Playlist
Show Playlist
Hide Playlist
Radiculopathy
-
Slides Diseases of the Spinal Cord.pdf
-
Download Lecture Overview
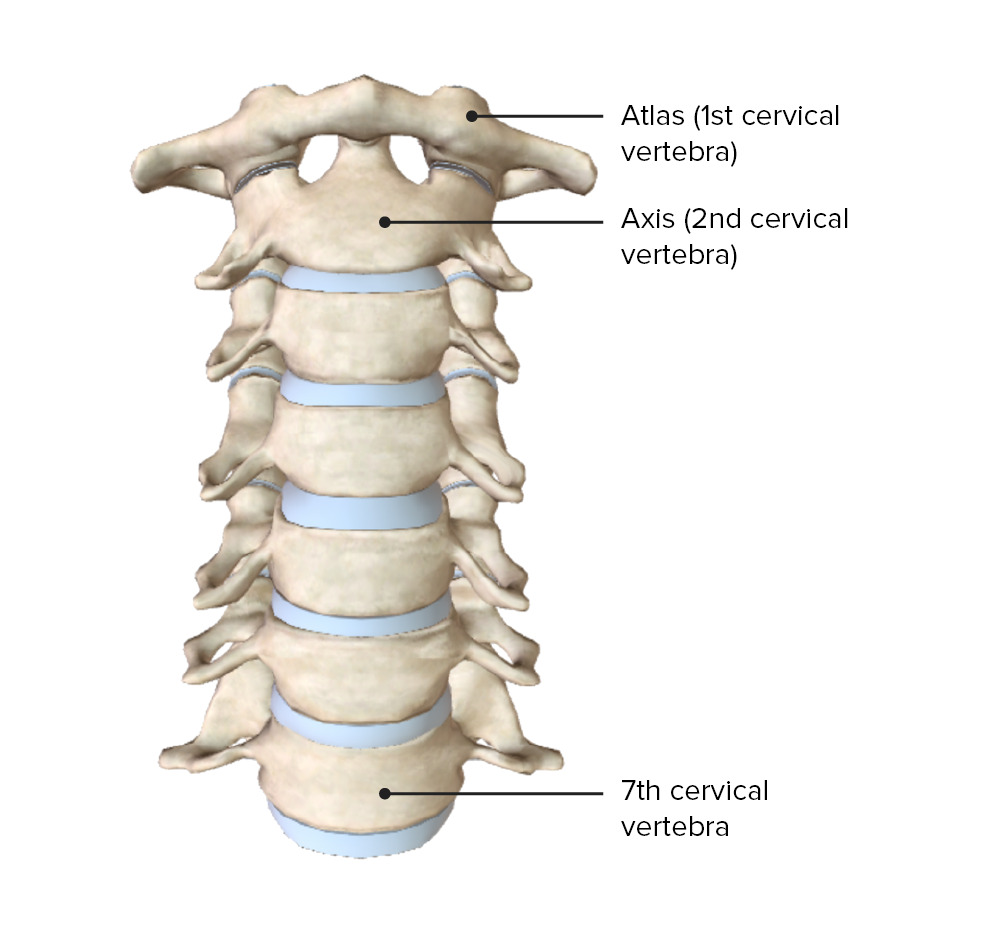
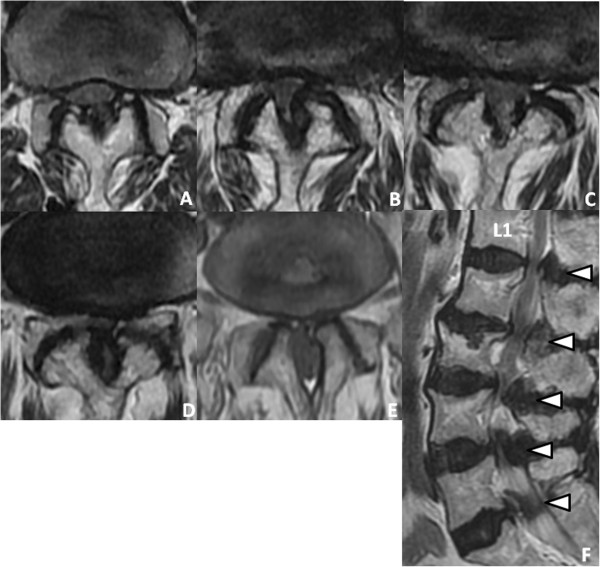
00:00 And this is the typical presentation of a patient with a lumbosacral radiculopathy. 00:07 So let's talk a little bit about radiculopathy, how we diagnose and understand and think about nerve roots impinging or damage the nerve roots or radiculopathy. 00:18 To do so, we're going to start with reviewing the anatomy of the spinal cord and spinal column. Well, remember that the spinal column is broken down into segments; cervical, thoracic, lumbar, and sacral. There are 8 cervical segments, 8 cervical nerves, and only 7 cervical vertebrae and you can see that here. 12 thoracic segments, 5 lumbar segments, 5 sacral segments, and 1 coccygeal segment. The spinal column is made up of vertebral bodies and in between those interspersed are the intervertebral disc material. Note that C1-7 nerve emerge above their respective vertebrae, but there is more nerve than there are cervical vertebrae. So the C8 nerve emerges between the 7th cervical vertebrae and the 1st thoracic vertebrae and this important anatomy will help to inform which disc degeneration will affect which nerve dermatome and myotome. So the remaining nerves C8 and below emerge from below their respective vertebrae. When we think about the vertebral column and vertebral body bony anatomy, this schematic reminds us of the key and important structures. 01:41 There is a posterior vertebral arch and an anterior vertebral arch that form the spinal column. The posterior vertebral arch is made up of the spinous process and 2 lamina that attach to the facet joints. Anteriorly, we see the vertebral body and the pedicles attaching to the lateral transverse processes and the spinal cord is in the middle. 02:04 When we look at the sagittal section here, we can see those key bony findings, spinous processes posteriorly, you can see the superior and anterior articular processes which form the joints within the posterior aspect of the spinal column. Transverse processes are extending out or towards us and we see them on cross section and their vertebral body anteriorly, vertebral bodies being connected by the intervertebral disc. Importantly, the neuroforamen is the critical structure through which nerve roots exit. Damage to the intervertebral disc and herniation or thickening of the ligaments around the vertebral bodies can pinch those nerves and result in radiculopathy or damage pinching of the peripheral nerve roots as they exit the spinal column. 02:52 When we think about radiculopathy and nerve root dysfunction, it's important to remember both the dermatomes and myotomes. Nerve roots are entering and exiting the spinal cord at a level, problem affecting those nerve roots will cause sensory symptoms in their respective dermatome and may cause motor symptoms, motor symptoms in their respective myotome. So let's look now at the spinal cord in cross section and look at the association between the bony anatomy and the neural anatomy. When we think about problems affecting the spinal cord and the nerve roots, there are really 3 places that we can see those problems develop. One is a result of rupture of the intervertebral disc or herniated