Playlist
Show Playlist
Hide Playlist
Placenta and Fetal Membranes
-
Slides 10-64 Placenta, Fetal Membranes and Abnormalities.pdf
-
Reference List Embryology.pdf
-
Download Lecture Overview
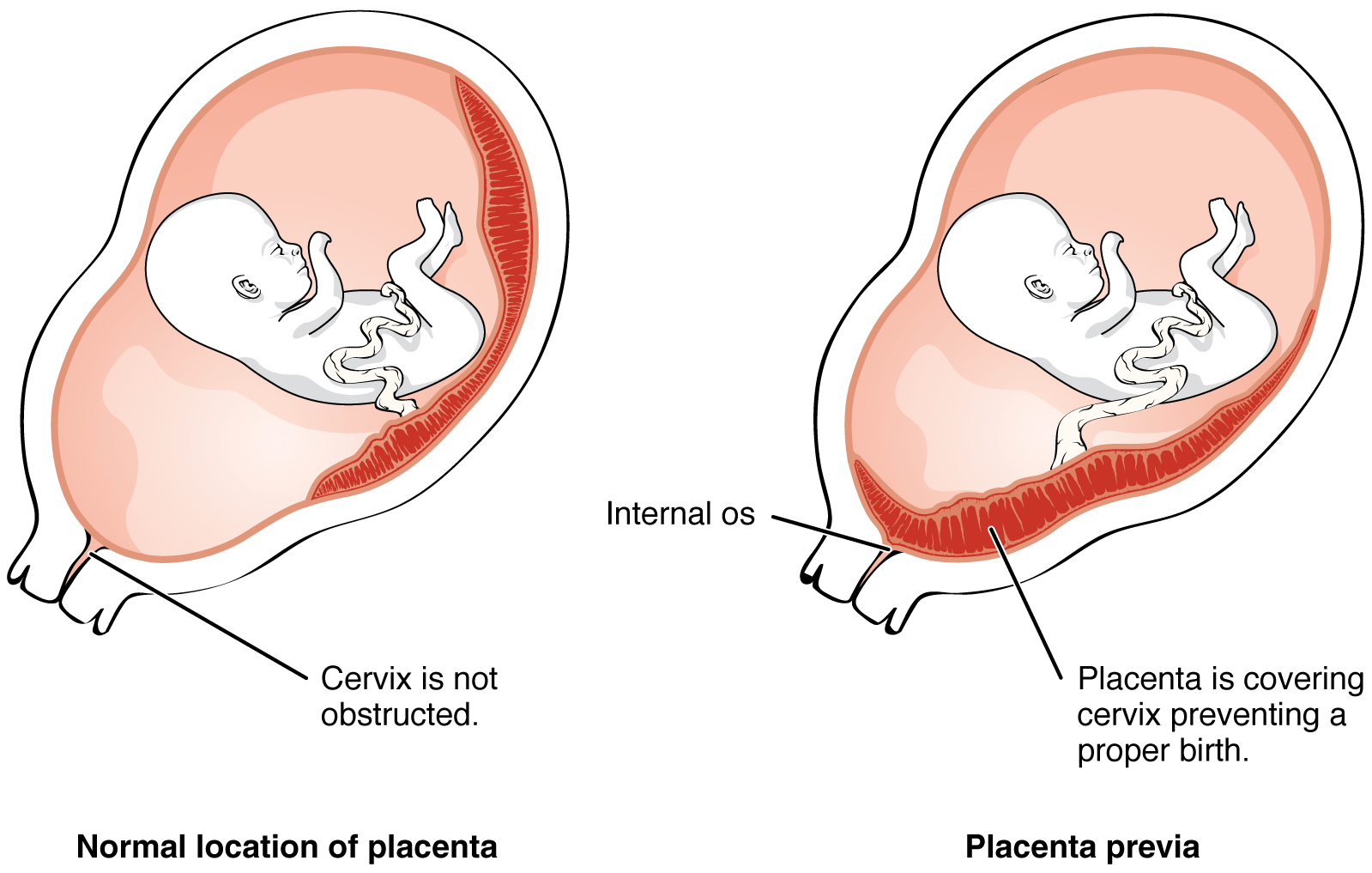
00:01 We will now proceed to follow the further development of the placenta and its relationship to the membranes that surround the developing fetus. 00:10 Once the placenta is in place, we have a situation where uterine arteries travel into placenta bringing oxygen in blood to the embryo. 00:19 This maternal oxygen and blood fills intervillous spaces and allows gas exchange to occur across the villi. 00:27 Maternal blood interacts with deoxygenated blood coming from the umbilical arteries of the fetus, and even if though blood does not directly mingle, gas exchange and nutrients exchange occur across the villi. 00:40 Thereafter, umbilical veins take oxygenated blood back to the embryo and maternal veins take deoxygenated maternal blood from the intervillous space back into maternal circulation to be replenished. 00:54 Typically, the blood of the fetus and the mother should never directly connect. 01:00 One problem that arises with this situation is that as maternal blood enters the intervillous space, it necessarily mixes with blood that's already there; meaning that the oxygenated blood from the mother is mixing with the deoxygenated blood already present in the intervillous space that has not yet left through maternal vein. 01:19 What this means is that the oxygen content of the blood in the intervillous space is lower than pure arterial blood. 01:26 To compensate for this, the fetus produces a fetal hemoglobin which binds to oxygen much more strongly than mature hemoglobin. 01:36 In physiology, we can say that the O2 P50 value of fetal hemoglobin is 19 millimeters of mercury, meaning it's about 50% saturated at a partial pressure of 19 millimeters compared with 26.8 millimeters of mercury for adult hemoglobin. 01:56 Long story short, it binds to oxygen much more strongly than mature hemoglobin and allows the fetal hemoglobin to actually take the oxygen away from the maternal circulation even though we've got mixture of maternal oxygenated and deoxygenated blood in the intervillous space. 02:15 Now, one problem that can also occur, is that if fetal blood does contact maternal blood due to a rupture of a villus or another problem, there can be immune reactions on the maternal side to fetal blood. 02:28 In particular, if the fetal blood produces the D antigen and is therefore Rh positive, then it can create an immune reaction in a mother who is Rh negative. 02:41 So she has not got that antigen on her own blood, she will produce antibodies against the D antigen and these IgG antibodies can cross the placenta and attack fetal red blood cells. 02:56 Anti-D immune globulin prevents the Alloimmunization in a D-Woman by interfering with the maternal immune response provoked by D antigen positive fetal red cells that have escaped into the maternal circulation. 03:09 Exactly how immunization is prevented is unknown, but it may include rapid macrophage mediated clearance of anti decoded red cells and or down regulation of antigen specific B cells before alloimmunization occurs. 03:23 All D-women who have a negative anti-D antibody screen and who are carrying a fetus that is or maybe D+ should be given anti-D immune globulin. 03:33 The specific circumstances are at 28 weeks of gestation after delivery of a D+ newborn or after an anti partum event associated with an increased risk of fetal maternal bleeding such as spontaneous or induced abortion, threatened abortion, ectopic pregnancy, blunt abdominal trauma, amniocentesis or antepartum vaginal bleeding. 03:55 D- women who screen positive for anti-d antibodies should not receive anti-d immune globulin. 04:01 Because it is not effective and will not prevent a rise in maternal tighter. 04:06 Attacking the fetal red blood cells causes a condition known as erythroblastosis fetalis, that's going to mean that we have an excess of creation of new red blood cells erythroblast in the fetus to compensate for the red blood cells that are being attacked by the maternal antibodies. 04:24 This can progress to a condition called fetal hydrops where the tissues of the fetus swell in response to the immune attack from the mothers antibodies and in less severe but still serious forms you can have breakdown of fetal blood cells producing excessive bilirubin leading to jaundice as development proceeds further. 04:43 This response becomes more and more severe for subsequent pregnancies because the maternal immune system is already primed to produce those antibodies against the D antigen and RH positive blood. 04:55 The placenta initially is going to form as a spherical object surrounding the developing embryo in the uterine lining but as the embryo and placenta inlarge it starts to to push its way into the cavity of the uterus. 05:09 As this occurs the placenta thins on one side and will eventually form more or less a pancake shaped structure on its attachment to the uterus and not be present outside the fetus beyond that. 05:22 As the embryo enlarges the chorionic cavity which contains the yolk sac will thin and the amniotic cavity shown here in blue will expand outward tremendously giving buoyancy to the fetus and supporting it as it moves, but also helping it resist gravity. 05:40 The portion of the endometrium, the lining of the uterus that's pushed outward as the embryo grows out of the uterine wall is going to be known as the decidua capsularis. 05:51 And the lining of the endometrium everywhere else is called the decidua parietalis. 05:57 At the point where the decidua parietalis of the uterine wall meets the decidua capsularis covering the developing fetus, we have an area called the decidua basalis and that's just marking the subdivisions of the endometrial lining as the fetus continues to develop. 06:13 As it develops, the fetus becomes larger and larger. 06:17 The placenta is more or less pushed to one side, and as I said before from is a relatively pancake shaped structure most likely on the posterior wall of the embryos of the uterus. 06:30 It's connected to the developing fetus by the umbilical cord, which is full of a loose mesenchyme called Wharton's jelly that surrounds the vessels that are traveling in the record to and from the placenta. 06:44 The membrane that supports the fetus consists of the amniotic membrane and then a smoothly chorion a very thin layer of the endometrium that was present when the fetus grew out of the uterine wall and then another smooth layer of the chorion this amniochorionic membrane is what ruptures when delivery is imminent and is known as the water breaking that allows the amniotic fluid to exit the birth canal and set the stage for a hopefully smooth delivery By the 14th or 15th week of pregnancy, there's enough amniotic fluid surrounding the developing fetus that we can safely sample some of it by a Amniocentesis. 07:26 This is generally done in order to check some genetic issues that may be arising in the fetus and looking for chromosomal abnormalities, markers of neural tube defects such as alpha-fetoprotein and other possible issues that might be anticipated. 07:40 Alternative way, the chorionic villi can be sampled and then taken for genetic analysis. 07:47 This can be done either through the anterior body wall using ultrasound or vaginally to harvest some of the chorionic villi.
About the Lecture
The lecture Placenta and Fetal Membranes by Peter Ward, PhD is from the course Conception, Implantation and Fetal Development.
Included Quiz Questions
What best describes the O2 content of the blood in the intervillous spaces?
- Lower than pure arterial blood because the maternal oxygenated and deoxygenated blood are both present
- Higher than pure arterial blood because fetal hemoglobin has a P50 of 19.0 mm
- Equal to the O2 content of arterial blood because it is directly supplied by the maternal (spiral) artery
- Equal to the O2 content of venous blood because it is directly supplied by the maternal vein
- Variable based on the needs of the developing fetus
What circumstance leads an Rh- mother’s immune system to mount a response against Rh+ fetal blood?
- Rh+ fetal blood expressing D antigen entering the maternal circulation causing the Rh- mother to release IgG antibodies and attack the fetal red blood cells
- Rh+ fetal blood expressing D antigen entering the maternal circulation causing the Rh- mother to release IgA antibodies and attack the fetal red blood cells
- Rh+ fetal blood expressing D antigen entering the maternal circulation causing the Rh- mother to release IgM antibodies and attack the fetal red blood cells
- Rh+ fetal blood expressing D antigen entering the maternal circulation causing the Rh- mother to release IgD antibodies and attack the fetal red blood cells
- Rh+ fetal blood expressing D antigen entering the maternal circulation causing the Rh- mother to release IgE antibodies and attack the fetal red blood cells
How does hemolytic disease of the fetus change with subsequent pregnancies?
- The response becomes more severe but can be controlled with Rh immunoglobulin
- The response is attenuated
- Subsequent pregnancies are not affected
- Subsequent pregnancies are not possible due to immediate IgG targeting
- The response is uncontrollable and becomes more severe
At what week of pregnancy can amniotic fluid be sampled, and what type of information can be ascertained through this process?
- By the 14th or 15th week amniotic fluid can be sampled via syringe and can assess for chromosomal abnormalities, fetal sex, neural tube defects, and other potential issues.
- By the 7th or 8th week amniotic fluid can be sampled via syringe and can assess for chromosomal abnormalities, fetal sex, neural tube defects, and other potential issues.
- By the 21st or 22nd week amniotic fluid can be sampled via syringe and can assess for chromosomal abnormalities, fetal sex, neural tube defects, and other potential issues.
- By the 14th or 15th week amniotic fluid can be sampled via syringe and can assess for fetal sex, but chromosomal abnormalities, neural tube defects, and other potential issues are only revealed through chorionic villi biopsy.
- By the 7th or 8th week amniotic fluid can be sampled via syringe and can assess for fetal sex, but chromosomal abnormalities, neural tube defects, and other potential issues are only revealed through chorionic villi biopsy.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |