Playlist
Show Playlist
Hide Playlist
Post-Streptococcal Glomerulonephritis
-
Slides Glomerulonephritis.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
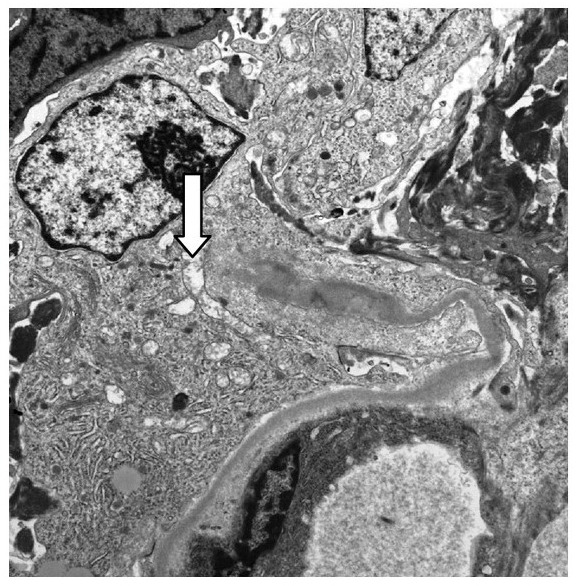
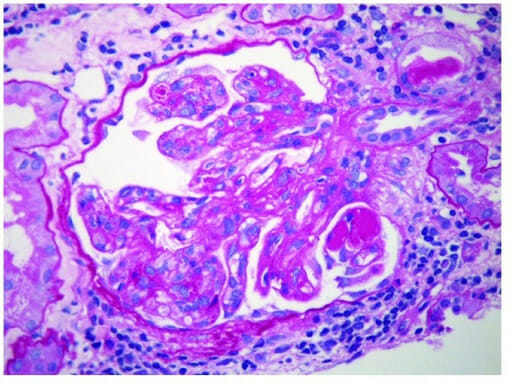
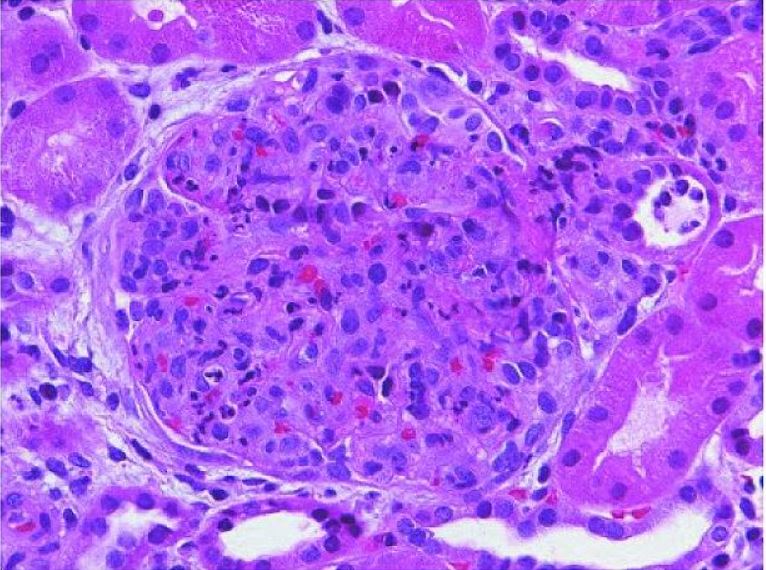
00:01 Continuing our discussion of glomerulonephritis. 00:04 We are still within the realm of nephritic disorders and with nephritic disorders, at this point, you should be pretty good with what the overall signs of the patients are including your hypertension and hematuria. 00:19 With hematurias, RBC casts, dysmorphic RBCs, oliguria and as far as protein loss is concerned, less than 3.5 grams of protein per day and this is the most common type of post infectious glomerulonephritis. 00:34 Is that clear? In a little bit, I’ll give you some non-infectious glomerulonephritis. 00:39 Now, with post infectious, this will be most commonly following weeks after exposure to an organism, bacteria known as group A streptococci and here, of course, we’re referring to streptococci pyogenes. 00:53 Now, before I give you pharyngitis which many of you, most of you are familiar with, I have to point out to you skin, skin, skin. 01:03 And by skin, maybe perhaps you have a skin infection by the same organism, so, that’s not going to differ. 01:09 Now, what you will have to memorize is the fact that it’s subepithelial immune-complex deposition. 01:17 To make your life a little bit easier, P as in post, P as in subepi. 01:22 Now, on light microscopy, you’re going to find diffused proliferation of that glomerulus. 01:29 So in your mind, you should be think as to what a light microscopy normally looks like of a glomerulus, and then, here with PSGN, we have diffused proliferation with neutrophilic infiltration. 01:41 On immunofluorescence microscopy of tissue from a kidney biopsy, there is a characteristic diffuse granular pattern of IgG and C3 complement seen in the capillary walls, referred to as a "starry sky" pattern. 01:53 On electron microscopy, there are dome-shaped subepithelial deposition or "humps" Which are immune complexes that correspond to the IgG and C3 deposits". 02:03 Post-streptococcal glomerulonephritis is induced by specific nephritogenic strains of Group A Streptococcal infection. 02:10 The clinical presentation can vary from asymptomatic microscopic hematuria to a full-blown nephritic syndrome with gross hematuria, edema, hypertension, and sometimes acute kidney injury. 02:22 The hypertension can be severe but is transient and treatable with medications. 02:26 Other treatment is supportive including diuretics for the edema, and antibiotics are used only if there is currently a strep infection still present, the most patients have already cleared their Group A strep infection be this time. 02:37 Short-term dialysis may be needed for patients with acute kidney injury, but the vast majority of patients with post-steptococcal glomerulonephritis recover completely in a few weeks. 02:46 Now, with the Streptozyme test, important ones that you wanna keep in mind here. 02:50 Typically rise, what you’re seeing here in green. 02:55 ASO, anti-streptolysin O, anti-hyaluronidase, anti-nicotinamide or adenine-dinucleotidase, all part of typically rising in post-streptococcal, postpharyngeal is what we’re looking for, anti-DNAse B antibody. 03:16 Once again, post pharyngeal cause, are we clear? Of what? Resulting in PSGN. 03:22 Next, post-skin causes and by skin, it’s still the same organism. 03:29 It should be noted that all of these tests can be positive in response to a pharyngeal source of poststreptococcal GN, but from a skin source such as impetigo, only the anti-DNAase B and AHase titers are typically increased. 03:41 These are numbers 2 and 5 on the slide. 03:44 Labs, what are we looking for Well, we have nephritic, nephritic, nephritic. 03:49 We talked about hypertension and its importance for management. 03:53 Next, you do have your hematuria and under hematuria, RBC casts, yes. 03:58 Could you find RBC’s? Sure. 04:00 Most likely, what kind of RBC’s? Dysmorphic. 04:03 Because you’ve activated your complement system, you can expect there to be deposition every complement and thus in your serum, you have hypocomplementemia, specifically, C3. 04:14 Next, as far as your streptozyme tests are concerned, well, we just went through both of the strains, pharyngeal and skin. 04:22 Clinical features, prognosis, children, recovery, 95% and greater. 04:27 Adults, not so much. 04:29 Some may progress to RPGN, keep that in mind.
About the Lecture
The lecture Post-Streptococcal Glomerulonephritis by Carlo Raj, MD is from the course Glomerulonephritis.
Included Quiz Questions
Which of the following depicts the location of the deposition of immune complexes in post-streptococcal glomerulonephritis?
- Subepithelial
- Subendothelial
- Mesangial
- Vascular
- Bowman's space
Which of the following clinical manifestations is not likely seen in a patient with post-streptococcal glomerulonephritis?
- Proteinuria of > 3.5 g/day
- Hematuria
- RBC casts in the urine
- Hypertension
- Proteinuria of < 3.5 g/day
Which of the following is not manifested by the nephritogenic strain of group A streptococcal infection?
- Pancarditis
- RBC casts
- Dysmorphic RBC
- Periorbital edema
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Dr Carlo Raj is excellent teacher that manages to keep me both attentive and interested in the topic. He seems to have a good understanding of key topics and what is important to medical students.
It was great because I achieved to understand in detail a very complex topics. Thanks