Playlist
Show Playlist
Hide Playlist
Physical Exam Findings in Peripheral Artery Disease (PAD)
-
Reference List Physical Examination.pdf
-
Download Lecture Overview
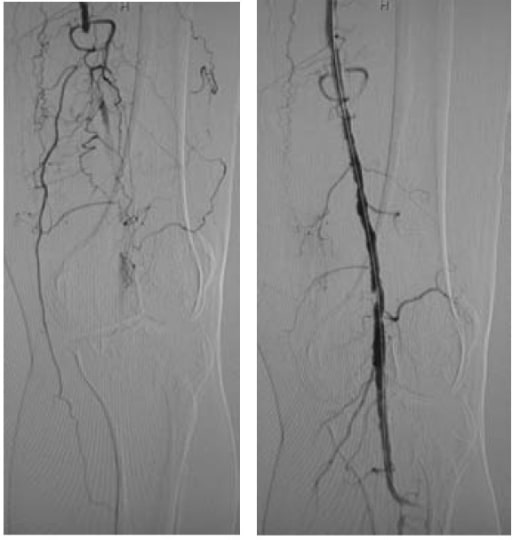
00:01 Alright, so now we're heading into the last section on our cardiovascular exam and we're focusing on the vasculature, and most notably, we're looking for peripheral arterial disease. 00:09 We've already talked about looking for peripheral edema in the prior section and how that distinguishes, how we can distinguish it from lymphedema, but now we're looking at the circulation itself, not so much the venous circulation but the arterial side. 00:21 There's a number of different findings that have variable levels of significance when making the diagnosis of peripheral arterial disease, and we can see very quickly just looking at our patient that the color of his legs looks good, he has hair on his toes here, there's no evidence of any ulcers either on the medial aspects or on the lateral aspects of his feet and there's evidence of good normal muscle bulk on both sides. 00:46 So this is not a person who we're likely to find significant arterial disease. 00:51 But there are three particular findings which can be really helpful to pickup potentially subclinical peripheral arterial disease, so let us look at those three aspects. 00:59 The first one's just temperature. 01:00 You know if somebody has significant peripheral arterial disease on one foot compared with the other, you can expect the temperature from one foot to the other is going to be different and sometimes you can compare temperatures by first putting your hands on like this and then swapping hands because you'll accentuate the difference between a cool limb and a warm limb. 01:19 Secondly, looking at the fill times for the capillary beds of the toes. 01:24 Simply you're going to squeeze a particular digit, you're going to watch the color dissipates, when I release it'll be pale and you want to see how quickly the color comes back to the toe. 01:36 But the third piece and the most important piece when you're trying to diagnose subclinical peripheral arterial disease or I should say disease that is manifesting with symptoms but is not showing up in obvious ways on the exam is the ankle-brachial indices. 01:54 This is essentially a test using simply a blood pressure cuff and a hand held Doppler to compare how well your arms are being perfused, peripheral arterial disease rarely manifests in the upper extremities, compared with how well is blood getting down into the lower extremities? And so, that what we're going to do next. 02:12 So after you've the patient lie down for a good five minutes to make sure the blood pressure has settled down, you'll simply going to check the blood pressure in the right arm first, so let's go ahead and do that. 02:35 Now one caveat I should say, by the way, I only went up to 160 cuz I know my patient here. 02:39 In general, if you've got somebody you are worried about peripheral arterial disease, you've gotta ratchet that up to probably 200 or so to make sure you're not missing occult hypertension. 02:49 Sometimes you can have this auscultatory gap between the first Korotkoff sound and the second, so always make sure you're going up to 200. 02:56 Anybody who has history of hypertension or any concerns of that nature. 03:00 Time to take the cuff off and move on to the next limb. 03:05 I like to go on a sequence from right upper extremity to right lower extremity then to left and then back up to the left arm as well. 03:11 You're going to take the highest pressure in each of those areas in this case the blood pressure cuff should go a few centimeters above the malleoli of the ankle, and in this case, the advantage is I'm not going to use my stethoscope anymore, instead it's time to use my handheld Doppler. 03:40 Now of course, if you don't have access to a handheld Doppler, you can just palpate the pulses and I'll show you how to do that in a moment, but if you have the advantage of one of these $80 or $100 handheld Doppler, it can be very helpful to augment the findings. 04:01 First off, I'm going to find out approximately where the pulse is. 04:04 The posterior tibial pulse is going to found on the medial malleolus back here. 04:09 I'm going to apply some ultrasound goo to my probe and turn it on. 04:23 So this is a nice biphasic pulse heading to the posterior tibial artery. 04:29 You can hear it has two peaks, that's systole -- the left ventricular contraction, and right after it is the elastic recoil of the aorta which is then pushing pressure in our diastole. 04:42 Now that I know where I am, I can squeeze the blood pressure cuff and we'll see what is pressure is in this area. 04:52 Great, and I think you heard the systolic pressure return very quickly at around a 130 which is the same as in the right upper extremity which is a good sign. 05:01 To be certain, we want also to check out the dorsalis pedis pulse, so we'll do that now. 05:09 Dorsalis pedis pulse is found about halfway down the midfoot and about medial or halfway between the top of the first MCP and over to the navicular bone, so oftentimes you'll find it around here. 05:22 It can be very variable, there's a lot of anatomic variation in patients. 05:25 I'm going to try and find it here just with my fingers first and again if I did not have the benefit of a handheld Doppler, I simply would be holding the pulse until I'm sure that it's firm, then I would inflate the cuff and mark accordingly. 05:40 Okay, I think I found his pulse so let's take a look and bring it to light. 05:59 Okay now that we've identified the dorsalis pedis pulse, let's see how quickly we can make it go away. 06:31 Okay, so with that we again got a pressure of around a 129 millimeters of mercury with his systolic pressure over his dorsalis pedis. 06:39 So now that we've got our numbers for our lower extremities and our upper extremities, let's talk about how to interpret them. 06:45 So you're going to end up with an ankle-brachial index for the left foot as well as for the right foot, and keep in mind that we don't focus as much on looking for peripheral arterial disease in the upper extremities cuz that's much, much, less common. 06:58 That been said there are some instances where you can have subclavian steal or other issues with carotid, I mean great vessel stenosis in the setting of Takayasu's disease and things like that which can lead to asymmetry in the upper extremity blood pressure and that's something to be mindful of or any aortic dissection for example, but for now we're talking about peripheral arterial disease and focusing on where the money is, which is really in the legs. 07:20 So starting with the left foot, so let's say with his dorsalis pedis pulse was a 115 or his dorsalis pedis systolic pressure was 115 and his posterior tibial systolic pressure was 110, we're going to take a higher of those values the 115 and you're going to compare that with whichever of the two arms yielded the highest systolic pressure, let's say it was 135 in this arm and 130 in the other. 07:46 So now we're taking the 135 here as the bottom of our fraction, the 115 from the left leg dorsalis pedis pressure and we're putting that on top of one another so we have 115 on top of 135 and that's going to yield a ratio, again, that's the ankle-brachial index for the left lower extremity and depending upon what that number is, whether it's less than 0.8 would suggest peripheral arterial disease, if it's less than 0.5 it suggest more advanced peripheral arterial disease and then values between 0.9 to 1.1 are considered normal. 08:22 Above 1.1 there are some idiosyncrasies about patients with diabetes that can complicate things as their arteries will get "hardened" and aren't quite as pliable and can end up with these falsely elevated ankle-brachial indices. 08:36 So now that would be the ABI we would have for the left, I'm guessing a 115 over 135 is probably around 0.8 or so whereas on the right leg, I would come up with a different ankle-brachial indices maybe that the dorsalis pedis and posterior tibial are both around 130, 135 which is compared as well with the systolic pressures in the upper extremities, and therefore the ABI would be around one which would be benign and we wouldn't worry about it. 09:02 If the patient has been reporting claudication symptoms with that achiness in the left calf after walking for a while and that correlates well with our ankle-brachial index of around 0.8 or lower, slam dunk. 09:14 It looks like somebody's got peripheral arterial disease. 09:17 So that wraps up our cardiovascular exam.
About the Lecture
The lecture Physical Exam Findings in Peripheral Artery Disease (PAD) by Stephen Holt, MD, MS is from the course Examination of Cardiovascular and Respiratory System.
Included Quiz Questions
What physical exam finding is more indicative of NORMAL peripheral arterial circulation than peripheral artery disease?
- Hair growth on feet
- Pallor after light pressure applied to the foot
- Cold to palpation
- Purple discoloration
- Presence of skin ulcers
What physical exam finding is more indicative of peripheral artery disease than normal peripheral arterial circulation?
- Pallor after light pressure applied to the foot
- Hair growth on feet
- Warm to palpation
- Pink color
- Strong pedal pulses
What is the primary indication for performing an ankle-brachial index test?
- Claudication
- Hypertension
- Chest pain
- Diabetes
- Hyperlipidemia
Which result indicates the most severe peripheral artery disease?
- Ankle-brachial index (ABI) < 0.5
- ABI < 0.8
- ABI < 1
- ABI > 1
- ABI > 2
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent , this is what I was waiting for. Thank you very much!