13:59 What are the clinical manifestations of congenital syphilis? Early on, meaning when the baby is born, they may show such sign as enlargement of the liver and spleen, hepatosplenomegaly. 14:13 They may show some rash, they may show what looks like post-date skin, very dry crinkly skin which actually is a manifestation of that sort of great overturn of the skin due to prior infection. 14:28 Eventually, as they grow older, they’ll develop these additional findings several what you see on the images here. 14:35 Facial abnormalities such a rhagades, yes, that’s pronounced rha-gades not rha-ge-des, although some might try to say that in your presence. 14:45 The rhagades are linear scars at the angle of the mouth, you may think of them as sort of a fan-shape or like what some people might call angular cheilosis but the rhagades are due to syphilis occurring in utero. 14:59 That baby’s picture also demonstrates a nasal discharge and a classic finding in congenital syphilis both early like in the first couple of days to weeks after delivery and even later is what it’s called the snuffles, not the sniffles such that you get with the common cold but the snuffles. 15:18 Copious, mucopurulent discharge sometimes in fact frequently progressing to become overtly bloody, this is something that you could not miss - it’s very prominent. 15:31 Patients even later in life then, so not in the early infancy stages but later still to develop into childhood, adolescence and adulthood, may develop what’s called as a saddle nose. 15:43 A saddle nose is best seen in profile the patient. 15:47 I’ll just turn this way for a second. 15:49 The nose itself dips in like that and it becomes sort of a suppressed saddle shape, it’s really quite prominent and you can actually see many examples of that in historic paintings in the traditional series. 16:02 Teeth, the notched or Hutchinson’s teeth such as you see in the image on the lower part of the screen, you can see at almost all of the incisors and even some of the canines that there’s a central divot if you will, that would be called Hutchinson’s teeth. 16:20 If you look at the molars in somebody with congenital syphilis, they may have what’s called a mulberry molar, this is a fat, squat, it looks like a mulberry if you even know what that is, but it’s a very bulbous looking molar far more so then the normal smooth walled straight and purposeful looking molar. Also the maxilla itself may be shortened. 16:43 Saber shins, certainly something one can see on imaging as well as looking at the patient, they sort of bow outward and then cranial nerve VIII deafness. 16:52 So, congenital syphilis is a very bad player when it occurs and it is so preventable if only we can remember to test and treat the mothers at every stage in their pregnancy.
About the Lecture
The lecture Syphilis – Treponema Pallidum by Sean Elliott, MD is from the course Bacteria.
Included Quiz Questions
The Jarisch-Herxheimer reaction is caused by injecting high doses of which antibiotic in patients with syphilis?
- Penicillin
- Ceftriaxone
- Ciprofloxacin
- Azithromycin
- Gentamicin
Which of the following describes chancres formed as a result of primary syphilis?
- Painless, ulcerated skin lesion
- Painful, ulcerated skin lesion
- Painless, raised skin lesion
- Painless, nodular skin lesion
- Painful, raised skin lesion
When do buboes appear in patients with primary syphilis?
- 1–2 weeks after chancres
- 1–2 days after chancres
- 1–2 days before chancres
- 1–2 weeks before chancres
- 1–2 hours after chancres
For patients with primary syphilis, diagnosis can be made by observing treponemes under which microscope?
- Dark-field microscope
- Light microscope
- Electron microscope
- Immunofluorescence microscope
- Stereo microscope
Which of the following describes the condyloma lata formed as a result of secondary syphilis?
- Smooth, painless, flat lesions
- Smooth, painful, flat lesions
- Smooth, painful, raised lesions
- Rough, painless, flat lesions
- Rough, painful, raised lesions
Which type of rash is present in patients with secondary syphilis?
- Maculopapular rash
- Vesicular rash
- Papular rash
- Macular rash
- Papulovesicular rash
Which of the following conditions may be caused when Treponema pallidum involves the nervous system in patients with tertiary syphilis?
- Tabes dorsalis
- Central cord syndrome
- Lumbar spinal stenosis
- Syringomyelia
- Posterior cord syndrome
Which complication may be produced when Treponema pallidum involves the cardiovascular system in patients with tertiary syphilis?
- Aortitis
- Pericarditis
- Endocarditis
- Myocarditis
- Pancarditis
Which cranial nerve may be damaged in congenital syphilis?
- Cranial nerve VIII
- Cranial nerve VII
- Cranial nerve V
- Cranial nerve X
- Cranial nerve VI
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Covered all high yield points , very nice illustration which helps in remembering things better