Playlist
Show Playlist
Hide Playlist
POI: Mechanisms, FMR 1 and Management
-
Slides Primary Ovarian Insufficiency.pdf
-
Download Lecture Overview
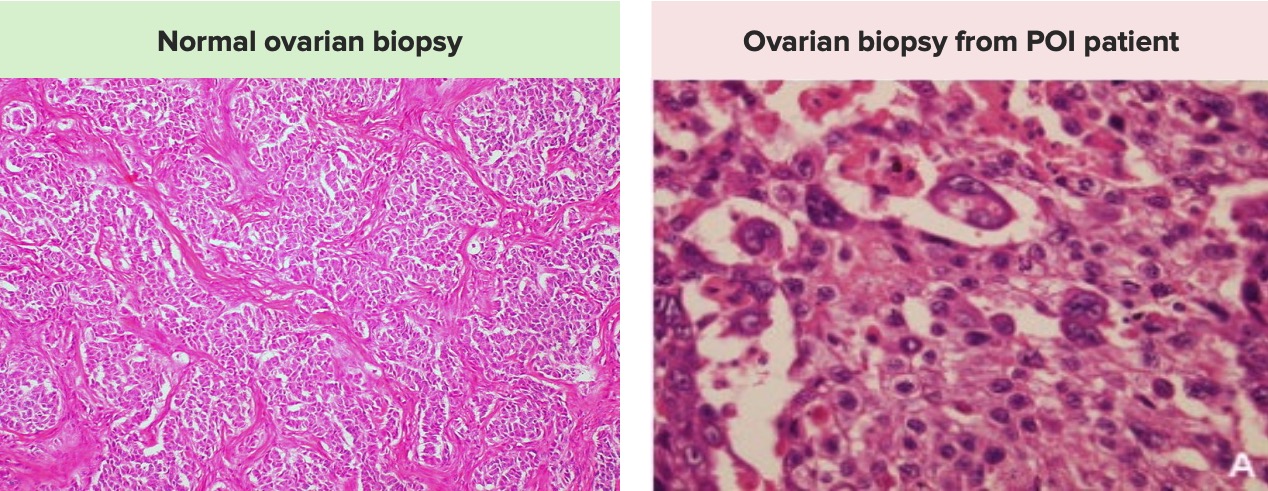
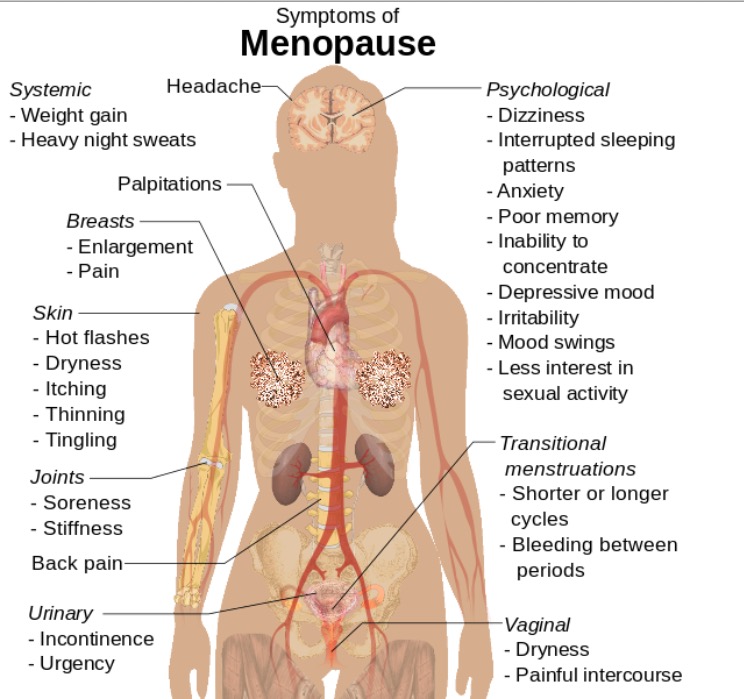
00:01 Let’s now review POI Ovarian dysfunction. 00:05 Sometimes you can have a signal defect. 00:07 That is to say, that the FSH and LH receptors do not function properly. 00:13 Here, you’ll see that the theca cell has an LH receptor, while the granulosa cell has an FSH receptor. 00:21 Normally, LH and FSH surges will cause LH and FSH to bind to this receptor. 00:28 These receptors in turn will cause steroidogenesis to occur with the precursor being cholesterol. 00:35 Cholesterol is converted through a long pathway to androstenedione and testosterone in the theca cells. 00:42 These two hormones then diffuse into the granulosa cell and are aromatized by aromatase making estrone and estradiol. 00:52 For more information about this pathway, please check out the lecture entitled, Congenital Adrenal Hyperplasia. 00:58 You can also have enzymatic deficiencies. 01:02 You have isolated 17.200 lyase deficiency. 01:06 This is discussed more in the CAH or congenital adrenal hyperplasia lecture. 01:11 You can always have aromatase deficiency as well. 01:15 Aromatase deficiency means that the androgens cannot be converted to estrogens. 01:20 You can find more about this pathway again in the CAH lectures. 01:25 You may also have autoimmunity causing ovarian insufficiency. 01:29 And typically, this is a lymphocytic oophoritis which is autoimmune, of course. 01:35 And occasionally, you can have inappropriate follicular luteinization. 01:40 And what that means is that the LH surge normally causes luteinization after ovulation. 01:46 But this can happen in follicles before the oocyte is released, and therefore, the ovary has some dysfunction. 01:53 60% of all antral follicles are found to be luteinized with this condition. 01:58 Let’s now talk about follicular depletion in ovarian insufficiency. 02:04 Essentially, what this means, is that the patient may have an insufficient initial follicle number. 02:09 As you’ll recall from the puberty lectures, we have millions of follicles and oocytes midgestation. 02:17 These follicles and oocytes then undergo atresia. 02:21 However, patients with POI may start out with much less. 02:26 This is the case in some familial syndromes where you have follicular depletion such as an NBPES. 02:33 Please find more information about this syndrome in OMIM. 02:37 With Turner Syndrome, we also think the mechanism is follicular depletion. 02:42 These patients start out with less ovarian reserve and lose their ovarian reserve through atresia. 02:48 However, some of us may also experience spontaneous accelerated follicle loss leading to ovarian insufficiency. 02:56 Let’s now talk about Fragile X or FMR1 permutation as a cause of POI. 03:05 In Fragile X, we have three different clinical presentations. 03:10 You can have Fragile X syndrome, primary ovarian insufficiency, or Fragile X-associated tremor ataxia syndrome or FXTAS for short. 03:20 Let’s discuss what you have in this setting of a premutation; normal, abnormal, and a full mutation. 03:30 Normal is less than 45 repeats and determinant means 45-54 repeats, and there are increased risk of expansion. 03:39 A premutation is 55-200 repeats and a full mutation is greater than 200 repeats, which will cause fragile X syndrome. 03:49 Now let’s talk about how they actually develop molecularly. 03:53 In the normal patient, you should have a normal amount of FMR1 mRNA, but in the premutation you may have less and in the full mutation you may have none. 04:04 That affects protein function or protein development that affects phenotype. 04:10 And in the normal patient, you shouldn’t see any phenotype but the premutation you may see POI. 04:17 With the full mutation, you will see the syndrome. 04:19 Let’s now discuss the different physical attributes in men who have fragile X. 04:25 They tend to have tall structure, macrocephaly, and an elongated face, large ears, large testes sometimes called macro-orchidism, MVP or mitral valve prolapse, joint hypermobility and generalized hypotonia. 04:43 They can also have some deficits intellectually. 04:46 They may have a moderately low IQ. 04:50 They may have anxiety, hyperactivity, ADD or Attention deficit disorder. 04:56 These patients may maintain avoidance of eye contact, and they may have speech perseveration, perseveration, perseveration. 05:05 That means that they repeat something over, over, and over again. 05:09 They may have stereotypical movements and autism. 05:13 Let’s now talk about Fragile X associated tremor ataxia syndrome. 05:19 This is usually diagnosed later in life, and not something that a gynecologist would actually see. 05:25 However, it’s hopeful to know that there are certain MRI findings that maybe present. 05:29 If you suspect POI in a patient, you should alert her that she should inform her other family members who may suffer from this. 05:37 We see on histology that there are certain inclusion cyst that are found in the brain when this syndrome is present. 05:44 Let’s now talk about how the number of repeats correlate with the last menstrual cycle. 05:52 Remember these patients are going into a early menopause state. 05:56 The higher the number of repeats, the more likely that she will go into menopause earlier. 06:01 Here you can see that a hundred repeats to two hundred repeats means that you’ll go into menopause much earlier than average. 06:09 Increased repeats not only determine the severity of disease for the individual, your patient, but also any children she may have in the future. 06:20 Remember, that even though these patients have ovarian insufficiency, they may have spontaneous conception. 06:27 And there’s a definite increase of the risk of expansion. 06:30 Let’s now talk about the endocrine profile in an ovarian insufficient patient. 06:37 In a normal patient we should have normal FSH levels, their fertility should be normal and they should have regular monthly menses 21-35 days on average. 06:48 With occult POI, which means that it hasn’t been discover yet, they can have normal FSH but reduced fertility and regular menses. 06:57 And these patients that we suspect of having occult disease it’s helpful to send up FMR1 premutation. 07:04 Then there’s biochemical POI, that means they’re starting to have some biochemical symptoms. 07:10 Including an elevated FSH with reduced fertility but they still may have regular menses. 07:16 And then there’s overt POI. 07:18 They have elevated FSH, they have reduced fertility and they may have irregular or absent menses. 07:25 These patients are on their way to having frank ovarian sufficiency and menopausal symptoms. 07:31 Let’s now talk about autoimmunity in these patients. 07:35 This is characterized by oophoritis or lymphocytic infiltrates growing into the follicles. 07:41 You can see this histological picture here where we do have evidence of this. 07:45 This is associated with adrenal insufficiency or Addisonian crisis or Addison's disease. 07:52 These can also be associate with autoimmune hypothyroidism. 07:55 And these should never be forgotten in the context of ovarian insufficiency. 07:59 We can now review the management of patients with ovarian insufficiency. 08:05 Hormone replacement is necessary. 08:08 However, oral contraceptive pills are not effective birth control. 08:13 And they’re also, not good HRT. 08:16 Typically, women with POI or ovarian insufficiency will require twice as much estrogen as a postmenopausal woman to alleviate symptoms. 08:27 Remember, they should be seeing estrogen that a young woman should be seen not which you would give to a postmenopausal woman who is actually already decreasing estrogen throughout her lifetime. 08:39 A 100 mcg estradiol patch is the recommended dosing. 08:44 However, there are other oral preparations that can be used as well. 08:48 Let’s now talk about contraception in these women. 08:52 Remember, then oral contraceptive pill is not good contraception or good hormone replacement therapy. 08:59 Now, why would an oral contraceptive pill work in this type of patient? Do you want to think about it? I’ll give you a second. 09:08 Well, their FSH is so high that it can’t be suppressed by the oral contraceptive pill, which is how it works. 09:16 Their LH may also be high and therefore a progesterone only pill can also not suppress their LH. 09:22 IUDs, intrauterine devices, and barrier methods are best choices for women who have ovarian insufficiency. 09:29 Again, we have not studied oral contraceptive pills in POI patients. 09:34 Let’s talk about ways these patients can conceive. 09:40 Well, they can spontaneously ovulate and have a child on their own. 09:44 However, it’s hard to predict when ovulation will occur because they may go in and out ovarian insufficiency and ovarian functionality. 09:52 These patients may opt for egg donation. 09:56 If you’d like information about egg donation, please see the lecture about assisted reproductive technologies. 10:02 These patients make up about 10% of all IVF cycles in the U.S. 10:07 They can also adopt embryos, however, this is a little bit more complicated as they have to adopt an embryo from certain organizations. 10:17 But, it’s not impossible. 10:19 And then there’s traditional adoption which is always encouraged in these patients. 10:24 These patients are at risk for osteoporosis and they should have a calcium intake of that of a postmenopausal woman between 1200 and 1500 mg of calcium daily. 10:37 Their vitamin D should be between 800 and a thousand IUs daily. 10:43 We encourage these women to engage in weight bearing exercises as well. 10:48 Also don’t forget to obtain a DEXA at baseline and reevaluate if they’re osteopenic. 10:55 The presence of adrenal antibodies has a 50% risk of developing Addisonian crisis or adrenal insufficiency. 11:03 Remember to check these and this may be tested on your USMLE. 11:07 Patients with ovarian sufficiency can also have autoimmune hypothyroidism. 11:13 20% of women who have POI will develop autoimmune hypothyroidism, such as in Hashimoto thyroiditis. 11:22 Thank you for listening and good luck on your exam.
About the Lecture
The lecture POI: Mechanisms, FMR 1 and Management by Lynae Brayboy, MD is from the course Abnormal Menstruation.
Included Quiz Questions
Which of the following is a characteristic feature of fragile X syndrome in males?
- Macroorchidism
- Microorchidism
- Macro-ovaries
- Micro-ovaries
- Atrophic ovaries
Which of the following is FALSE regarding fragile X syndrome?
- An increase in the number of repeats will decrease the severity of the disease.
- FMR1 gene is also associated with fragile X ataxia.
- Fragile X syndrome can present with psychiatric disturbances.
- Fragile X syndrome has macrocephaly.
Which of the following is NOT a feature of primary ovarian insufficiency?
- Occasionally, the individual can present with normal levels of serum FSH, regular menses, and normal fertility.
- In the occult form, there are normal premenopausal FSH levels, reduced fertility, and regular menses.
- In the biochemical form, the FSH level is elevated, with reduced fertility and regular menses.,
- In the overt form, the FSH level is elevated, the fertility is reduced, and there are irregular or absent menses.
- It can be associated with adrenal insufficiency and autoimmune hypothyroidism.
Which of the following is NOT a hormone typically evaluated for primary ovarian insufficiency?
- Cortisol
- FSH
- Estriol
- TSH
- Prolactin
Which of the following is NOT a mechanism of primary ovarian insufficiency?
- Asherman syndrome
- Enzyme deficiency
- Autoimmunity
- Inappropriate follicular luteinization
- Signal defect
Which of the following describes the histopathological picture of primary ovarian insufficiency due to autoimmunity?
- Oophoritis with lymphocytic infiltrates in growing follicles
- Large clear cells with centrally placed nuclei arranged in sheets in ovarian stroma
- Multiple cystic spaces in the ovary
- Cystic ovary with papillary excrescences
- Normal ovarian stroma
Which of the following is TRUE regarding primary ovarian insufficiency?
- IUD and barrier methods are useful for contraception in patients with primary ovarian insufficiency.
- Oral contraceptive pills are useful in patients with primary ovarian insufficiency.
- Progesterone only pills are useful in primary ovarian insufficiency as it helps decrease the LH levels.
- Hormone replacement therapy is NOT useful in treatment of primary ovarian insufficiency.
- Embryo transfer is NOT a useful alternative method to conceive in primary ovarian insufficiency.
A 40-year-old female with a BMI of 23 kg/m^2 presents with a fracture of the neck of the femur due to slipping in the bathroom. She was referred to the OB/GYN specialist for primary ovarian insufficiency. In addition to estrogen therapy, which of the following prophylactic treatments would have decreased the probability of this fracture?
- Vitamin D and calcium supplements
- Oral contraceptive pills
- Testosterone therapy
- Periodic X-ray scans of the whole body
- Weight loss
Customer reviews
2,0 of 5 stars
| 5 Stars |
|
0 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
2 |
| 1 Star |
|
0 |
I fully agree with the previous comment as the content is not well structured and it is hard to focus the attention as the content of the lectures is jumping all the time
no order on it, it would be better if keeps an idea flow as, epidemiology, etiology, fisiopatology, clinical presentation, diagnosis, treatment. i felt like jumping from one idea to another