Playlist
Show Playlist
Hide Playlist
Special Tests for the Evaluation of the Hip
-
Slides Osteopathic Evaluation of the Hip.pdf
-
Reference List Osteopathic Manipulative Medicine.pdf
-
Download Lecture Overview
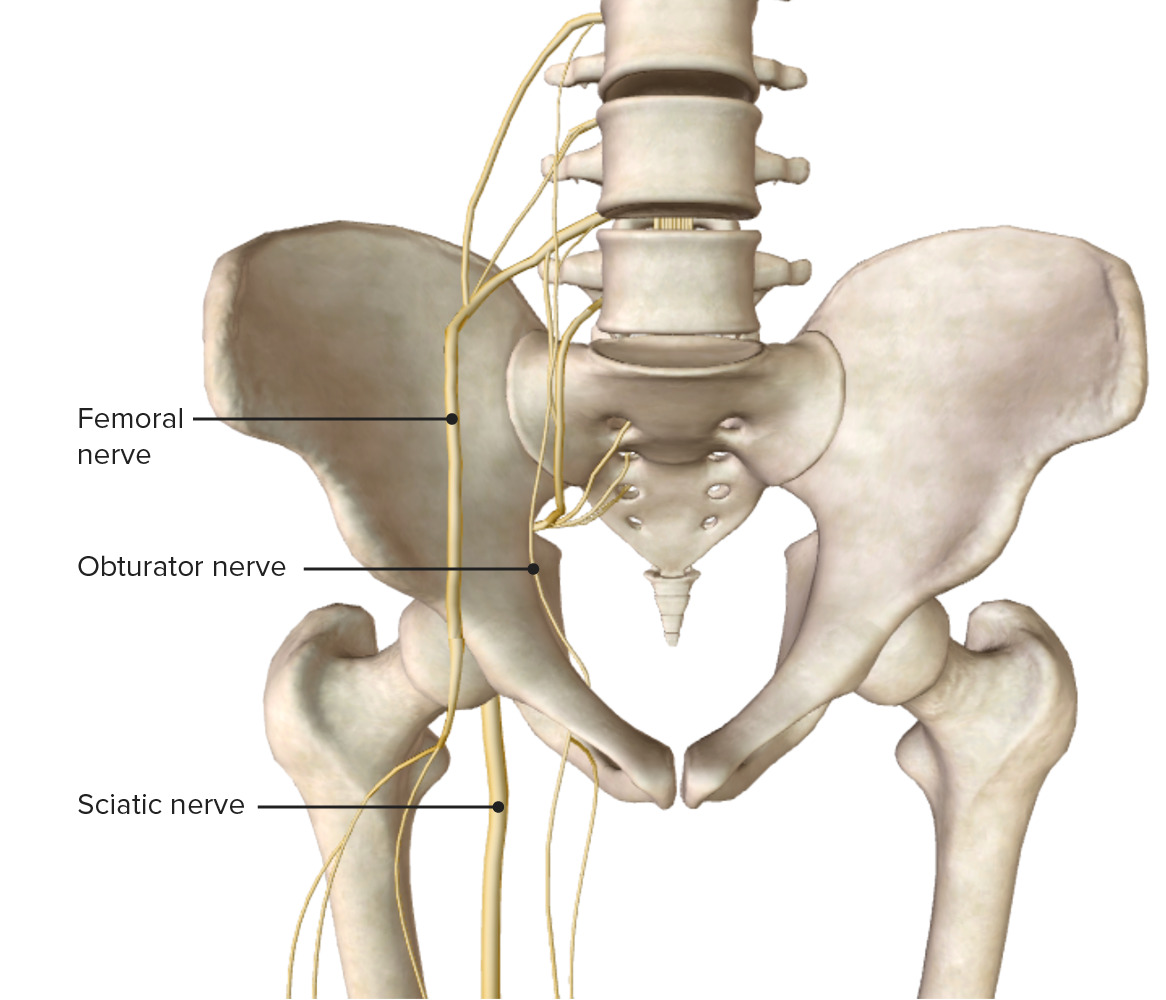
00:01 When considering hip pathologies, there are several special tests that we could utilize to help narrow down our differential. 00:08 So we could perform a Trendelenburg test to check for gluteus medius weakness, straight leg raising to check for lumbar radiculopathy, Stinchfield tests for intra-articular hip pathology, FABERE test or Patrick’s tests to check for range of motion restrictions in the hip, Fadir also will check for range of motion restrictions in the hip, the Thomas test will check for iliopsoas contraction, Erichsen’s for any sacroiliac restrictions, Ober’s test for contracture of IT band, and the hip drop test will check for any lumbar involvement with back pain and hip pains. 00:47 So the Trendelenburg test is a special test that tests for gluteus medius weakness. 00:53 And so, if we have a patient complaining of back pain, buttock pain, feeling unstable when they’re ambulating, or weakness in the hip, what we could do is to perform the Trendelenburg test to see if there’s gluteus medius weakness. 01:08 And so, what you’re going to do is to ask the patient to pretty much stand and then try to stand on one leg. 01:14 So in the image here, you could see how the patient is picking up their left foot, and when you lift the left foot, the right gluteus medius has to fire so it stabilizes the hip and allows the hip to stay level. 01:31 An abnormal test is when you have someone trying to lift up their leg and that hip actually drops. So the iliac crest will drop because the gluteus medius on the opposite side cannot fire and hold the pelvis more level. 01:46 So a positive Trendelenburg test will give you a positive gluteus medius on the standing leg or the side opposite the leg you’re lifting. 01:59 Straight leg test is a test to check for any lumbar radiculopathy or sciatica. 02:06 What you’re doing here is with the leg straight, you’re slowly flexing the hip. 02:12 So the patient is supine, you’re going to passively— with the leg straight— slowly flex the hip to about 70°. 02:24 And what this does, is this puts a stretch on the sciatic nerve. 02:30 If the patient has pain recreated that shoots down the leg then that is a positive test. 02:37 So when you’re stretching that nerve, if someone has some sort of compression, inflammation, or irritation, the patient will complain of pain when you’re flexing the leg. 02:49 You could confirm also by slowly lowering the leg, maybe 5°, then dorsiflexing the toes. 02:56 If you do that and the patient has pain again, that helps to confirm the positive straight leg raise. 03:03 You could also perform this on the opposite side, or the side that the patient is not complaining about, because usually if you have a lumbar radiculopathy or sciatica, it effects one side. 03:13 But if you perform the test on the opposite side, and the patient gets the pain on the side where it originally hurt, that also confirms your suspicion. 03:24 So test both sides when you’re performing the test to see if the patient has lumbar radiculopathy. 03:30 And so a positive straight leg test is indicative of some sort of sciatic or radicular pain. 03:39 Stinchfield’s test is a test for intra-articular hip pathology. 03:43 So if the patient complains of hip pain and you’re suspecting possible osteoarthritis or some sort of degenerative change in the hip itself, you could perform this test. 03:52 So for this test, the patient is supine and here you’re going to have the patient actively try to raise the leg off the table while you provide resistance. 04:01 Pain within the joint would be a positive test for a possible intra-articular hip pathology. 04:11 Patrick’s test or FABERE’s test is a range of motion test for the hip. 04:15 So FABERE actually stands for the motions that you’re going to put the hip through. 04:22 So the motion that you engage the patient in is you’re going to take the hip into flexion, abduct by letting the knee come out to the side, externally rotate and extension. 04:32 So usually you’re going to feel for possible range of motion, if there’s restriction. 04:38 If the patient can’t get into that position, could indicate that there’s a problem with the SI joint, the hip, or some sort of muscle imbalance or muscle problem. 04:48 So it’s a positive test if you’re unable to kind of create that figure 4 with the leg, and then you have to motion test each individual one to try to distinguish what is the key problem. 05:04 FADIR test here or FAIR test what you’re doing is here you’re moving the hip into flexion, adduction, and internal rotation. 05:14 So again, we’re looking for the quality, quantity, and symmetry of motion on both sides. 05:19 It could indicate a problem with the hip joint itself or muscular problems such as a piriformis spasm. 05:24 And so again, a positive test is if you’re unable to move the hip through its full range of motion. 05:32 The Thomas test is a special test to check for psoas muscle hypertonicity. 05:37 So the psoas muscle is a very important hip flexor, and when that muscle is irritated or inflamed, that could cause a lot of hip pain and even lower back pain because remember the psoas attaches from the anterior bodies of the lumbar spine and comes down and attaches to the lesser trochanter. 05:54 So when we have a psoas muscle spasm, that could cause hip and lower back pain, and sometimes patients may complain of like an anterior groin pain from it. 06:02 Remember that the psoas muscle is a hip flexor so things that patients usually complain about when they come in with a complaint of psoas pain, is that they were sitting for a long time and suddenly got up, or they were in a crouch or crawling position or gardening position and suddenly get up, and that sometimes can cause that psoas spasm. 06:22 And when the psoas is spasmed, they complain about not being able to fully stand up straight or potentially having more pain when they’re lying down flat. 06:30 So to perform the Thomas test, we have the patient supine. 06:34 And first, the patient kind of grabs both of their knees to their chest and then they allow one leg to extend. 06:42 What the physician does then is to measure the distance between that extended leg and the table. 06:49 Really, the popliteal crease should get down to the table without any problems. 06:55 Sometimes patients might kind of arch their back a little bit more to let the leg come down. 06:59 So you want to make sure that they’re not arching to allow their leg to reach the table. 07:03 And then you do the same for the other side. 07:05 A positive test really is when you note that the hip does not extend all the down onto the table on one side because that’s psoas contracture or spasm is preventing that hip from going into extension. 07:16 So a positive Thomas test signals a potential psoas spasm on the affected side. 07:25 Erichsen’s test. 07:26 So Erichsen’s test is a test for sacroiliitis. 07:29 So if you have inflammation of the sacroiliac joints, patients will complain of tenderness and pain in their sacroiliac joints. 07:40 So to perform this test, the patient is supine. 07:42 The physician is going to place both your hands on the ASIS on the innominates and then you’re going to apply a medial pressure— kind of medial and a little bit towards the table. 07:53 And as you compress at the ASIS bilaterally, what you’re doing is you are gapping the SI joints posteriorly. 08:02 Patient’s that have pain when you perform that maneuver would be a positive test on that particular side. 08:09 So the Erichsen’s test screens for sacroiliitis, and again, a positive test would be pain on the side when you’re adding the compression to the ASIS. 08:22 Ober’s test. 08:23 So Ober’s test is a test to check for IT band contracture. 08:26 This is more common with patients that are runners or marathon runners. 08:32 Patients that have these contractures will usually complain about perhaps lateral knee pain. 08:37 So remember the iliotibial band comes down and attaches along the lateral aspect of the leg into the fibular head and so patients might have lateral knee pain or pain along the lateral aspect of their leg into the hip. 08:50 So to perform the test, what we do is we have the patient lying on their sides so the affected side is up. 08:57 The physician is going to take the knee and abduct the hip and so as you abduct the hip you shorten the IT band. 09:09 And when you release the hip to let the leg fall towards the table, someone with a contracted IT band will have like a delayed drop or ratcheting motion as it comes down. 09:22 So Ober’s test is testing for iliotibial band spasm or contractures. 09:27 And again, as you’re releasing the leg, if there’s a decrease in the rate of how it drops or ratcheting as you move and let the leg fall towards the table then that would be a positive test. 09:40 The hip drop test or lateral lumbar flexion test could help to discern whether or not there’s some sort of lumbar involvement with back pain and hip pains. 09:50 So lateral lumbar flexion is also known as sidebending of the lumbar spine, so what we’re looking at here overall is to see if someone drops their hip whether or not the lumbar spine side bends accordingly. 10:02 So to perform the test, we’re going to start with the patient standing with their feet about 4 to 6 inches apart. 10:08 As a physician, you want to get about eye level to the lumbar spine to see if there is changes and how much the hip is dropping. 10:17 You’re going to ask the patient to bend one knee while both feet are flat on the ground and you’re going to look at how the lumbar spine shifts and whether or not it shifts smoothly. 10:27 So you want to look at how much the hips drop so if I ask the patient to bend their right knee you are going to note how much that right hip drops and see how fluid that movement is. 10:38 And so you’re going to compare the side that drops more is going to be opposite to the side of the greatest lumbar sidebending. 10:46 Or in other words, the lumbar convexity on the side as the side of the greatest amount of drop. 10:54 So your lumbar will be convex on the side of the greater hip drop. 10:58 There’s some additional musculoskeletal disorders that we need to be aware of in children and adolescents. 11:05 There are certain diseases that you have to kind of keep in mind. 11:08 Congenital hip dislocation or developmental dysplasia of the hip are some things to be concerned about with kids. 11:18 Legg-Calve-Perthes is also another hip problem that you should be aware of. 11:22 Slipped capital femoral epiphysis and also transient synovitis are all more prevalent and common in children. 11:32 Whereas in adults due to aging, wear and tear, and trauma, adults have a different set of differentials. 11:42 Keep in mind avascular necrosis. 11:43 Remember we talked about how the femoral head doesn’t receive as much blood supply so patients might complain about hip pain and you can’t find anything going on musculoskeletally. 11:55 Sometimes x-rays or CT will help pick up on avascular necrosis. 12:01 Ischiogluteal bursitis. 12:02 So the different bursas that lie close to the hip joint itself sometimes become inflamed. 12:10 The trochanteric bursa also could become inflamed and cause hip pains. 12:14 The iliopsoas also has a bursa and also the iliopsoas could also have a tendonitis that could cause that anterior groin pain. 12:22 Psoas syndrome—we discussed a little bit about how the psoas muscle could become spasmed but then that also leads to a whole syndrome where there’s compensatory changes that could occur. 12:33 Piriformis syndrome— the piriformis could be spasmed and also cause pain in the hip and also pain shooting down the leg. 12:41 And osteoarthritis is another common thing on your differential list you should think about for adults that complain about hip pains. 12:51 So iliopsoas bursitis and tendonitis, also known as “snapping hip syndrome.” Patients may complain of a snapping sensation or sound with hip flexion. 13:03 Usually the patient will present with like a psoas gait which is more of like a kind of a staggering, waddling gait and a positive Thomas test. 13:15 Patient will have pain kind of in that anterior groin and femoral triangle region. 13:21 They will have a pelvic shift to the opposite side and it could be associated with visceral somatic dysfunctions. 13:28 Your psoas muscle is in close proximity to your appendix. 13:33 You also have the kidneys and the ureters that travels kind of over the psoas muscle. 13:40 So visceral dysfunction or problems could potentially irritate the psoas muscle. 13:46 So it’s something to kind of think about. 13:49 Psoas syndrome usually starts with a somatic dysfunction of the psoas. 13:54 So the psoas is spasmed, and what happens when the psoas muscle is spasmed, is based on its attachments to the lumbar spine. 14:01 It usually causes a non-neutral, usually a flex dysfunction of L1-L2 on the side of spasm. 14:09 Usually you also have a sacral dysfunction— a right on right or left on left— based on the side of spasm and the pelvis will shift to the opposite side. 14:19 Usually you’ll also have involvement of the opposite piriformis. 14:23 So if you see someone with a piriformis syndrome or piriformis spasm that isn’t resolving with treatment, make sure that you check the psoas on the opposite side. 14:35 Piriformis syndrome. 14:36 Piriformis syndrome is a syndrome that occurs when patients might complain about shooting pain radiating down their leg. 14:43 And you need to distinguish this from lumbar radiculopathy because the pain is due to compression of the nerve or inflammation of the nerve as it passes close or through the piriformis muscle. 14:56 So the sciatic nerve could have two different anatomical variations. 15:01 It could pass through the piriformis or sometimes it could actually bisect the piriformis because the piriformis could arise from two tendinous origins. 15:11 And so you can see how spasm of that muscle could compress that nerve causing pain to shoot down the posterior lateral aspect of the leg. 15:22 So usually patients might complain about piriformis muscle spasms which could arise from a sudden fall on the buttock region or the sacroiliac region. 15:33 Sometimes patients don’t have to necessarily fall and hit something but it’s almost have a slip and a near fall where they catch themselves and that piriformis muscle fires to try to stabilize their hip and they could have that spasm that could occur. 15:47 Sometimes prolonged sitting could irritate that region or sometimes overuse of the muscles of the hip could also irritate that muscle leading to irritation of the nerve. 15:59 Having items in the back pocket, where you’re kind of sitting on your wallet for men, could also irritate the nerve and the muscle. 16:08 And sometimes, the pain is worsened by sitting and walking. 16:12 It could effect stride, your gait and also lead to decreased internal rotation, that positive FADIR special test, and sometimes you could develop a piriformis tender point where you’re pushing along the muscle and the muscle belly and the patient cries in pain as you’re palpating in that area without any other significant lower back pain in the lumbar spine. 16:36 Osteoarthritis is also an important consideration of the hip. 16:40 You could have wear and tear of the hip joint where you have degeneration of the femoral head or the acetabulum. 16:50 Usually on x-ray, you can see some degenerative changes, narrowing of the joint space, or bone spurs, or a non-smooth appearance of the actual femoral head and the acetabulum. 17:04 Usually, your symptoms could be so severe that they may require total hip replacement. 17:11 Osteopathic manipulation could potentially help treat some of the muscle spasms and pain in the area and help delay some of the surgeries that need to occur. 17:22 Osteoarthritis of the hip could affect anywhere up to 85% to 90% of the population that is greater than 65 years old and is really the most common form of articular degeneration. 17:34 So osteoarthritis is graded on a scale of 1 to 4 based on imaging. 17:39 So on imaging, if you see some minor chondral changes that might be a grade 1 and it becomes as severe as a grade 4 when you have additional changes to the bony surface and also to the femoral head. 17:53 Usually on examination, patients might have decreased internal rotation of the hip. 17:58 Patient might also have a positive Stinchfield test which was a test that tests for intra-articular hip pathology. 18:07 So with that knowledge of anatomy and physiology and these different examination skills and special tests, it could help you determine the different hip pathologies that your patients may present with.
About the Lecture
The lecture Special Tests for the Evaluation of the Hip by Sheldon C. Yao, DO is from the course Osteopathic Diagnosis of the Hip Region. It contains the following chapters:
- Special Tests for the Evaluation of the Hip
- Additional Musculoskeletal Hip Disorders
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |