Playlist
Show Playlist
Hide Playlist
Pulmonary Fibrosis: Signs and Investigation
-
Slides 06 ILD InterstitialLungDisease RespiratoryAdvanced.pdf
-
Download Lecture Overview
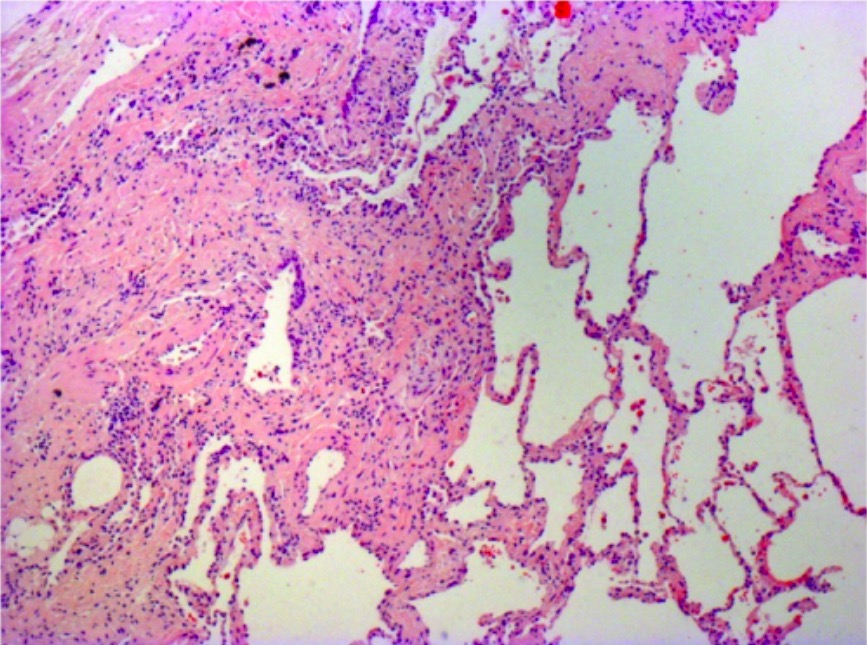
00:00 When you examine the patient, they may be clubbed. Now, this is actually unusual in patients presenting with early fibrosis becomes more obvious for the more severe disease. Chest expansion will be reduced bilaterally but it is quite hard to detect. There is no effect in percussion note or vocal resonance. 00:17 The hallmark of pulmonary fibrosis is an auscultation, where you will hear what we call velcro crepitations. These are fine late inspiratory crepitations that occur in birth. 00:30 That is the description. Normally, because the disease is bibasal, you hear them at the bases. In more severe disease, the patient will be dyspnoeic at rest. They will be centrally cyanosed and the crackles will spread from the bases to affect the whole of the lung. 00:47 In addition, the patient might, due to chronic hypoxia, be developing cor pulmonale and have the signs of cor pulmonale with a raised JVP, oedema, a right ventricular heave, etc. 01:02 Investigations of pulmonary fibrosis, we start off with the chest X-ray which should show reticulonodular infiltrates. Again, because it starts off from the bases, this will be most obvious in the bases and should be relatively symmetrical. However, early pulmonary fibrosis is often quite hard to see on a chest X-ray. It is only when you got extensive diseases, it becomes obvious as seen by this X-ray here. Very important are lung function tests. 01:28 If you have restrictive lung function test with reduced transfer factor, you need to think that the patient may have pulmonary fibrosis or another form of interstitial lung disease. 01:38 So, lung function test is incredibly important for identifying the potential patients with ILDs. The most important test is probably the CT scan. I will discuss that in the next slide or two. Blood tests are used to identify potential causes, and that could be a rheumatoid factor, autoantibodies, or ANCA for people with connective tissue diseases, a serum angiotensin-converting enzyme level to identify somebody who may have sarcoidosis. Avian precipitins, these are antibodies which are detectable in patients who have hypersensitivity pneumonitis in Bird fancier’s lung. You may want to do test to identify differential diagnosis, and the most important of that is probably going to be an echocardiogram to look for people with left ventricular impairment which might indicate they have cardiac disease. In some patients, which I will discuss shortly, you may want to move on to do a bronchoscopy or a lung biopsy.
About the Lecture
The lecture Pulmonary Fibrosis: Signs and Investigation by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Interstitial Lung Disease (ILD).
Included Quiz Questions
Which of the following signs and symptoms are commonly identified in pulmonary fibrosis?
- Bibasal, late-inspiratory, “velcro” crepitations
- Dullness to percussion over lung fields
- Increased chest expansion
- Purulent sputum
- Increased vocal resonance
Which of the following statements regarding pulmonary fibrosis is false?
- Pulmonary fibrosis is seen more commonly in women than in men.
- Pulmonary fibrosis can present with severe dyspnea at rest.
- Pulmonary fibrosis is usually a disease of old age.
- Pulmonary fibrosis can present with clubbing.
- Pulmonary fibrosis can cause cor pulmonale.
Which of the following is NOT a change seen in pulmonary function tests of patients with pulmonary fibrosis?
- Decreased FEV1/FVC
- Decreased FEV1
- Reduced total lung capacity
- Decreased transfer factor for carbon monoxide
Which of the following tests is used to confirm diagnosis of interstitial lung disease?
- CT scan
- Bronchoscopy
- MRI
- Sputum culture
- Sputum microscopy
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |