Playlist
Show Playlist
Hide Playlist
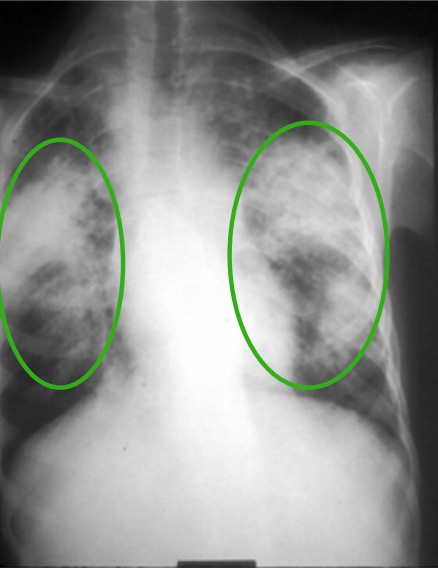
Sarcoidosis: Histological Confirmation
-
Slides 06 ILD InterstitialLungDisease RespiratoryAdvanced.pdf
-
Download Lecture Overview
00:01 Histological confirmation, this is important if somebody has chronic disease. So for the Lofgren's presentation, with bilateral hilar lymphadenopathy and erythema nodosum. If there’s no evidence of disease which is aggressive or problematic such as hypocalcaemia with lung infiltrate associated with it, you probably don’t need to get histological diagnosis and to just wait for the patient to get better. 00:25 However, in those patients who might have TB or might have lung cancer or lymphoma because there’s asymmetry in the lymph nodes or because they’re from a high risk country for tuberculosis, then you may want to actually be sure there’s a sarcoid rather than active TB lymphoma cancer, etc, and that will require biopsy of the enlarged nodes. 00:50 Chronic disease is probably obligatory to get a tissue diagnosis so you know that you’re dealing with sarcoidosis. And the biopsy of the affected tissue should show well-defined non-caseating granulomas. Now, you get granulomas with tuberculosis but in sarcoid, there will be no culture of AFBs, mycobacteria from the sample, and there will be no visible mycobacteria in the sample as well. In addition, sarcoid causes non-caseating granulomas, whereas tuberculosis, it tends to be an area of central necrosis called caseation in the granulomas. 01:25 So, how do you do a biopsy? Well, it depends on the presentation. So with lung disease, we can get biopsies from the bronchi. So the bronchial mucosa often shows infiltration with sarcoid granulomas in patient with sarcoidosis even if it looks normal when you do a bronchoscopy. 01:42 We can do transbronchial biopsies to get tissue from the lung parenchyma. And again, those are frequently positive in patients with sarcoid and lung involvement. 01:52 Thirdly, more recently, we’ve developed the ability to do biopsies of the mediastinal nodes using ultrasound guidance via a bronchoscope so that the needle is passed through the bronchial wall into the affected mediastinal node using ultrasound guidance. And this is a very good way of identifying sarcoid infiltration of mediastinal lymph node, and excluding, importantly, cancer and lymphoma. Now, if somebody presents with extrapulmonary sarcoidosis that actually gives you another range of different things that could be biopsied. So for example, the liver could be biopsied and if somebody has abnormal liver infiltration and potential sarcoidosis, lupus perennial lumps in the skin are very easy and very safe way to confirm a diagnosis of sarcoidosis as are the persons with peripheral nodes or parotid glands. 02:42 So, treatment. Well, actually, most patients with sarcoidosis probably don’t require treatment. If they have stable and non-progressive disease, which is not causing significant physiological upset, then they will not require treatment. And most patients with acute sarcoid will settle without any therapy. However, if you have somebody who has progressive lung impairment or some of the more severe forms of extrapulmonary sarcoidosis, hypercalcaemia, neurological, cardiac, nasal, eye involvement, then they will need treatment with immunosuppresion. 03:20 And the mainstay of therapy is steroids. With medication of immunosuppresants, sarcoid is often at least partially reversible or at least we can slow progression. So as they said, the main form of this treatment is systemic corticosteroids for pulmonary cardiac and neurological involvement. You can use other immunosuppresants. Hydroxychloroquine methotrexate are frequently used. And more recently, severe disease is actually treated with anti-tumour necrosis factor alpha antibodies, and that can be very effective especially for extrapulmonary disease. Overall, the prognosis for sarcoid is generally good. Acute cases will result spontaneously in general, and chronic cases, only a minority will develop severe disabling and damaging disease. So to summarize the main learning points on this lecture of interstitial lung disease, interstitial lung disease are non-infective, non-cancer infiltrations of the alveoli and interstitium. They cause in general restrictive lung disease although some cause a restrictive obstructive picture and a fall in the transfer factor due to reduction of the ability of oxygen to diffuse from the alveoli into pulmonary capillaries. There are multiple causes and these causes are defined by the pathology, which is infiltrating through the lung, and most important causes being the idiopathic pulmonary fibrosis, pulmonary fibrosis developing without a known cause. 04:44 That is connective tissue associated pulmonary fibrosis. That is pulmonary fibrosis associated with a rheumatoid arthritis, systemic sclerosis, dermatomyositis, and other autoimmune rheumatological conditions. 04:57 Hypersensitivity pneumonitis and allergic reaction through inhaled antigen, and sarcoidosis, a granulomatous infiltration of the lungs and extrapulmonary tissue. The diagnosis requires a CT scan, and the CT scan appearance can often give big clues as to what the actual cause of the ILD might be, whether it’s a sarcoid or a hypersensitivity pneumonitis or a normal pulmonary fibrosis. But lung biopsy is occasionally required to confirm that. 05:26 Treatment, in general, is difficult. For example, idiopathic pulmonary fibrosis has a very poor prognosis where there’s only 15% survival over five years, which is much worse than many cancers. Sarcoidosis is the exception that usually has a good prognosis but only a minority of patients developing chronic progressive disease and respiratory failure in long-term. 05:48 Thank you for listening.
About the Lecture
The lecture Sarcoidosis: Histological Confirmation by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Interstitial Lung Disease (ILD).
Included Quiz Questions
Which of the following is NOT a common radiological finding in a patient with sarcoidosis?
- Unilateral hilar mass
- Bilateral symmetrical hilar lymphadenopathy
- Bilateral upper lobe infiltrates
- Normal chest X-ray
Which of the following is the unlikely clinical presentation of a 32-year-old man with confirmed sarcoidosis?
- Constant right-sided chest pain
- Abnormal chest X-ray without accompanying respiratory or cardiac symptoms
- Heart block on the ECG
- Nontender, purple lumps on the skin
Which lab finding constitutes the best evidence to confirm a clinical diagnosis of sarcoidosis?
- Presence of well-defined, noncaseating granulomas in an endobronchial ultrasound guided biopsy of an enlarged mediastinal lymph node
- A raised serum angiotensin-converting enzyme level
- Mixed restrictive/obstructive changes in lung function
- Upper lobe changes on the chest X-ray
Which of the following is the treatment of choice for severe sarcoidosis?
- Systemic corticosteroids
- Antibiotics
- Plasmapheresis
- Chemotherapy
- IV immunoglobulin
Which of the following immune modulators is effective in the treatment of severe sarcoidosis?
- Anti-TNF–alpha antibodies
- Anti-TNF–beta antibodies
- Anti-TGF–beta antibodies
- Anti-IFN–gamma antibodies
- Anti-IFN–alpha antibodies
Which of the following statements is FALSE regarding sarcoidosis?
- Hypercalcemia and eye lesions do not warrant treatment because they spontaneously resolve.
- Angiotensin-converting enzyme levels are a good prognostic indicator towards response to the treatment of disease.
- The overall prognosis of sarcoidosis is good, and most acute cases resolve spontaneously.
- Patients who present with neurological symptoms are considered to have severe disease.
- Stable, nonprogressive sarcoidosis may not require treatment.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |