Playlist
Show Playlist
Hide Playlist
Shigella – Enteric Bacteria
-
Slides 03 EntericBacterialDiseases MicrobiologyAdvanced.pdf
-
Download Lecture Overview
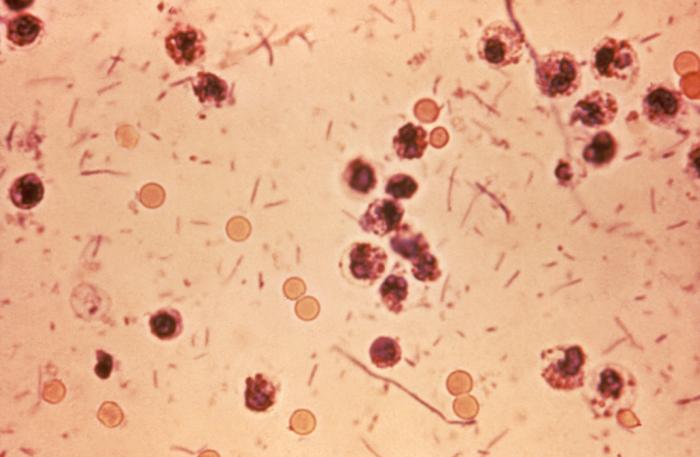
00:01 So the shigella come in four species, shigella dysenteriae, shigella flexneri, shigella boydii and shigella sonnei, and these are all capable of causing dysentery. 00:16 These bacteria are spread from person-to-person via contact or by contaminated food or water, and you don't need a lot of these bacteria to cause an infection, only a hundred or a thousand are enough, so very minimal contamination of food for example or transmission of minimal numbers is enough to initiate an infection. So you ingest these organisms, they go to your intestine and they invade through M cells. Now M cells you may remember from an earlier lecture about bacteria are the cells that are interspersed throughout the other epithelial cells and these cells are constantly sampling the lumen of the intestine to make sure there aren't any dangerous antigens there. So they take up things very actively and pass them through to immune cells on the lower side of the intestinal wall. Many pathogens take advantage of M cells to enter the host and shigella is one of them. They bind to M cells and they get passage through the M cell and then they're released onto the underlying space which is called the lamina propria. In this process, M cells are often full of macrophages that are there, sampling antigens, they take up the shigella in this case, but the shigella are not destroyed by the macrophages. They escaped the phagosome in the macrophage which is taking them up, get outside and they can spread elsewhere, but this transitory experience with the macrophage causes the release of cytokines from the macrophage, that causes inflammation of course. The cytokines recruit other cells to the infected area and all of this causes the symptom of infection. These shigella, by the way, which are shown as the red oblong bacteria here, can then invade epithelial cells from the bottom. So they've come in through the M cell, they're in the lamina propria and now they go back into the epithelial cell from the bottom. They ride the host cytoskeleton up to the surface again and now they're back on the surface of the epithelial cells. And they can go through multiple cycles of reinfection and being brought to the top again, eventually this destroys M cells as well as epithelial cells. The cells come off, so you end up having erosion of the gut wall or an ulcer, so this is a physical removal of cells as a consequence of bacterial inflammation. You have an ulcer and in the process of doing this, many other immune cells have been trying to clear the infection, including neutrophils, major defense cells for many bacterial infections as we've mentioned before. These cells die in the process and they accumulate in the stool and that's what provides the pus for the stool, the presence of all these dead immune cells. So the lesion in the wall, the dying neutrophils, that gives you the blood and the pus in the stool, part of the dysentery. 03:22 One of the species of shigella produces another toxin called shiga toxin and this toxin has a specific effect in our cells. It cleaves the large ribosomal subunit, the 60S subunit and that stops protein synthesis, so that basically kills the cells and is partly responsible for the cells leaving their position in the epithelium and causing that ulcer. You do need to take oral fluids to take care of a shigella induced dysentery, you don't need intravenous fluid, you can just take this by mouth. 03:58 You can use antibiotics, but there's a lot of resistance out there and they are not effective.
About the Lecture
The lecture Shigella – Enteric Bacteria by Vincent Racaniello, PhD is from the course Bacteria.
Included Quiz Questions
Shigella invades the host through which of the following mechanisms?
- Enteric M cell invasion
- Receptor-mediated endocytosis
- Pili adhesion
- Phagocytosis via luminal macrophages
- Epithelial cell destruction and invasion
Which of the following describes the pathological mechanism of action of Shiga toxin?
- Cleaves mammalian 60s ribosomal subunit
- Increases protein synthesis
- Prevents the formation of the mammalian 30s ribosomal subunit
- Increases intracellular cGMP
- Decreases absorption of Na and increases secretion of Cl
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
well most know that shigella destroys gis mucosa...but the pathophysiology is now clear...thanx lecturio