Playlist
Show Playlist
Hide Playlist
Prostatitis and Prostate Cancer: Pathophysiology
-
Slides Testicular Neoplasms and Prostate-Male Reproductive Pathology.pdf
-
Reference List Pathology.pdf
-
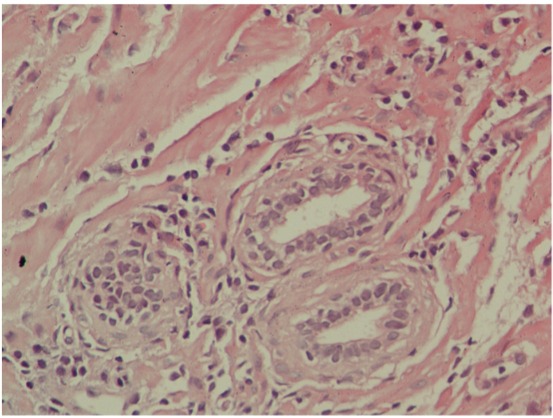
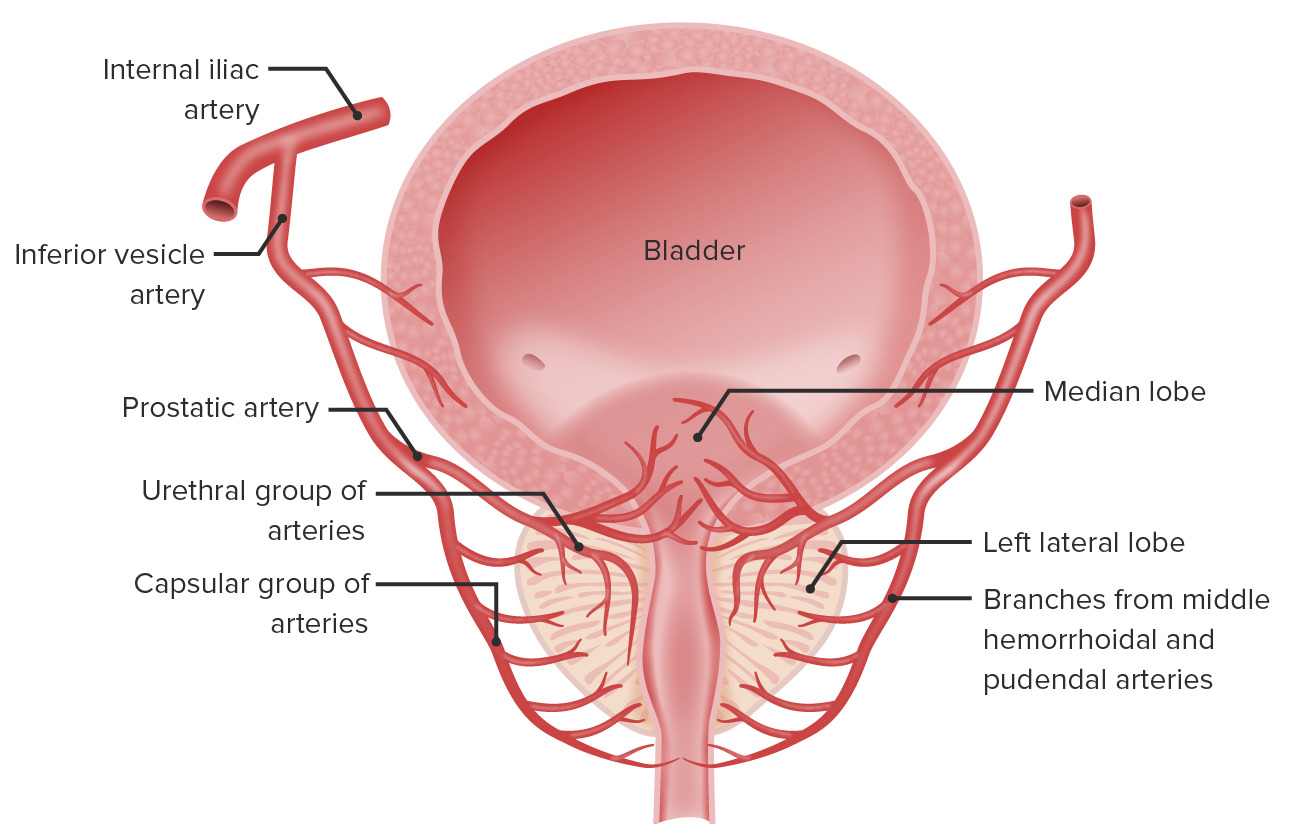
Download Lecture Overview
00:02 Our topic is prostate pathology. 00:05 I’ll walk you through some infections and I’ll walk you through BPH and then finally get into what’s known as your prostate cancer. 00:12 I’ll begin our discussion by looking at acute bacterial prostatitis. 00:17 Think about the prostate and now there might be infection. 00:22 So now with this infection, how is the patient going to present? Lower back pelvic pain. 00:27 Do not confuse this with pyelonephritis or urinary tract infection. 00:34 Keep it as a differential. 00:36 In a male, the prostate should come to mind. 00:39 Dysuria, frequency, tender, warm, enlarged prostate. 00:45 Dysuria, frequency, what about that? Be careful, do not confuse this with BPH. 00:51 Okay. 00:51 So two differentials with the first two presentations. 00:55 Lower back pain, maybe pyelonephritis being a differential or urinary tract infection with suprapubic pain. 01:03 Or number two here, with frequency as a differential, BPH. 01:08 How can you rule out one from the other? The next statement. 01:11 Upon digital rectal examination, warm, enlarged prostate. 01:16 DRE. 01:17 Digital rectal. 01:19 Warm, enlarged, what does it feel like? See my big nose? You press on big nose and it’s kind of soft and boggy. 01:29 That’s protatitis. 01:31 If it feels like my ugly chin and it’s gritty, that’s not good. 01:35 That’s prostate cancer. 01:38 Next, etiology, sexually transmitted infections such as gonococcal, Chlamydia, usual suspects. 01:43 And BPH with what’s known as coliform or E. coli in elderly. 01:49 Understand the statements here. 01:50 Pathogenesis: Young patient with sexually transmitted infection. 01:54 Uh-oh. 01:55 Acute bacterial prostatitis. 01:57 If you have a male who’s older, 67-72, has frequency and you don’t find an increase in PSA and you can’t feel any prostate issues because this is BPH, imagine now if there’s frequency and unable to properly void when he goes to the bathroom. 02:19 The perfect nidus or environment for urinary tract infection, E. coli, E. coli, E. coli. 02:24 Here comes the E. coli, up the urethra, climbing up the urethra, causing prostatitis. 02:33 Antibiotics are used to treat this infection. 02:35 Chronic prostatitis: What’s interesting when you go into practice and, you know, you’re going through internal medicine, so on and so fourth. 02:44 And then you suspect prostatitis, oftentimes, you’ll find a chronic prostatitis being an issue, very common. 02:52 And what’s amazing, is the fact abacterial chronic prostatitis is the most common. 02:58 Even though we call it abacterial, we just don’t have the proper tools to maybe perhaps diagnose the infection. 03:06 Important, chronic. 03:08 Our topic is BPH. 03:10 With benign prostatic hyperplasia, who’s your patient? BPH is commonly seen in men over age 50, but it can be asymptomatic and only requires treatment if it is bothersome to the patient. 03:21 The enlarged prostate is palpable on digital rectal exam; however, the size of the prostate on exam does not correlate with symptom severity. Clinical presentation may include urinary frequency, inability to empty the bladder completely, urinary dribbling, and an increase in nocturia with patients having to get up to urinate several times during the night. 03:41 BPH can also increase the risk of urinary tract infection of the bladder in older men. Management can be with alpha-blockers, phosphodiesterase type 5 inhibitors, 5-alpha reductase inhibitors or surgery. Some alpha-blockers such as terazosin and doxazosin are also used to treat high blood pressure Prostate adenocarcinoma. 04:02 You may notice an asymmetric enlargement of the prostate or nodule on digital rectal exam. 04:07 This is an adenocarcinoma. 04:08 What does that mean to you? Glandular, glandular, glandular. 04:12 Isn’t that what the prostate does? It secretes fluid into the seminal vesicle, mixes it all up and then when the time is right, what have you? Erection, ejaculation, emission, so on and so forth. 04:24 But adenocarcinoma, it’s glandular. Glandular. 04:27 As far as you’re concerned, you’ll be paying attention to PSA. 04:31 What if you also find increase in alk phos? Uh-oh. 04:36 PSA and alkaline phosphatase, why was I so dramatic about that? Because now, the prostate cancer has metastasized from the prostate to the vertebrae through your Batson paravertebral plexus. 04:50 And now, upon your x-ray, what does this bone look like? Hot. 04:54 What does hot mean? Clinically hot then means that it’s opaque and white. 04:59 It’s an osteoblastic type of metastasis. 05:02 Prostate adenocarcninoma, you can feel it, increased PSA. 05:08 Always look to see as to whether or not there is metastasis.
About the Lecture
The lecture Prostatitis and Prostate Cancer: Pathophysiology by Carlo Raj, MD is from the course Male Reproductive System Diseases.
Included Quiz Questions
Which of the following is NOT usually seen in a patient with acute bacterial prostatitis?
- Firm, nodular prostate on digital rectal exam
- Warm, tender prostate gland
- Urinary frequency
- Dysuria
- Lower pelvic/back pain
Which of the following statements is TRUE about benign prostatic hyperplasia (BPH)?
- With BPH, patients present with urinary frequency.
- An elevated PSA is not seen with BPH.
- BPH can increase the risk of prostate cancer.
- The main treatment for BPH is surgery.
- BPH mainly affects the peripheral part of the prostate.
What is the most appropriate drug class used to treat benign prostatic hyperplasia in a patient with hypertension?
- Alpha-blockers
- Antibiotics
- Testosterone
- 5-alpha reductase inhibitor
- Beta-blockers
Which of the following statements about prostate cancer is NOT true?
- Metastatic lesions are characteristically osteolytic.
- It is a glandular type of cancer.
- Metastatic lesions may be associated with elevated levels of alkaline phosphatase.
- It is associated with an elevated PSA level.
- It may present as a firm prostatic nodule on digital rectal exam.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Great lecture, thanks for using humor in the explanations so we don't get bored!