Playlist
Show Playlist
Hide Playlist
Seborrheic Keratosis (Seborrheic Eczema) and Actinic Keratosis (Solar Keratosis)
-
Slides Dermatology Neoplastic Skin Diseases.pdf
-
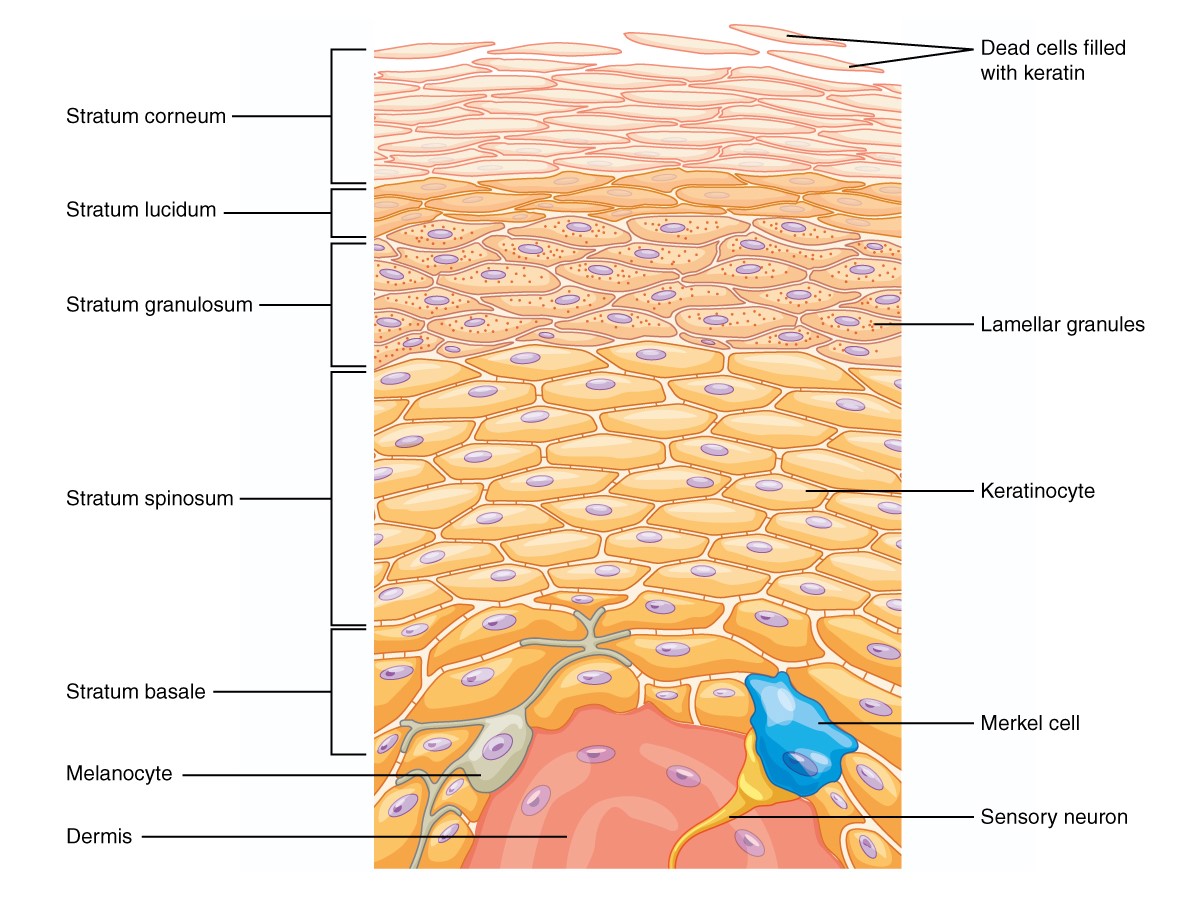
Download Lecture Overview
00:02 Our topic here is seborrheic keratosis. 00:05 A common epidermal tumor consisting of a benign proliferation of immature keratinocytes Very common in the elderly. 00:13 Greater than 65% of persons older than 80 may have quite a number of these seborrheic keratosis or keratoses. 00:24 Thought to be inherited in an autosomal dominant fashion It could be inherited in terms and with cherry angioma also being associated. 00:34 Possesses absolutely no malignant potential. 00:37 The sign of Leser-Trélat is a rare paraneoplastic disorder Abrupt appearance of multiple seborrheic keratoses, Associated with a variety of malignancies, including gastrointestinal and lung cancers Seborrheic keratosis in this case, Morphology would be sharply circumscribed. 00:55 Literally like taking a piece of chocolate and putting it on a person’s back. 01:00 We call this stuck on. 01:04 White-yellow, maybe brown in appearance. 01:10 Management: Well, requires really no treatment. 01:14 Seborrheic keratosis, SK, doesn’t require a treatment. 01:18 If inflamed, traumatized or symptomatic, they may be destroyed. 01:22 Seborrheic keratosis not to be confused with seborrheic dermatitis and definitely not to be confused with, later on, we’ll talk about actinic keratosis. 01:33 You see as to how terminologies -- everything in derm. 01:38 Your pathology, acanthotic. 01:41 What does that mean to you? Thickened epidermis with overlying hyperkeratosis, sharply demarcated base. 01:47 It looks like, as I told you earlier, a piece of chocolate that has been placed on the back and therefore if you take a look at the histology here, It will be sharply demarcated because of increased thickness of your keratinocytes. 01:59 Hyperkeratosis, as you can see in the histologic picture here. 02:03 Here, we move on to actinic keratoses or actinic keratosis. 02:07 Pause here for a second and make sure that you know that our topic is actinic keratosis versus seborrheic keratosis. 02:19 So what does actinic keratosis mean to you? This is premalignant. 02:23 Is that clear? Seborrheic keratosis, rally no chance of going on to malignancy. 02:30 So if you’re thinking about malignancy, then you’re thinking about on your skin exposure to UV rays. 02:35 So therefore, actinic keratosis is premalignant caused by UV exposure. 02:40 Have a potential to move on -- Now of the type of skin cancers that we will discuss in this section, which will then include squamous cell cancer, which is our topic, squamous cell cancer of the skin or cutaneous squamous cell is what you must think of actinic keratosis as being premalignant too. 02:59 Is that clear? Clinically feels gritty, like sand paper. 03:05 Remember, as far as the skin is concerned, what kind of cells are these? Squamous cells. 03:10 So therefore, upon exposure to UV rays, maybe premalignant condition such as actinic as you see in the picture here and worst case scenario, unfortunately, may go on to squamous cell cancer of the skin. 03:23 Our first true premalignant condition, actinic keratosis.
About the Lecture
The lecture Seborrheic Keratosis (Seborrheic Eczema) and Actinic Keratosis (Solar Keratosis) by Carlo Raj, MD is from the course Neoplastic Skin Diseases. It contains the following chapters:
- Seborrheic Keratosis
- Actinic Keratoses
Included Quiz Questions
A 79-year-old man presents with multiple asymptomatic brown, sharply circumscribed lesions with a verrucous surface and a "stuck-on" appearance on his back. What is the next step in management?
- No treatment required
- Surgical excision
- Punch biopsy
- Topical steroids
- Topical antibiotics
Which of the following conditions is premalignant?
- Actinic keratosis
- Seborrheic dermatitis
- Seborrheic keratosis
- Cherry hemangioma
- Pyogenic granuloma
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |