Playlist
Show Playlist
Hide Playlist
Primary Ovarian Insufficiency (POI)
-
Slides Primary Ovarian Insufficiency.pdf
-
Download Lecture Overview
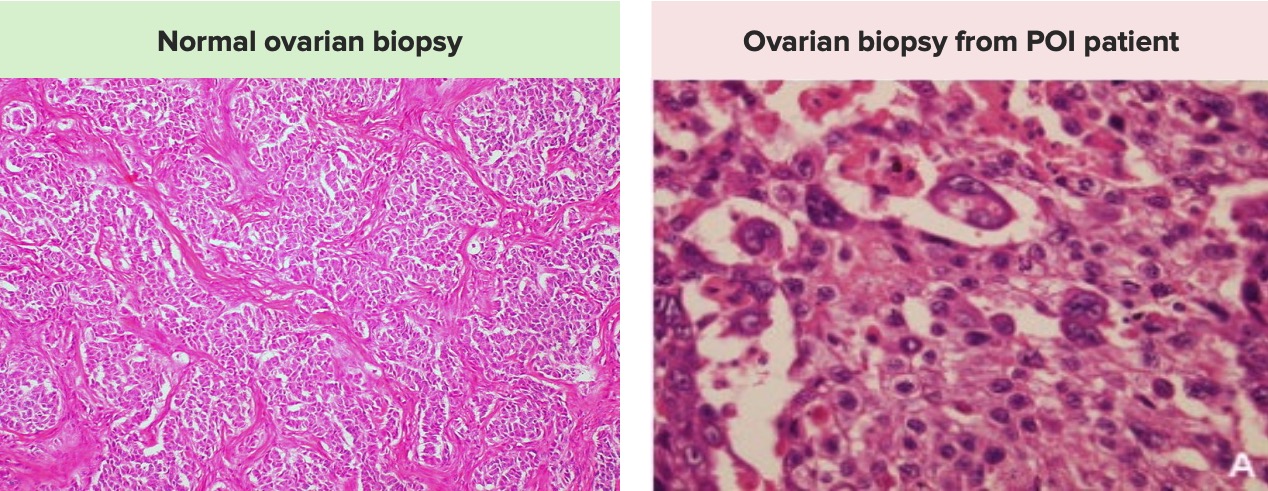
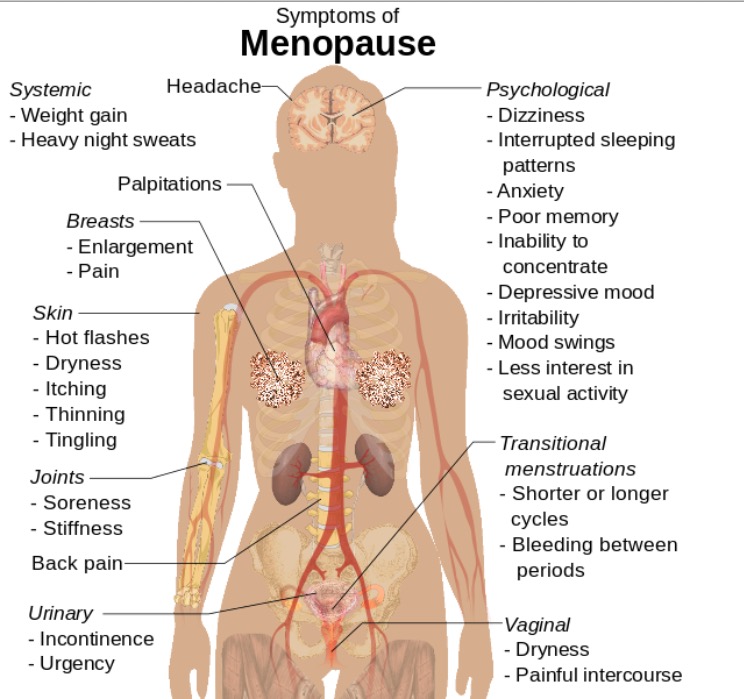
00:00 Hello. This will be a lecture entitled Primary Ovarian Insufficiency. This is a cause of secondary amenorrhea. Let's jump right in. Primary ovarian insufficiency is sometimes referred to as hypergonadotropic hypogonadism. This is not menopause. This occurs when a woman has oligo or amenorrhea for 4 months or she has laboratory findings consistent with the disease. That typically means that you'll have 2 FSHs greater than 30 obtained at least 1 month apart. Now let's look oocytes which means her reserve is decreased. Let's talk about the epidemiology of primary ovarian insufficiency. It affects about 1% of women in the US; however, this is hard to really identify as some patients may be on oral contraceptive pills which may mask symptoms. 00:57 Incidence is increasing due to the increasing rates of premenopausal cancer survivors. 01:03 The specific risk factor is tested on the USMLE POI for short has varying and unpredictable levels of ovarian function and this occurs in about half of women who actually make the diagnosis. 5 to 10% of women conceive and actually deliver after the diagnosis. 90% of patients though have no clear etiology making this a very difficult and frustrating diagnosis for patients. Let's now talk about making the diagnosis in patients. One study found that patients had to see more than 3 different clinicians before the diagnosis was actually made. This can be very frustrating for a patient so you should think about this syndrome when a woman has oligomenorrhea or amenorrhea. When you have a patient that you suspect has ovarian insufficiency, remember it's important to always take a thorough history and do a physical exam. First you want to question her about her normal puberty and establish that she at one point had regular menses. If she didn't, this will be called primary amenorrhea. This occurs in 10% of cases. If you'd like to know more about primary amenorrhea, there is a separate lecture about that. If a patient has an abrupt stop of menses, this is consistent with ovarian insufficiency. 02:29 You can have a common prodrome of oligomenorrhea, polymenorrhea, or AUB. If you'd like to learn more about AUB, please refer to that lecture. You also find on physical exam these patients have estrogen deficiency. They may complain of hot flushes which are actually called hot flashes which are vasomotor symptoms. They may also complain of night sweats. They may say something such as "I sweat through my pajamas every night." They may appear sleepy or somnolent usually because they have some type of sleep disturbance due to their vasomotor symptoms. These patients can also have dyspareunia which is related to vaginal dryness in the setting of low estrogen. 03:17 Sometimes you may find a positive family history during your history taking. 10 to 15% of women have an affected first degree relative. There are some other associated conditions that you may find on history. They may have other autoimmune disorders such as hypothyroidism or adrenal insufficiency or hypoparathyroidism. They may complain of dry eye syndrome, they may carry a diagnosis of myasthenia gravis, rheumatoid arthritis, or lupus. Let's now review a case. "I had a 27-year-old woman come to my office and she had Tanner stage III breast and pubic hair development. 04:01 Wait a second. Tanner III and she's grown? Hmm. She was started on oral contraceptive pills as a teenager because she only had a few episodes of spotting. This time she was coming to the office because she wanted to become pregnant and was experiencing infertility. Her FSH level or follicle stimulating hormone was found to be markedly elevated and her estrogen levels were in the menopausal range or very low. What's your differential diagnosis? I'll let you think about that. Are you ready to go on? How would you counsel and how would you treat this patient? Well this patient likely has primary ovarian insufficiency. She can potentially have other causes such as gonadal dysgenesis with mosaicism as we talked about in another lecture entitled Turner Syndrome. What would you do for this patient? You would attain a karyotype with FMR1 premutation evaluation as well. This patient would require hormone replacement therapy because recall her gonads or her ovaries are not producing estrogen which is bone protective. Once you've made the diagnosis of ovarian insufficiency, this patient will require a baseline DEXA scan. Let's now discuss the physical exam that we might see in a patient who presents with primary ovarian insufficiency. Recall that these patients have other autoimmune processes which can help you or assist you in the diagnosis. You sometimes may see hypopigmentation or vitiligo. Sometimes you can also see hyperpigmentation as would occur with potentially adrenal insufficiency. The thyroid may be enlarged so it's important to palpate the thyroid and ask the patient if she has noticed any differences. Sometimes bringing in old photos of the neck prior in life can actually help you determine if the thyroid has enlarged. There are some certain stigmata associated with Turner syndrome such as short stature, webbed neck, and a high-arched palate that may suggest that the cause may be Turner syndrome. Let's now talk about the laboratory evaluation. In these patients, you should obtain a serum prolactin just to rule out hyperprolactinemia. You should also obtain a cycle day #3 FSH or follicle stimulating hormone with an estradiol. If they are not having a menses, you won't know when cycle day #3 is so you may have to do this just spontaneously and an AMH in conjunction with that will help to determine if the FSH and estradiol are truly accurate. 06:51 To evaluate autoimmune etiologies for POI or primary ovarian insufficiency. 06:57 In addition to TSH, recommended testing includes free T4, antithyroid peroxidase antibodies, anti 21 hydroxylase antibodies and anti adrenal cortex antibodies. 07:12 You can also get a TSH or thyroid stimulating hormone. This will help to tell you if she has hypothyroidism which is an autoimmune disease that can go along with ovarian insufficiency. 07:24 If you make the diagnosis, these patients also require anti-adrenal antibodies as these antibodies are very important and may suggest that in the future she may have adrenal crises which can be life threatening. Let's now talk about counseling. This may not be actually question on your USMLE but it's important to note that many women described feeling emotionally devastated after a diagnosis of primary ovarian insufficiency. Essentially, most of these patients think they will never be able to become a mother which is not quite true but it is definitely more complicated. 08:02 Therefore, as a provider, we have to schedule sufficient time to go over the medical and emotional impact of such a diagnosis. Okay, now let's talk about when it's time to refer these patients to a subspecialist. You may be a family medicine doctor or a pediatrician or OB/GYN. It's important to do some evaluation before these patients are referred. A karyotype is helpful in determining whether this patient may be a Turner Mosaic. A fragile X premutation screen is also helpful as this can be a cause of primary ovarian insufficiency. Adrenal antibodies are also helpful to the clinician that will see this patient as that can tell of an impending adrenal crisis. A pelvic ultrasound is also helpful as we can see if there are any follicles on the ovaries. A baseline DEXA will also be helpful to tell us if there is abnormal bone mineral density as you can sometimes see with osteopenia. This information is high yield and you will likely be tested about one of these evaluations. 09:07 In terms of the etiology, most cases will have 46,XX karyotype. Unfortunately, 90% of these cases will not have a clear etiology identified and this is problematic and distressing for many patients. 09:23 About 4% will have steroidogenic cell autoimmunity and this is a reason they don't make estrogen. 09:31 About 14% of patients with familial POI will have a premutation to the FMR1 gene as opposed to 2% of women who have isolated POI. Let's now briefly review some of the syndromes that are associated with 46,XX POI. The most important here that I want to bring your attention to is fragile X associated disorders, the gene being FMR1. These patients usually have a family history of intellectual disability usually in males and some of their older relatives may be diagnosed with Parkinsonian-type syndromes that cause tremor and ataxia disorder. It's important to note that FMR1 is frequently tested on exams. Here you can see there are other diagnosis that can lead to 46,XX POI. Please download this at your convenience to review them. If you'd like more information, you can check out the genes on OMIM, which is a free database that will go over the presentation and genetics of each disease.
About the Lecture
The lecture Primary Ovarian Insufficiency (POI) by Lynae Brayboy, MD is from the course Abnormal Menstruation. It contains the following chapters:
- Primary Ovarian Insufficiency
- Case: Typical Presentation
- POI: Evaluation
Included Quiz Questions
Which of the following would NOT be expected in patients with primary ovarian deficiency?
- Dysmenorrhea
- Hot flashes
- Vaginal dryness
- Dyspareunia
- Sleep disturbances
Which of the following is associated with primary ovarian insufficiency?
- Myasthenia gravis
- Serous cystadenocarcinoma
- Brunner tumor
- Polycystic disease of ovary
- Teratoma
Which of the following is FALSE regarding primary ovarian insufficiency?
- Almost 90% of the etiology can be detected.
- Many women with primary ovarian insufficiency have steroidogenic cell autoimmunity.
- Women with familial primary ovarian insufficiency have permutation in FMR1 gene.
- Most cases with primary ovarian insufficiency have 46 XX karyotype with secondary amenorrhoea.
- Rheumatoid arthritis is associated with primary ovarian insufficiency.
Which of the following is helpful to perform before referral of a patient with primary ovarian insufficiency?
- All the options are helpful to perform before referral.
- Karyotype
- FMR premutation screen
- Adrenal antibodies
- Pelvic ultrasound
What is the purpose of doing a pelvic ultrasound prior to referral of the patient with primary ovarian insufficiency?
- To check for follicles
- To rule out associated benign disease
- To rule out associated malignant ovarian disease
- To provide an accurate diagnosis of primary ovarian insufficiency
- To check for the prognosis of the disease
Which of the following genes are associated with autoimmune polyendocrine syndrome type 1?
- AIRE
- FMR
- CYP17A1
- GALT
- FOXL2
Which of the following genes are present with hepatomegaly, cataracts and intellectual disability in a 2-year-old child who will have primary ovarian insufficiency?
- GALT
- FOXL2
- POLG
- PMM2
- CYP17A1
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |