Playlist
Show Playlist
Hide Playlist
Retinal Detachment
-
Slides OP Retinal Detachment Retinitis Pigmentosa Optic Neuritis.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
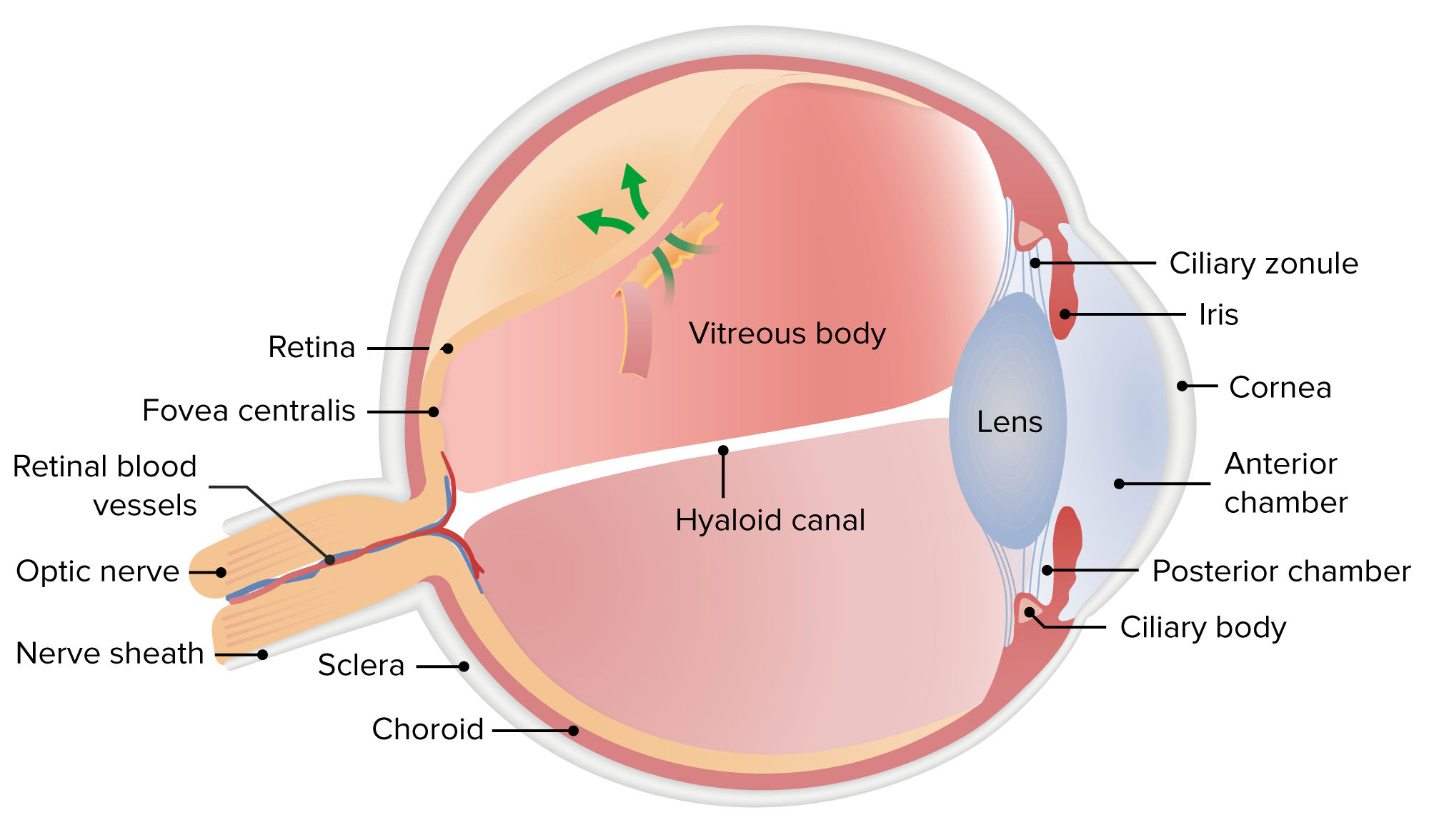
00:02 Welcome back. 00:03 In this session, we're going to talk more about diseases that affect the posterior segment of the eye, particularly things involving the retina and the optic nerve. 00:16 With that, here's where we are, here's what we need to pay attention is at the retina for most of what we're going to be talking about now. 00:24 So the retina is basically the innermost lining all the way around, the ladder, 2/3 of the eye. 00:33 The vitreous body is not a completely liquid thing that sloshes around, it's actually semi gel-like. 00:41 And with time and age, and all this, it can contract and crosslink a little bit so the vitreous slowly shrinks. 00:50 And then it tugs ever so gently on the fibrils, connecting the vitreous to the retina. 00:55 And these are really strongly attached in most cases. 00:58 And as the vitreous shrinks, it pulls away. 01:02 And you see that little bit of detachment near the bottom. 01:05 And really, there's no significance to this other than patients will present with flashes of light, or with new floaters that they hadn't seen previously, and get very concerned and show up to their ophthalmologist. 01:20 It's very common as we age. 01:23 So I can also attest to this. 01:26 I recently had an episode where I had this I was very worried I was going blind. 01:31 When 10, they assured me, pat me on the back, said no, this is posterior vitreous detachment, you're just getting old. 01:38 Anyway, I'm not over 70. 01:40 But it is more common as we age, people over 70 will typically get this. 01:45 And the majority of cases are benign. 01:48 And as the vitreous body slowly shrinks, it kind of gently detaches, it does not lead, it doesn't pull the retina with it in most cases, there are exceptions. 02:00 So now the retinal attachment. 02:03 So the pathophysiology of that is tearing, pulling, separation of the retina away from its underlying choroid and therefore its vascular supply. 02:16 And we are literally going to end up killing that portion of the retina that does that. 02:22 There are two flavors to this. 02:24 There's rhegmatogenous, I love saying that word, rhegmatogenous which means basically there's a tear, retinal detachment, and then there's non-rhegmatogenous retinal detachment, which is just means that an exudate has formed behind the retina and kind of pushed it away. 02:41 So it can be exudative, such as shown there, or tractional, we get scarring of the retina and scar contracts. 02:50 Remember that's part of the normal process of scar reorganization is that it contracts it can pull the retina away. 02:57 Okay, so let's look at these. 03:02 We are going to be basically seen a separation when we talk about retinal detachment that happens between the choroid and then the pigmented retinal epithelial cells, RPE. 03:13 And that line that is showing there is going to be where we typically have the separation and then the retina with all of those nerve cell bodies below are going to pull away. 03:24 In exudative retinal detachment. 03:26 So this is the non-rhegmatogenous version, no tears in the retina or anything like that. 03:32 So there are no retinal breaks, the fluid accumulates beneath the retina, beneath the retinal pigmented epithelium. 03:39 And that accumulation of fluid in that area causes the eventual detachment is just kind of pumping fluid in there and slowly pushes it apart. 03:49 This can happen for a variety of causes such as indicated. 03:52 Age-related macular degeneration is one. 03:55 And that age-related macular degeneration because of inflammation associated with the accumulation of the drusen can lead to accumulation of fluid. 04:05 Remember, inflammation causes increased vascular permeability, so we can get in a fusion that accumulates in that space and causes the separation. 04:14 Trauma can clearly do that we can just yank on it or have sudden deceleration trauma that can lead to retinal detachment. 04:22 Inflammation, again, of any sort, not necessarily associated with AMD, the age-related macular degeneration, but any sort of inflammation in that location can lead to the accumulation of fluid that will cause separation. 04:36 And clearly tumors in that location. 04:39 Unfortunately, retinal blastoma and things like that can cause an exudate that will cause a separation or retinal detachment. 04:48 Tractional non-rhegmatogenous retinal detachment is going to be because of scar tissue, so we have some scarring of the retina. 04:56 And again, once you have scarring, scarring doesn't just lay down collagen and stay there, over time it remodels with matrix metalloproteinases and tissue inhibitors and metalloproteinases. 05:08 All the things we've talked about when we talk about pathology, that scar tissue, as it contracts will cause the retina to pull away and detach. 05:18 This can be associated with, for example, diabetes. 05:20 And I refer you back to an earlier session where we talked about diabetic retinopathy can also be related to trauma, injury, scarring, and then subsequent contraction of that scar. 05:32 So that's the non-rhegmatogenous variety. 05:38 The rhegmatogenous retinal detachment is the most common. 05:42 And this occurs because we have a tear in the retina. 05:45 And fluid can get through that tear, that semi jellied material that's in the vitreous chamber can also transudate into that. 05:56 And clearly with tears, we're also going to incite trauma to the underlying vasculature. 06:02 So trauma will do this. 06:04 Posterior vitreous detachment of the most of the time, thank goodness. 06:08 It's a benign process and just has a slight little kind of pulling away of the viscous material that's present in the vitreous chamber. 06:20 But sometimes it can be more serious. 06:23 Cataract surgery. 06:24 So manipulation of the eye pulling, tugging on the material associated with the vitreous chamber can actually induce a tear. 06:33 Marfan syndrome because we have defective extracellular matrix. 06:37 So we don't have a really good framework for the vasculature and a lot of the connective tissue. 06:44 And then severe myopia. 06:45 So severe myopia will occur when we have a very elongated orbit in the forward-backward dimension. 06:54 And with that severe kind of angulation, and of the kind of orbit shape that can also put abnormal forces and cause a tear. 07:06 So what are the clinical manifestations of retinal detachment? And some of these are the exactly the same as those that we described for the posterior vitreous detachment that's not so bad. 07:16 So that's why you can't just say, "Oh, it's posterior vitreous detachment and not worry about it." Symptoms are very similar. 07:22 So photopsia, that simply means flashes. 07:26 And as we pull away the retina from the underlying vasculature, the little rods and cones are firing away like crazy. 07:33 And so you'll see the abnormal flashes of light. 07:36 The the kind of opaqueness here of the pupil is not, you're not seeing the flashes of light back there, it's flashes of light in your perception in the brain, as a result of pulling away on the retina. 07:49 There will be floaters. 07:50 So we will have inhomogeneities in the retina and you will get new kind of things in your field of vision that float around. 08:00 Because you are pulling the retina away from its blood supply, you'll develop visual field losses. 08:06 And because of the fluid that's now separating the retina, from the choroid you will have distorted vision, you won't have light hitting the retina appropriately, and you'll have blurred vision or loss of central vision. 08:23 So sudden painless loss of vision. 08:27 Particularly if it's also associated with photopsias and floaters, as if there was a descending curtain represents an emergency. 08:34 And we need to get you or the patient who's having these symptoms in as soon as possible to ophthalmologists emergently to reattach that retina so that the neurons don't die. 08:48 What does it look like if we look in through a funduscope? And these are multiple images stitched together by a computer so that you can see what it looks like. 08:57 So the bright little ball, there is the optic disc, the darker little areas going to be our macula and the things that look like curtains floating in the breeze is the detached retina and it moves freely with eye movements. 09:12 Basically, as you move your eye around that viscous material that sitting there in the vitreous chamber is going to kind of sloshing back and forth and you'll see looking like a curtain flowing in the breeze.
About the Lecture
The lecture Retinal Detachment by Richard Mitchell, MD, PhD is from the course Posterior Segment Eye Diseases.
Included Quiz Questions
What are the symptoms of a posterior vitreous detachment?
- Appearance of floaters and flashes
- Disappearance of rods and cones
- Progressive night blindness
- Inability to close the eyes
- Occasional purulent discharge from the eye
Rhegmatogenous retinal detachment results in...
- ...tearing of the retina.
- ...traction on the retina.
- ...exudates from the retina.
- ...inflammation in the retina.
- ...apoptosis of the retina.
What condition is associated with NON-rhegmatogenous retinal detachment?
- Diabetes
- Tuberculosis
- Hodgkin lymphoma
- Hypertension
- Rheumatoid arthritis
What common condition can cause rhegmatogenous retinal detachment?
- Severe myopia
- Hypertension
- Diabetes
- Toxic goiter
- Hyperopia
How does the retinal detachment appear on a fundoscopic exam?
- Like "curtains floating in the breeze"
- Cotton wool spots
- Hard exudate
- Focal yellow retinal lesion
- Blurring of optic disc
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |