Playlist
Show Playlist
Hide Playlist
Polyarteritis Nodosa
-
Slides Vasculitis.pdf
-
Reference List Rheumatology.pdf
-
Download Lecture Overview
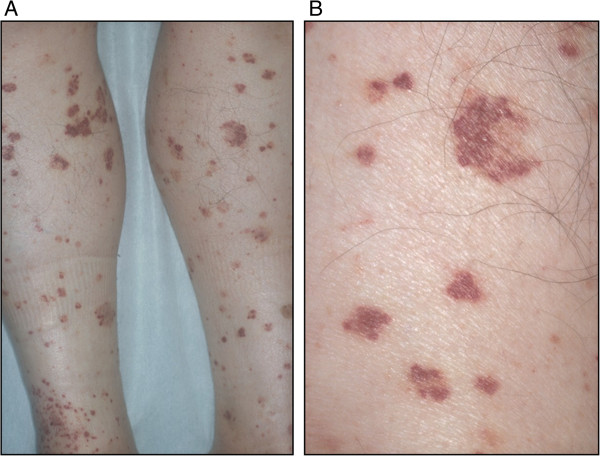
00:00 So, let's start at the bottom for this case with polyarteritis nodosa. So polyarteritis nodosa, again shown here on the right with multiple aneurysms and irregular constrictions, is a systemic necrotizing vasculitis of medium-sized arteries in multiple organ systems. I'll also mention here that many of these vasculitides are not exclusively involving medium vessels or small vessels or large vessels. For the most part when we call something a small, medium, or large vessel vasculitis we're just highlighting that most of the pathology is small or medium or large but a large vessel vasculitides could also have some medium-sized arteries involved and a small vessel vasculitis could have some medium vessels involved. So, just keep that in mind as we go through this. Next up while polyarteritis nodosa like all of the vasculitides is idiopathic, we do know that it is strongly associated with hepatitis B and hepatitis C so we have to keep that in mind. We were told that she has a history of injection drug use with cocaine so perhaps she could've transmitted HPV or HCV. Polyarteritis nodosa is characterized by segmental, transmural inflammation which leads to luminal narrowing, thrombosis potentially, of course downstream ischemia as we've talked about before, and aneurismal dilatation and that's of course what we're seeing in our image. It's tissue necrosis that can lead to things like renal infarcts and other disease pathology. 01:30 What we're going to do now is take a brief detour from this slide just to talk about the different ways that this segmental, transmural inflammation can manifest in various organs. We'll be back to this one. So here's our list of the specific manifestations that we can see with polyarteritis nodosa. First up on this skin exam you'll find palpable purpura, tender subcutaneous nodules, and potentially livedo reticularis. This, if you perform a biopsy, will be associated with some evidence of leukocytoclastic vasculitis which is a finding you'll see in a light of a different vasculitides. The kidneys essentially can manifest with either renal artery aneurysms or potentially renal infarcts if there's significant occlusion of the renal arteries, which of course you might find on renal arteriography. In fact, new onset hypertension with an accompanying acute kidney injury may be a significant clue to either renal artery aneurysms or renal infarction in such patients. On the neurologic exam, you'll certainly find some peripheral nerve involvement which could also be an indication of vasculitis involving the nerve's vascular system. That condition is called mononeuritis and when you have multiple nerves involved you'd call it mononeuritis multiplex and I'll remind you our patient seems to have an acute foot drop which could be an indication of a mononeuritis. Next up, the gastrointestinal system. Like any artery in the body, if the mesenteric arteries are a little bit occluded you can get intestinal ischemia. 02:59 So, mesenteric arteritis with intestinal angina would also be a feature that we'd be worried about with polyarteritis nodosa amongst a number of other vasculitides and it sounds again like that may be something that we're seeing in our patient. Okay, let's go back to that slide we were looking at before. Now that we're back to the slide, we can briefly discuss the diagnosis of polyarteritis nodosa. There's a lot of different manifestations that PAN can have that are similar to the other vasculitides. So ultimately you're going to need a biopsy to make this diagnosis. In contrast to the 3 other diagnoses that were on our list, the 3 other types of small vessel vasculitis, this condition is going to be ANCA negative when you perform serologic testing. 03:41 Of course, a mesenteric arteriography might be helpful like the one shown here, that would be a pretty strong clue for this diagnosis. Lastly, briefly talking about the treatment, you're going to treat polyarteritis nodosa with steroids. You'll possibly add on cyclophosphamide in certain cases best left to the discretion of a rheumatologist. And of course, if it turns out the patient does have hepatitis B, you should probably go ahead and treat that too. One thing we're going to see over time is that most of our vasculitides are going to be treated with steroids plus or minus cyclophosphamide though there are some important cases where we would not use those medications. Alright, so with all that in mind we've got an awful lot going for polyarteritis nodosa. We'll need to get some more labs and imaging data before we draw any conclusions, however. Of course, thinking back on the case though that history of asthma is kind of odd but then again, you know, asthma is incredibly common and maybe there's nothing to do with our patient's presentation. So we'll leave a question mark for PAN for now.
About the Lecture
The lecture Polyarteritis Nodosa by Stephen Holt, MD, MS is from the course Vasculitides.
Included Quiz Questions
All of the following clinical features are associated with polyarteritis nodosa EXCEPT...?
- ...unilateral orbital pain and redness.
- ...livedo reticularis.
- ...wrist drop.
- ...palpable purpura.
- ...hematuria due to renal infarction.
A 39-year-old woman presents to the emergency department with hematuria. Her medical history is significant for chronic hepatitis B and polyarteritis nodosa. Her vital signs include blood pressure of 146/94 mm Hg, a pulse of 74/min, and a respiratory rate of 14/min. Laboratory findings are significant for elevated creatinine and hematuria. Renal arteriography is significant for multiple aneurysms on the left side and complete occlusion of the right renal artery. Which of the following is NOT considered as part of the treatment plan?
- Furosemide
- Steroids
- Cyclophosphamide
- Hepatitis B treatment
- Antihypertensive medications
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |