Playlist
Show Playlist
Hide Playlist
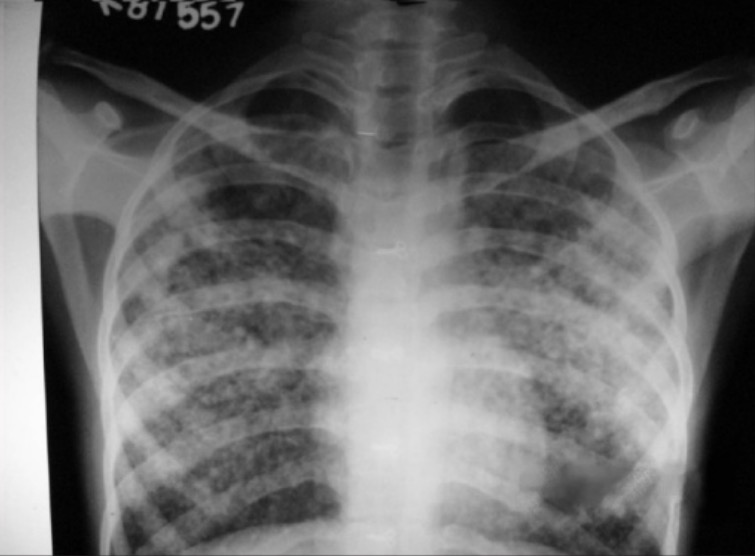
Pulmonary Edema: Underlying Cause
-
Emergency Medicine Bord Pulmonary edema and CHF.pdf
-
Download Lecture Overview
00:01 Now why do patients get this? Why do patients get acute pulmonary edema or decompensated heart failure? There’s a few underlying causes. 00:09 One of them is dietary noncompliance. 00:13 So salt as water and when you’re taking too much salt you can cause increased fluid buildup. 00:20 It’s very important that you ask patients about their diet. 00:23 Are you eating things that are higher in salt than what you normally do? You really sometimes need to get specific with patient. 00:30 So patients will say no, I’m just eating soup. 00:33 Well soup from a can actually has a really high rate or high content of salt. 00:38 Patients may also get more CHF exacerbations around holiday time. 00:45 So for example, if they normally cook for themselves, they know what they’re making, but they go to a friend’s house or a family member’s house for holiday dinner and they have this meal that can be loaded with salt. 00:56 So if you’re working on the Christmas holiday or Thanksgiving, a classic afternoon presentation is that patients will come in with heart failure all the time. 01:05 It never fails. 01:06 You’re working on one of those holidays someone comes in after those meals. 01:10 Medication noncompliance is also a big one. 01:13 Patient’s one of the main medications that they’re maintained on are diuretic medications like furosemide or bumetanide and patients sometimes don’t wanna take these medications because it makes them urinate. 01:27 So for example, a classic thing that we see is an elderly woman who goes to get her hair done or goes out to run errands, she doesn’t wanna have to worry about finding a bathroom or running to the bathroom so these patients just decide not to take their medications. 01:43 Again, you have to be specific with people. 01:45 So the number of times that I’ve said are you taking your medicines to people and they’ve said yes and then I say specifically, are you taking your diuretic medication? And they sheepishly say no happens all the time. 01:58 All the time. 02:00 Patients won't admit that they’re not taking it or they won’t be totally forthcoming with the first question, so ask specific questions. 02:07 I guarantee you that there will be someone who won’t necessarily tell you that they’re not taking their medication on first questioning. 02:14 And then lastly, worsening heart failure. 02:16 Now this is one of the most worrisome concerns. 02:18 So basically what this means is that the patient has had a further decrease in their ejection fraction so that the heart isn’t squeezing effectively even worse than it was before. 02:28 So classically, these patients will have a decreased ejection fraction and what that means is that’s the amount of blood that’s closed in out of the heart or squeezed out of the heart each time the heart pumps. 02:39 Now, in a normal person that’s about 60% so every time our heart squeezes about 60% of the blood will leave it. 02:46 In patients who have heart failure, this number can be much less. 02:49 It can be somewhere along the lines of like 10%, 15%, 20%, so if they have had another heart attack or some kind of change in their physiology, they can have a worsening ejection fraction. 03:01 There are different causes for a worsening heart failure. 03:04 The main causes are easily remembered with this mnemonic champ. 03:10 This means acute coronary syndrome, hypertension, emergency arrhythmia such as atrial fibrillationor or ventricular tachycardia, acute mechanical cause, such as ventricular septal rupture and pulmonary embolism. 03:26 Now patients who present with acute pulmonary edema and decompensated failure will generally be experiencing very severe dyspnea. 03:35 This is gonna be someone who’s gonna come in, who’s gonna be able to speak only one, two word sentences, gonna have a very hard time catching their breath. 03:44 Now once you recognize this and think about it, there are some good, quick interventions that can be done. 03:49 Now this was mentioned in other lectures on shortness of breath here but sitting your patient up is key. 03:55 So sitting your patient up recruits more functional lung tissue and improves oxygenation. 04:00 If your patient has pleural effusions or fluid in the lung cavity, it’ll make the fluid go down and the air go up. 04:07 It’s a very easy and simple maneuver that you can do for your patient.
About the Lecture
The lecture Pulmonary Edema: Underlying Cause by Sharon Bord, MD is from the course Respiratory Emergencies.
Included Quiz Questions
There are several underlying causes for acute pulmonary edema. Which among the following is NOT an underlying cause?
- Intake of diuretic medications
- Excessive sodium intake
- Non-compliance with heart medications
- Increased fluid intake
- Decreased ejection fraction
In the investigation of the possible cause of pulmonary edema in patients with heart failure, which of the following statements is NOT true?
- Patients will always admit on first questioning that they are not compliant with medication
- Worsening of heart failure means a further decrease in ejection fraction
- Asking specific questions regarding the patient’s diet will give you an idea if he is taking too much salt
- Patients usually have heart failure exacerbations during holiday season
- Patients who present with acute pulmonary edema and decompensated heart failure will be experiencing severe dyspnea
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |