Playlist
Show Playlist
Hide Playlist
PO₂ Calculations – Effect of Barometric Pressure on the Pulmonary System
-
Slides 06 PulmonaryBarometricPressure RespiratorySystem.pdf
-
Download Lecture Overview
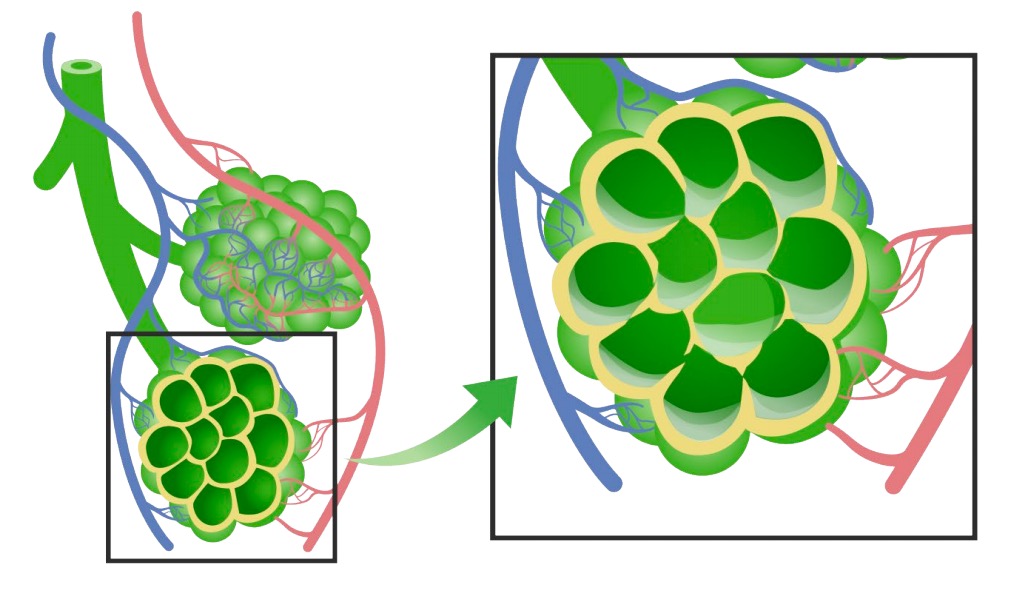
00:00 Now let’s go through a couple of examples of partial pressures of inspired O2. 00:06 If you think of your sea level calculation, if we are counting for humidity in the air, that value ends up being around 150 millimeters of mercury for PIO2. 00:19 If you look at Colorado Springs, with the barometric pressure of somewhere just over 600 millimeters of mercury, the pressure is only 118 millimeters of mercury. 00:31 If we look at the summit of Mount Everest in which barometric pressure is only 250 millimeters of mercury, barometric pressure in inspired air is only 43 millimeters of mercury. 00:45 That is less or about the same amount as normal sea level venous oxygen partial pressures are. 00:55 This is a very, very challenging environment. 00:58 And in fact, without supplemental oxygen, this is very difficult, particular barometric pressure to be able to overcome. 01:06 So now what we have the PIO2s which is the partial pressure of inspired O2, that doesn’t even account yet for what is in your alveolar or in your air sacs. 01:18 So at the summit of Mount Everest, the PIO2 is only 42 millimeters of mercury. 01:24 But that’s just the first part of this equation. 01:27 So you can understand how the alveolar partial pressure might be a lot more decreased than simply the inspired O2. 01:41 Now, what are the effects of high altitude? And we’re going to usually call high altitude, hypobaric hypoxia. 01:49 Hypo- meaning low pressure and low oxygen. 01:55 Alveolar ventilation and pulmonary blood flow are going to be the first topics. 02:01 Ventilation increases during a hypobaric, hypoxic exposure. 02:07 In terms of pulmonary blood flow, there are increases in cardiovascular responses and these usually are due to the mechanical effects of the lung. 02:17 The last areas that changes in terms of blood pressure is there is there is a hypoxic pulmonary vasoconstriction. 02:25 And what this does is increases mean pulmonary artery pressure and I will emphasize that right now because this may have something to do with high altitude pulmonary edema that we’ll talk about later. 02:39 There are also changes that happen in diffusion and gas transport. 02:43 So in terms of diffusion, there is a less of a gradient for O2 because there is a lower PAO2. 02:52 There’s also more surface area involved and this allows for – And this occurs because of recruitment issues that were previously unventilated or underperfused So the first aspect of diffusion increased your ability to diffuse. 03:09 The second aspect might increase it. 03:12 So diffusion is hard to know how much is going to change in hypobaric hypoxia. 03:17 In terms of gas transport, there could be issues associated with the loading, the O2 on hemoglobin. 03:27 Cardiac output though increases and that helps to maintain O2 delivery. 03:33 And finally, there usually is an increase in hemoglobin concentration and this occurs through one of two mechanisms. 03:41 One is either the person dehydrates themselves by urinating out more fluid or, chronically across time, you might increase red blood cell production. 03:56 What are the effects on the control of breathing? There’s usually a decrease in arterial O2. 04:03 And this will of course stimulate peripheral chemoreceptors to increase ventilation. 04:08 This ventilation though does have a downside. 04:11 And that is as ventilation increases, there is a decrease in the partial pressure of carbon dioxide both in the arterial as well as the alveolar spaces. 04:23 Now, this arterial hypocapnea or low PCO2 can diffuse out some CO2 in the cerebrospinal fluid. 04:32 Why this is bad is that central chemoreceptors respond to this particular carbon dioxide. 04:41 And this creates an alkalosis in the cerebrospinal fluid. 04:46 And thus, can suppress the drive to breathe. 04:52 So what do you want to do if you’re exposed to hypobaric hypoxia? The first thing is you want to ventilate more. 04:59 So you want to hyperventilate, hyperventilate, hyperventilate. 05:02 The second thing you’d want to do is increase O2 transport and you can do that by pumping more blood through the system. 05:10 Finally, you want to hemoconcentrate the blood, meaning that you want to have more red blood cells per 100 mLs of blood. 05:18 You can either do it acutely by decreasing plasma volume or chronically by increasing the number of red blood cells. 05:25 And finally, with these acid-base changes that happen, the body must adapt to that and so it can get rid of bicarbonate easily. 05:35 Now, if we can’t adapt to an environment, what happens to you? Well, it usually is an illness can result. 05:45 Acute mountain sickness and high altitude cerebral edema are two. 05:49 High altitude pulmonary edema is another potential as well as there are other ones that we’re not going to go through dealing with high altitude illnesses such as chronic mountain sickness, there can some retinal hemorrhages that occur and a lot of times, this can also exacerbate some chronic conditions whether it be cardiovascular or pulmonary in nature.
About the Lecture
The lecture PO₂ Calculations – Effect of Barometric Pressure on the Pulmonary System by Thad Wilson, PhD is from the course Respiratory Physiology.
Included Quiz Questions
Which of the following is a predictable acute effect of hypobaric hypoxia?
- An increase in mean pulmonary artery pressure
- A decrease in the rate and depth of breathing
- An increase in the partial pressure gradient of oxygen
- A decrease in hemoglobin concentration
- A decrease in urinary output
Which of the following is NOT an effect of the hyperventilation response to hypobaric hypoxia?
- Stimulation of central chemoreceptors
- The decreased partial pressure of carbon dioxide in the arterial blood
- The decreased partial pressure of carbon dioxide in the alveolar gas
- Diffusion of carbon dioxide out of the cerebrospinal fluid
- The depressed activity of central chemoreceptors
Which of the following changes will NOT occur at high altitude?
- Respiratory acidosis
- Hyperventilation
- Increased cardiac output
- Increased red cell mass
- Decreased plasma volume
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
very good lecture! finally i understood respiratory physiology, i loved the slides