discs. Those often occur laterally, not on the midline, but has the posterior longitudinal ligament is immediately in the midline behind the vertebral body. That lateral extrusion of an intervertebral disc will compress the spinal nerve roots as they exit. We can see thickening of the ligamentum flavum posteriorly, and so damage, degeneration, arthritis posteriorly can manifest with thickening of the ligamentum flavum either compressing lateral nerve roots or even in towards the spinal cord. And then lastly, bone spurs occurring around the neuroforamen may damage the nerve roots or injure compressed nerve roots as they exit the neuroforamen. And so understanding both the axial-sagittal anatomy as well as these typical areas of pathology can help us to evaluate imaging and patient symptoms in those presenting with radiculopathy. Let's look at how that appears on MRI. Here, we're looking at an axial T2 image of the spinal cord, column, and the nerve roots and we're looking at both the left and right exiting nerve root at this level. On the patient's right, we see an open normal neuroforamen. There is no extrusion of an intervertebral disc, there is no thickening or non-significant thickening of the ligamentum flavum. We see an open neuroforamen and nerve exiting on this side. 04:55 On the patient's left, we see significant pathology. You can see here the green arrow demonstrating extrusion of the intervertebral disc towards the neuroforamen and correspondingly we see thickening of the ligamentum flavum in the orange arrow resulting in pinching of this left neuroforamen as that nerve exits and resulting in symptoms of radiculopathy in this patient. This is a left-sided significant or severe neuroforaminal stenosis. The spinal column, spinal cord, and nerve roots inside the spinal column are not affected. This is pathology of the exiting nerve root. So when we think about radiculopathy and associating patient symptoms with imaging findings, we can remember that above C8 the patient's symptoms and nerve root pathology should match. Below C8 and T1, we see a mismatch where the patient's symptoms and the pathology may mismatch. The one exception is that lateral lumbar disc pathology which can affect the nerve root at the same level and this is important for understanding and evaluating patients particularly with imaging.
About the Lecture
The lecture Radiculopathy by Roy Strowd, MD is from the course Diseases of the Spinal Cord.
Included Quiz Questions
Through which structure do the spinal nerve roots exit?
- Intervertebral neural foramen
- Transverse process
- Spinal canal
- Spinous process
- Facet joints
Which structure of the vertebrae forms the anterior border of the spinal canal?
- Vertebral body
- Transverse process
- Intervertebral disc
- Spinous process
- Facet joints
What are the three primary issues that cause neurologic problems affecting the spinal cord and nerve roots?
- Thickening of the ligamentum flavum posteriorly, bone spurs, and herniated discs
- Facet joint hypertrophy, bone spurs, and vertebral body collapse
- Thinning of the ligamentum flavum posteriorly, vertebral compression fractures, and herniated discs
- Meningiomas, bone fractures, and herniated discs
- Tumors, compression fractures, and bone spurs
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |