Playlist
Show Playlist
Hide Playlist
Rapidly Progressive Glomerulonephritis (rpgn) & Subtypes
-
Slides KidneyDisorders RenalPathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
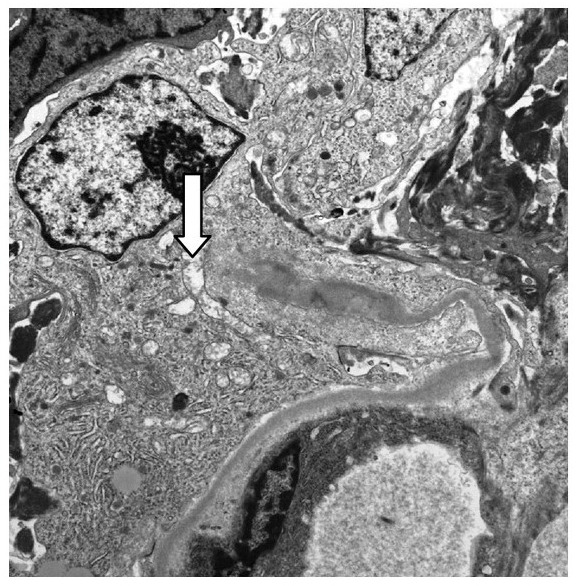
00:00 Now, once again, let me make sure we’re clear. 00:03 Two definitions, so that picture that I showed you, light microscopy with crescentic proliferation, remember, that is a syndrome so you could have many, many, many causes that may lead into it. 00:13 Nephritic always is where you’re coming from, tell me about your patient and presentation, hypertension, hematuria, RBC casts, we have many dysmorphic RBC, we have oliguria, and with nephritic is where I’m coming from and how quickly will the kidney die? 12 weeks. 00:31 Now, if you missed this question, I will come out and find you, and slap you silly. 00:34 Twelve weeks is rapid. 00:37 This is not acute renal failure, completely different definition and then, we’ll go into chronic later on. 00:43 Patients present with nephritic, everything we just said, H&E, light microscopy, we’ll show you Bowman’s space which has completely been occupied by crescentic cells which does what? Restricts and compresses the glomerular tuft, prognosis, poor, and go into end stage renal failure really quick. 01:02 Now, with RPGN, there are different types that we’ll talk about. 01:05 Now, it is not important for you to know type one, type two, type three, that’s not what’s important. 01:11 However, what I’d recommend and what we have in medicine is that type one RPGN include these diseases. 01:19 Type two will include more and type three will be even more. 01:23 What I would also do is because it’s impossible in my opinion to memorize everything at one time. 01:29 So what you wanna do is take a look at type one and give yourself an organization pattern, isn’t that much more effective? So type one, RPGN, perhaps it’s anti-glomerular basement membrane disease is what the patient had. 01:42 Who is your patient? Young patient, 20’s maybe, male more likely, and was coughing. 01:51 When coughing, found what? Blood, hemoptysis, also, had hematuria. 01:57 Why? It’s a nephritic, okay. 01:59 Any sinusitis? No. 02:01 Why did I put that in the mix? Sinusitis to you should give you a different diagnosis or have you think about another differential known as, well, once again, you know this being Wegener but now, what is it called? Granulomatosis with polyangiitis, I’ll abbreviate it as being GPA just to make our lives easy, I’m going to keep repeating that until it becomes part of your unconscious reflex. 02:25 Next, what else? It could be idiopathic, it could be, well, as you we said, Goodpasture. 02:31 Under type two, the category is, well, these are causing RPGN. 02:35 With type two, these are immune-complex diseases. 02:39 Let me walk you through this and you tell me where these immune-complex are located on your otomicroscopy. 02:45 Ready? Postreptococcal, postreptococcal infectious glomerulonephritis. 02:50 Where did it come from? Two places, pharynx or skin. 02:56 Give yourself an approximation of two to four weeks. 02:59 Later your child may be perhaps presented with hematuria. 03:04 Remember some of the streptozyme tests and some of them included anti-DNase B that want the skin which is 60% of the time they’ll present with PSGN will come from the skin and at least, give yourself S as in skin, S as in streptokinase being frequently found as being a streptozyme test. 03:24 Next, tell me about the immune-complex, where is it? Use the P to your advantage, subepithelial, good. 03:31 Pattern on immunofluorescence, granular. 03:34 Another one with a deposit, SLE. 03:39 What kind of stain or marker would you find with kidney damage? How many kidneys? Two, anti-double stranded DNA, good. 03:50 What is the prototype that you’d find here with SLE? It’s called DPGN, diffuse proliferative glomerulonephritis. 03:59 How are you gonna use that D for immune-complex? D as in subendothelial, clear? Once again, what kind of pattern on immunofluorescence? Granular, excellent. 04:11 Let’s move on to Henoch-Schonlein purpura, what’s a better name for this? IgA nephropathy? No. 04:19 IgA nephropathy or glomerulopathy is Berger, IgA vasculopathy is Henoch-Schonlein. 04:28 How can you make that differentiation? What does purpura mean to you? Damaged blood vessel, fibronoid necrosis, bleeding, purpura, IgA vasculopathy. 04:40 Are all of these dealing with immune-complexes? Sure they are. 04:43 You tell me how HSP, Henoch-Schonlein, is then affecting the kidney. 04:48 Could you get IgA deposition in the mesangium with HSP? Of course, you can. 04:53 Could all of these result in RPGN? That’s the point, isn’t it? Let me go into type three. 05:00 Type three that may result in RPGN, these will be Pauci-immune. 05:05 What’s Pauci mean? Pauci means little, okay, pauci means little. 05:09 So you have little immune involvement, but you are ANCA positive and when the time is right, we’ll talk about anti-neutrophil cytoplasmic antibodies being positive. 05:19 Now, the one that you all - well, you must know both of these but the one that you all know so well is granulomatosis with polyangiitis. 05:26 It was formally known as - good, Wegener. 05:30 What else do you wanna know as far as current day practice is that you know this being c-ANCA positive, don’t you? What’s the third letter of the alphabet? Ah, A, B, C, oh, wow, that’s letter C. 05:42 There it is. 05:43 So therefore, antiproteinase three, ANCA positive. 05:49 That’s a lot of words that you need to know and yes, you do need to know. 05:53 Microscopic polyangiitis, p-ANCA positive.
About the Lecture
The lecture Rapidly Progressive Glomerulonephritis (rpgn) & Subtypes by Carlo Raj, MD is from the course Glomerulonephritis.
Included Quiz Questions
Which of the following MUST include the clinical definition of rapidly progressive glomerulonephritis?
- Rapidly progressive renal failure in 4-12 weeks
- Proliferation of visceral epithelial cells
- Tubular dysfunction
- Chronic renal failure
- Acute renal failure
Proliferation of which cell type is responsible for “crescentic” rapidly progressive glomerulonephritis?
- Parietal epithelial cell
- Visceral epithelial cell
- Fenestrated cells
- Endothelial cell
- Mesangial cell
Which of the following is NOT a potential etiology of rapidly progressive glomerulonephritis?
- Minimal change disease
- Post-streptococcal glomerulonephritis
- Goodpasture syndrome
- Granulomatosis with polyangiitis
- IgA nephropathy
Which of the following statements about type 1 RPGN is CORRECT?
- It represents anti-GBM disease
- It presents with granular deposits on immunofluorescence
- It most commonly affects the elderly
- It may be diagnosed using electron microscopy
- It involves IgM deposition on the GBM
In a patient presenting with hematuria, which of the following signs or symptoms would lead you to suspect RPGN?
- Fibrin crescents with H&E stain on light microscopy
- Negative findings on immunofluorescence
- Polyuria
- Proteinuria > 3.5 g/day
- Lack of RBC casts in the urine
In terms of type 2 RPGN, which one of the following statements about immune deposition is INCORRECT?
- Henoch-Schonlein purpura associated type 2 RPGN involves IgM complex deposits.
- SLE-associated type 2 RPGN involves subendothelial deposits.
- Infectious etiologies for type 2 RPGN usually involve subepithelial deposits.
- Type 2 RPGN involves the deposition of preformed immune complexes.
What antibody is commonly associated with microscopic polyangiitis?
- Anti-myeloperoxidase
- Anti-proteinase 3
- Anti-dsDNA
- Anti-saccharomyces cerevisiae
- Cytoplasmic antineutrophil cytoplasmic antibodies
Which of the following antibodies is associated with Granulomatosis with polyangiitis?
- Anti-proteinase 3
- Anti-dsDNA
- Anti-CCP
- Antiphospholipid antibodies
- Anti-thrombin antibodies
Which of the following statements about the immune complex deposition in type 2 RPGN is CORRECT?
- SLE-associated type 2 RPGN, subendothelial deposition
- Post-infectious-associated type 2 RPGN, subendothelial deposition
- Henoch-Schonlein purpura associated type 2 RPGN, IgM deposition
- Henoch-Schonlein purpura associated type 2 RPGN, IgG deposition
- SLE-associated type 2 RPGN, subepithelial deposition
Which of the following types of immune deposition is characteristic of Goodpasture's syndrome?
- Linear deposition of IgG and C3 on GBM
- Granular deposition of subepithelial immune complexes
- Granular deposition of subendothelial immune complexes
- IgA deposition in the mesangium
- Granular deposition of intramembranous immune complexes
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Dr Raj is the best! he makes anything easily understandable! also his sense of humor is amazing and is adding to the lecture's quality!
The best teacher , his sense of humor make the lectures more fun