Playlist
Show Playlist
Hide Playlist
Pulmonary Fibrosis: Clinical Recognition and CT Scans
-
Slides 06 ILD InterstitialLungDisease RespiratoryAdvanced.pdf
-
Download Lecture Overview
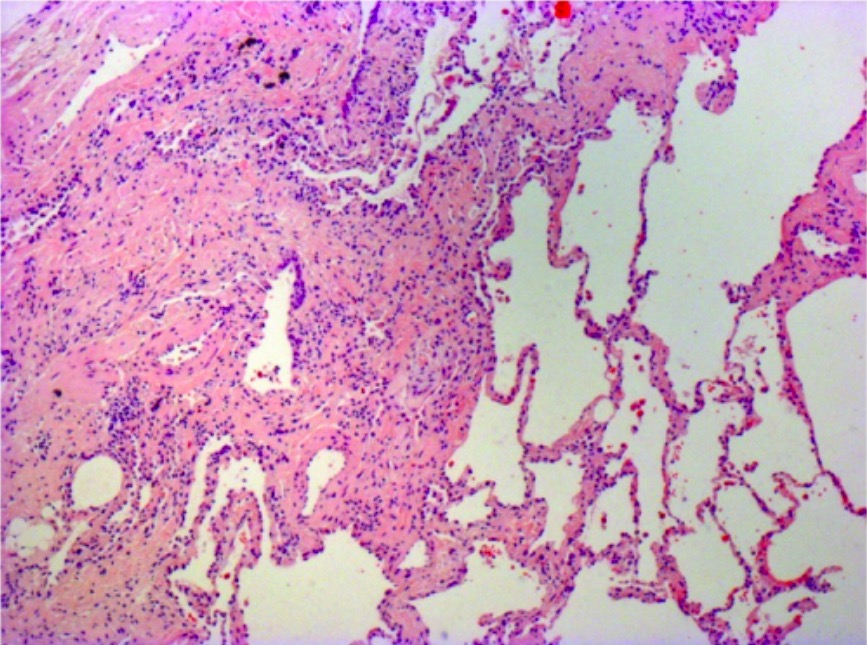
00:01 So, clinical recognition of pulmonary fibrosis, just to rehash on that, it's several weeks or months of exertion of dyspnoea usually progressive getting worse over time. And the presence of fine bibasal inspiratory crackles, what we described as velcro crepitations, plus restrictive lung function and a reduced transfer factor. Those are the three characteristics which identify clinically the patient who is likely to have ILD. And they may or may not have an underlying cause. 00:31 The main differential diagnosis for patients presenting with pulmonary fibrosis is other interstitial lung diseases such as sarcoidosis and hypersensitivity pneumonitis. COPD, in which case, there will be a smoking history, although ILD patients often have smoking history, anyway, but there are no crepitations in patients with COPD. And then congestive cardiac failure, but there should be some signs of abnormal heart function and they should have a background which might suggest that the heart is impaired, such as hypertension, diabetes, previous ischemic heart disease. So the CT scan is fundamental for making the diagnosis. The three dimensional ability of the scan to identify infiltrates in the lung parenchyma is vital to make the diagnosis, and also for telling you what the likely pathology and the likely potential cause there might be for this ILD. So for example, in this slide, we have two CT scans. The top one shows the usual interstitial pneumonitis pattern which is the crispy fibrosis with lots of collagen and fibroblastic infiltration into the lung which has a poorer prognosis and responds less well to treatment. And that shows quite a lot of subreticular intralobular changes and you tend to get honeycombing, which is formation of cyst within the lung in a subpleural and a basal distribution. 01:57 The bottom CT scan shows the NSIP pattern which is the more inflammatory pattern where ground glass infiltrates are more dominant. With fibrosis, you also get what we call traction bronchiectasis where the scarring of the lung tissue causes the bronchi to be pulled apart. The important point here is that the CT scan will define the distribution, and the type of infiltration in the lung give you some indication of histology for patients presenting a pulmonary fibrosis, and help distinguish pulmonary fibrosis from other causes of ILDs such as sarcoidosis and hypersensitivity pneumonitis.
About the Lecture
The lecture Pulmonary Fibrosis: Clinical Recognition and CT Scans by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Interstitial Lung Disease (ILD).
Included Quiz Questions
Which of the following is NOT a typical CT finding in patients with pulmonary fibrosis?
- Cavitation
- Thickened intralobular septa
- Honeycombing
- Traction bronchiectasis
- Ground-glass appearance
A 67-year-old man presents with progressive dyspnea for more than 6 months and bibasalar, fine, velcro crepitations. Which of the following results would contradict the clinical diagnosis of pulmonary fibrosis?
- Raised residual volume and total lung capacity
- A reduced transfer factor
- Restrictive changes on spirometry
- Reduced residual volume and total lung capacity
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |