Playlist
Show Playlist
Hide Playlist
Renal Losses: Metabolic Alkalosis – Hypokalemia
-
Slides Potassium Disorders Hypo and Hyperkalemia.pdf
-
Reference List Nephrology.pdf
-
Download Lecture Overview
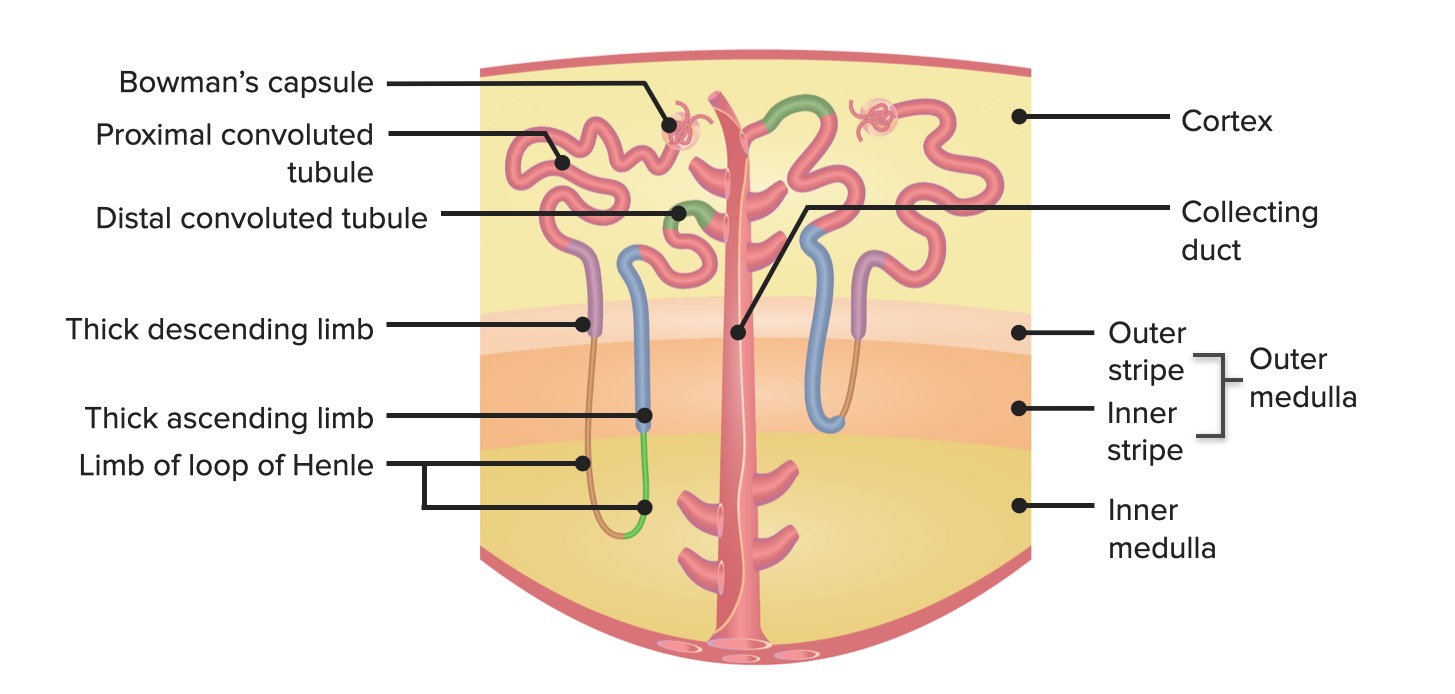
00:01 Alright, so let's move on to renal losses. 00:03 And this is really where all of the money is at. 00:07 So when we think about renal losses of potassium, there's three different categories that we can look at. 00:11 Disorders that are associated with a metabolic alkalosis disorders that are associated with a metabolic acidosis, magnesium which deserves its own little category. 00:22 When you have disorders with a metabolic alkalosis or hypokalemia with metabolic alkalosis, we can further subdivide those into people who present with either hypertension or normal or hypotension. 00:37 So let's discuss that a little bit further. 00:39 So conditions that are associated with a metabolic alkalosis and somebody who either has a normal or low blood pressure are going to include things like diuretics, and these can be Loop Diuretics at the thick ascending limb Loop of henle or thiazide diuretics located that distal convoluted tubule affecting that sodium chloride co-transporter. 01:00 So remember when that happens, what's happening, we've got an increase in distal delivery of sodium to that principle cell and that's the mechanism of potassium secretion into the tubular fluid. 01:12 We're also activating aldosterone by volume depletion, right? We're giving somebody a diuretic they're losing sodium. 01:19 They're losing volume when that happens that activates aldosterone and remember what aldosterone does it increases the number of sodium and potassium channels and turns on that sodium potassium ATPase so that it favors potassium e-flux into the tubular fluid. 01:32 We also have salt-wasting nephropathies. 01:35 This includes bartter's syndrome and gitelman's syndrome. 01:38 Let's take a closer look at those two syndromes bartter's syndrome when you think about that and that happens typically in our pediatric population. 01:45 I want you to think about a loop diuretic because it's almost behaves exactly like that. 01:50 So bartter's syndrome is an autosomal recessive disorder again at presents early in life. 01:54 So my pediatric nephrology colleague see this more than I do. 01:58 This is going to be a defect in sodium chloride reabsorption at that thick ascending limb of the loop of henle. 02:03 So there are three main Transporters that can be involved by mutations. 02:08 The first is the sodium potassium to chloride cotransporter or that NKCC2 which has a loss-of-function mutation. 02:15 And that's also the site of the loop of Loop Diuretics and that shown in the X here. 02:21 The luminol potassium channel can also be involved. 02:24 That's that reno outer medullary potassium channel and remember that's the site where potassium returns and gets recycled by the NKCC2. 02:32 And finally the basaloteral chloride channel can be involved with mutations as well. 02:38 How do our patients clinically present? That's going to be typically with either normal or lower blood pressure. 02:44 Remember they're getting volume depleted slightly because of the fact that they're losing sodium by this mutation. 02:50 They also have impaired concentrating ability. 02:53 So they don't concentrate their urine and it's often times isosthenuric. 02:57 This is because again, they don't have that medullary gradient if they're not reabsorbing sodium at the NKCC2 that's impairing the ability to concentrate their medullary gradient. 03:07 And then of course, they really present with a hypokalemic metabolic alkalosis. 03:12 Why are they hypokalemic? Same mechanism as diuretics. 03:15 If you don't absorb sodium here you have an increase in distal delivery of sodium and tubular flow rate. 03:21 Now how about Gitelman's, Gitelman's really when you think about that I want you to think about a thiazide diuretic because it's very much like that. 03:29 This is going to involve the distal convoluted tubule and the site at where the sodium chloride co-transporter reside. 03:37 It's an autosomal recessive disorder that can present later in childhood or in early adulthood and it's not uncommon for me as an adult nephrologist to actually make this diagnosis in our patients. 03:48 The defect is in the gene encoding that thiazide sensitive sodium chloride co-transporter in that distal convoluted tubule as shown here by the X. 03:56 Now in terms of their clinical presentation. 03:58 These patients also are slightly on the hypotensive side or normal tensive, however, over time, because they have such profound hypokalemia they can actually become hypertensive when they're an adult. 04:12 Similarly, they have an impaired concentrating capacity and they also present with the hypokalemic metabolic alkalosis. 04:18 Now again that hypokalemia is because of that distal delivery of sodium that's going to the principal cell because you're not reabsorbing it at that sodium chloride co-transporter the metabolic alkalosis really comes from activation of aldosterone because these patients remember are losing sodium which is going to turn on aldosterone and we talked about how aldosterone augments potassium secretion, but it also activates that hydrogen atpase. 04:41 Patients here are going to have a low urinary calcium and that's important, I want you to remember that because that's what's going to distinguish gitelman's from Bartter's. 04:51 So I'm going to see that one more time because that really is going to show up on your USMLE. 04:56 The difference in terms of looking at labs in your patients with Gitelman's and Bartter's is that Gitelman's will have a low urinary calcium. 05:04 So let's talk about patients who have a metabolic alkalosis and present with hypertension. 05:12 So these are patients who have mineralocorticoid excess. 05:16 Patients who have primary hyperaldosteronism. 05:18 These can be due to either adrenal tumors or bilateral adrenal hyperplasia. 05:23 Now remember if I'm turning on aldosterone remember what's happening. 05:27 I'm activating my sodium potassium ATPase. 05:29 I'm inserting more sodium and potassium channels in the apical region. 05:32 I am favoring potassium e-flux into that tubular fluid. 05:37 People who have glucocorticoid remediable aldosterone is mm. 05:40 This is one of those things that cause secondary hypertension. 05:43 This is essentially an autosomal dominant disorder that causes ACTH dependent production of aldosterone. 05:49 The bottom line and why it causes hypokalemia, you're turning on aldosterone or you have a mineralocorticoid receptor that is activated and that is going to favor potassium e-flux in the tubular fluid. 06:01 Reno vascular disease, again, one of these secondary hypertension diseases that we have to think about. 06:07 That's due to things like renal artery stenosis that turns on renin due to a decrease in renal artery perfusion. 06:13 Renin will then ultimately lead to aldosterone activation. 06:16 So once again, this is due to aldosterone. 06:19 You can have defects in 11 beta hydroxysteroid dehydrogenase type 2. 06:23 This is responsible for converting cortisol to the inactive form corticosterone. 06:28 When that happens. 06:29 Remember what happens cortisol you have if you have excess cortisol hanging around that can activate mineralocorticoid receptors, and when that happens you're going to favor again potassium e-flux into that tubular fluid. 06:41 Black licorice especially European black licorice contains an enzyme that also turns this pathway on so that you cannot convert cortisol to its inactive form. 06:51 Again, you have mineralocorticoid receptor activation. 06:55 And finally apparent mineralocorticoid excess, again, a similar phenomena, finally, congenital adrenal hyperplasia with 11 beta hydroxylase deficiency has precursors that activate those mineralocorticoid receptors and once again, you have potassium e-flux into that tubular fluid. 07:13 Now another thing to think about when patients present with a metabolic alkalosis hypokalemia, and hypertension is little syndrome. 07:21 Little syndrome is an autosomal dominant disorder and it affects the principal cell. 07:27 So specifically, it works at the epithelial sodium channel presents during adolescence and early adulthood and it is a gain of function mutation in that epithelial sodium channel, which is what I have outlined here. 07:39 You have excessive because of that excessive sodium reabsorption. 07:43 So if I'm reabsorbing and I'm turning on that epithelial sodium channel remember what I'm doing, I am leaving a negative charge behind because chloride always lags behind in its reabsorption. 07:54 So because of that electrical gradient, then I am going to favor potassium e-flux and that Triad of how that patient is going to clinically present is with hypertension a slight metabolic alkalosis and hypokalemia.
About the Lecture
The lecture Renal Losses: Metabolic Alkalosis – Hypokalemia by Amy Sussman, MD is from the course Potassium Disorders: Hypo- and Hyperkalemia.
Included Quiz Questions
Which of the following statements is true regarding salt-wasting nephropathies?
- Patients with salt-wasting nephropathies have low urine osmolality because of the loss of the medullary gradient.
- Patients with Bartter syndrome have decreased urinary calcium excretion.
- Salt-wasting nephropathies usually present in the pediatric age group with hypertension and metabolic alkalosis.
- Patients with Gitelman syndrome have similar clinical features to patients receiving loop diuretics.
- Patients with Bartter syndrome have a gain-of-function mutation in one of the channels of the thick ascending limb.
Which of the following is associated with Liddle syndrome?
- A gain-of-function mutation in the epithelial sodium channels (ENac)
- Effects on the intercalated cells of the collecting duct
- The typical triad of hypertension, metabolic alkalosis, and hyperkalemia
- An acquired condition caused by licorice intake
Which of the following is characterized by low aldosterone levels?
- Syndrome of apparent mineralocorticoid excess
- Bilateral adrenal hyperplasia
- Glucocorticoid remediable aldosteronism
- Renal artery stenosis
- Adrenal adenoma
Which of the following typically presents with hypertension, hypokalemia, and metabolic alkalosis?
- 11-hydroxylase deficiency
- 21-hydroxylase deficiency
- Bartter syndrome
- Gitelman syndrome
- Fanconi syndrome
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |