Playlist
Show Playlist
Hide Playlist
Paroxysmal Supraventricular Tachycardia (PSVT)
-
Emergency Medicine Tachyarrhythmia.pdf
-
Download Lecture Overview
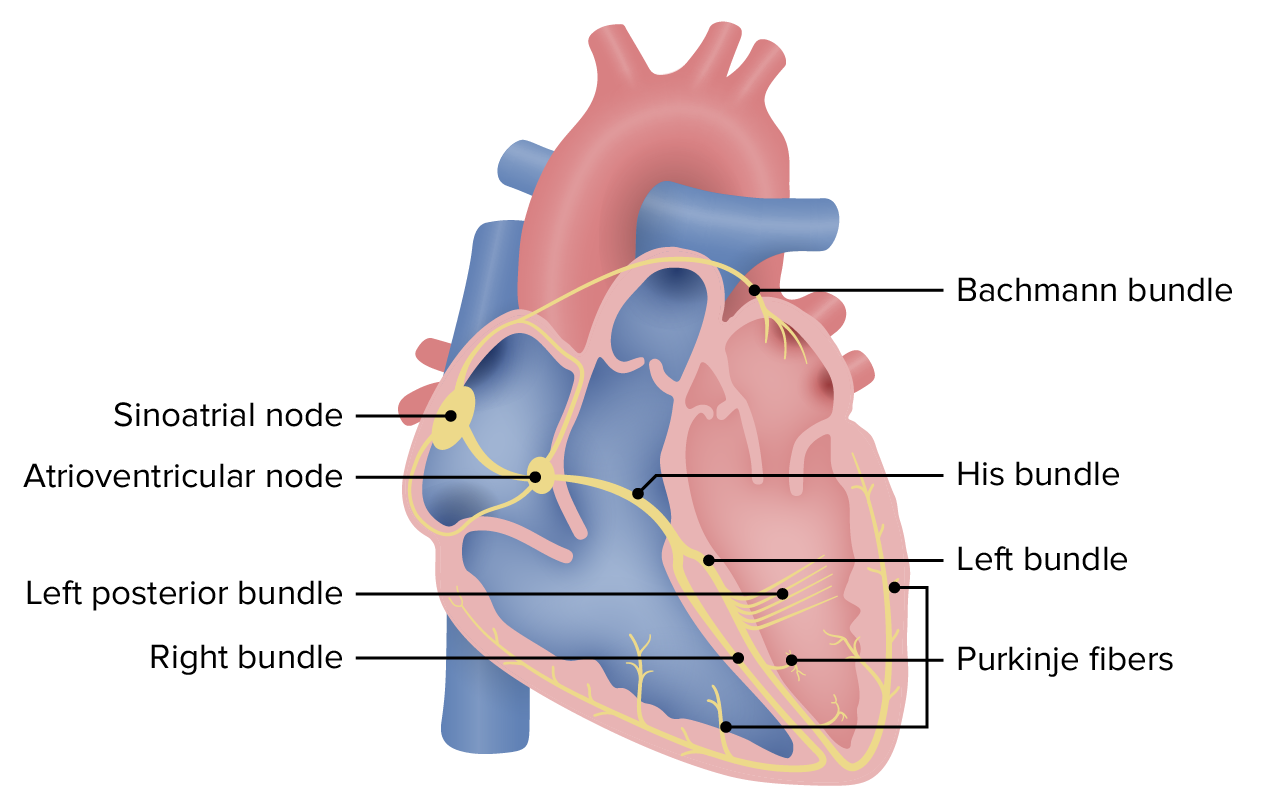
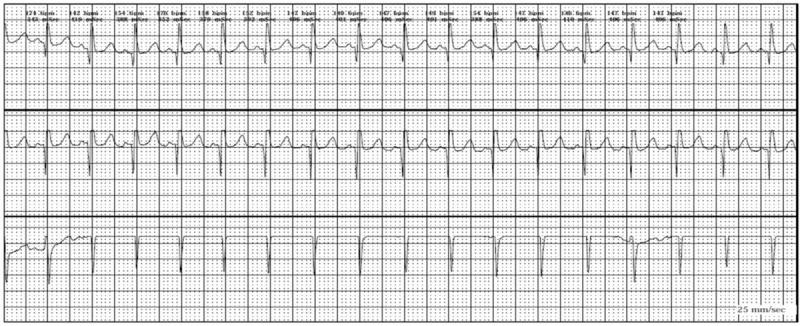
00:01 All right, so we’ve covered our irregular rhythms. 00:04 We’re now gonna move on to our regular narrow complex rhythms. 00:09 So like I said before, when you have a regular narrow complex rhythm, your next question is are there normal P-waves? If there are no normal P-waves present, you're dealing with one of the super ventricular tachycardias. 00:24 So paroxysmal SVT or supraventricular tachycardia is kind of a catch-all term for a few different diagnoses that shares some common pathophysiology. 00:35 So typically, paroxysmal SVTs are triggered by premature atrial beats So the atria for whatever reason contract prematurely and this sets off a cycle that produces a rhythm disturbance. 00:51 There are a number of metabolic risk factors for supraventricular tachycardia Hyperthyroidism, use of stimulants like cocaine, caffeine can trigger SVT, ethanol can do it as well. 01:06 In order to get SVT though in the setting any of these risk factors, you have to have some form of re-entry pathway to be able to maintain this abnormal rhythm. 01:18 So there's a couple common types of SVT, these are not the only ones, but the two most common ones are AV Nodal Reentrant Tachycardia or AVNRT and in AVNRT, you have bidirectional pathways in the AV node. 01:31 So the normal AV node only conducts in one direction, down. 01:35 Down from the atria to the ventricles. 01:38 However, if you have bidirectional pathways that allow conduction back from the ventricles to the atria, you can have a circuit form that basically creates an electrical loop driving very, very fast ventricular rates as electricity goes from the atria to the ventricle and then directly back up from the ventricle to the atrium. 02:01 There’s also AVRT or Atrioventricular Reentrant Tachycardia and in this situation, there is an accessory pathway that creates a loop between the normal AV nodal pathway and the abnormal accessory pathway. 02:17 So how do you diagnose paroxysmal SVT? So first and foremost, you have to have a narrow QRS complex like we said, your QRS has to be less than a hundred and twenty milliseconds. 02:29 You have to have a rapid regular rate. 02:33 So here, you can see the QRS' which I've marked are coming along every seven millimeters. 02:39 So your RR interval is seven millimeters and constant. 02:42 That gives us a rate of about 200. 02:46 And then lastly, you have to have absent or abnormally conducted P-waves So the arrows denote where P-waves should be before each QRS complex but you can see we’re basically just getting QRST, QRST, QRST and we’re not able to see P-waves. 03:03 So these are the diagnostic criteria for SVT. 03:08 What are we gonna do about SVT? Well, one, we’re gonna start off with some non-pharmacologic management. 03:14 So many cases of supraventricular tachycardia can be treated with vagal maneuvers. 03:20 So basically, any maneuver that you perform that increases parasympathetic tone is gonna decrease the heart rate and potentially terminate the SVT. 03:31 So a couple of the maneuvers that are commonly done is the valsalva, so you basically get the patient to hold their breath and bear down as though they’re having a bowel movement and they wanna hold that for 15 or 20 seconds if they can. 03:46 That raises parasympathetic tone and in some cases can terminate the SVT. 03:50 Another vagal maneuver that’s commonly performed is carotid massage. 03:54 Now, before you do carotid massage, you wanna auscultate the carotids and make sure you’re not hearing any bruits and obviously you only wanna do one side at a time because occluding both carotids at once is not a good idea. 04:06 What you're gonna do is put your fingers over the carotid artery high up in the neck and you're gonna apply firm but gentle pressure continually for about 15 or 20 seconds. 04:18 Again, this will raise parasympathetic tone and might terminate the SVT. 04:23 If your vagal maneuvers don't work and by the way, for patients who have a history of paroxysmal SVT in the past, they typically learn these maneuvers and will have attempted them at home before the even come into the hospital. 04:36 But if vagal maneuvers don’t work, of course, you’re gonna cardiovert your patient if they’re unstable but your initial medical management is gonna be adenosine. 04:44 Now, adenosine works by completely blocking conduction through the AV node for a very short period of time, about three to five seconds is its plasma half-life. 04:55 So it completely blocks nodal conduction but the effect of it goes away very, very quickly. 05:02 One of my favorite cardiology mentors when I was an intern described adenosine to me as control-alt-delete for the heart. 05:08 So basically, what you're doing is just shutting down all of the wacky electrical conduction pathways and hoping that the normal pathways will take back over when you restart. 05:19 If adenosine doesn't work, were gonna move on to AV nodal blocking agents. 05:23 Again, calcium channel blockers, beta blockers can be helpful for refractory cases. 05:29 They basically will block conduction through the AV node and hopefully decrease the ventricular rate. 05:37 I do wanna emphasize again, that these agents are contraindicated in wide complex tachycardia. 05:44 In situations like WPW, remember, your AV nodal blocking agents are not gonna block your accessory pathway and they could potentially accelerate your tachycardia. 05:55 So in wide complex rhythms, please do not give calcium channel blockers or beta blockers 'cause they can be very harmful. 06:03 All right, our last scenario is our regular, narrow, complex rhythm and if you have normal P-waves, you’re dealing with a sinus tachycardia. 06:17 So just a quick review on sinus tach, your rhythm is gonna be regular so your RR interval is gonna be the same from beat to beat, to beat, in this case 11 millimeters. 06:27 You’re of course going to have a narrow QRS complex and you're gonna see a P-wave preceding every single QRS and you can see that denoted here. 06:36 PQRS, PQRS all coming along at a regular rate. 06:43 I wanna emphasize that sinus tachycardia is not a dysrhythmia. 06:47 It's not a disease on to itself to be treated. 06:50 It’s a symptom of some other underlying problem. 06:53 There is some physiologic derangement that’s driving the tachycardia and your goal should not be to slow down the heart rate, it should be to identify and treat that underlying problem. 07:06 So in summary, I'll just remind you of a couple of key points about each rhythm we talked about. 07:12 Ventricular tachycardia is a wide complex rhythm with which patients should be cardioverted if unstable, otherwise, they can be managed medically. 07:22 And again, all wide complex tachycardia is vtec until proven otherwise. 07:28 Atrial fibrillation is our narrow, complex irregularly irregular rhythm. 07:34 Again, we're gonna cardiovert unstable patients but the mainstay of management is gonna be AV nodal blockers like calcium channel or beta blockers Atrial flutter, we identify by the saw tooth atrial waves and the management is the same as it is for atrial fibrillation. 07:50 And then lastly, paroxysmal SVT is characterized by a narrow QRS complex, a regular rate, and absent or abnormal P-waves. 08:01 Once again, cardioversion for any unstable patient but the mainstay of medical management is gonna be adenosine. 08:10 So once again, if the patient’s unstable, cardiovert them. 08:14 If they have hypotension or shock, altered mental status, ischemic chest pain, or evidence of acute heart failure, you wanna make sure you terminate that rhythm quickly. 08:24 Sinus tachycardia is always gonna be treated by addressing the underlying cause so please, never treat sinus tachycardia as a primary rhythm disturbance. 08:33 Thank you very much.
About the Lecture
The lecture Paroxysmal Supraventricular Tachycardia (PSVT) by Julianna Jung, MD, FACEP is from the course Cardiovascular Emergencies and Shock.
Included Quiz Questions
Which of the following differentiates sinus tachycardia from supraventricular tachycardia?
- Normal P waves
- Regular rhythm
- Narrow QRS complex
- Rate > 100 beats per minute
- Supraventricular origin
Which of the following is NOT a pathophysiologic mechanism of paroxysmal supraventricular tachycardia?
- A re-entry pathway is not required for maintenance.
- It is commonly triggered by premature atrial beats.
- It can be induced by hyperthyroidism.
- It can be induced by stimulants.
Which of the following is NOT a management for SVT?
- Decreasing parasympathetic tone
- Vagal maneuvers
- Cardioversion if unstable
- Adenosine
- Calcium channel or beta blockers
Which of the following statements regarding abnormal rhythms is INCORRECT?
- Normal P-waves are present in paroxysmal SVT.
- Management of unstable atrial fibrillation is cardioversion.
- Wide QRS complex is ventricular tachycardia until proven otherwise.
- Sawtooth atrial waves are characteristic of atrial flutter.
- Anticoagulation in atrial fibrillation is based on risk for embolization.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Thank you for your excellent lectures Dr Julianna Jung! Both clinically relevant, and easy to understand!