Playlist
Show Playlist
Hide Playlist
Peripheral Vascular Disease – Bypass Surgery
-
Slides Peripheral vascular disease Special Surgery.pdf
-
Download Lecture Overview
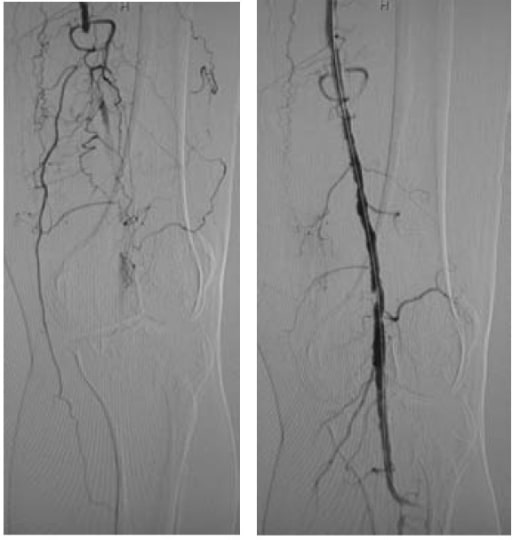
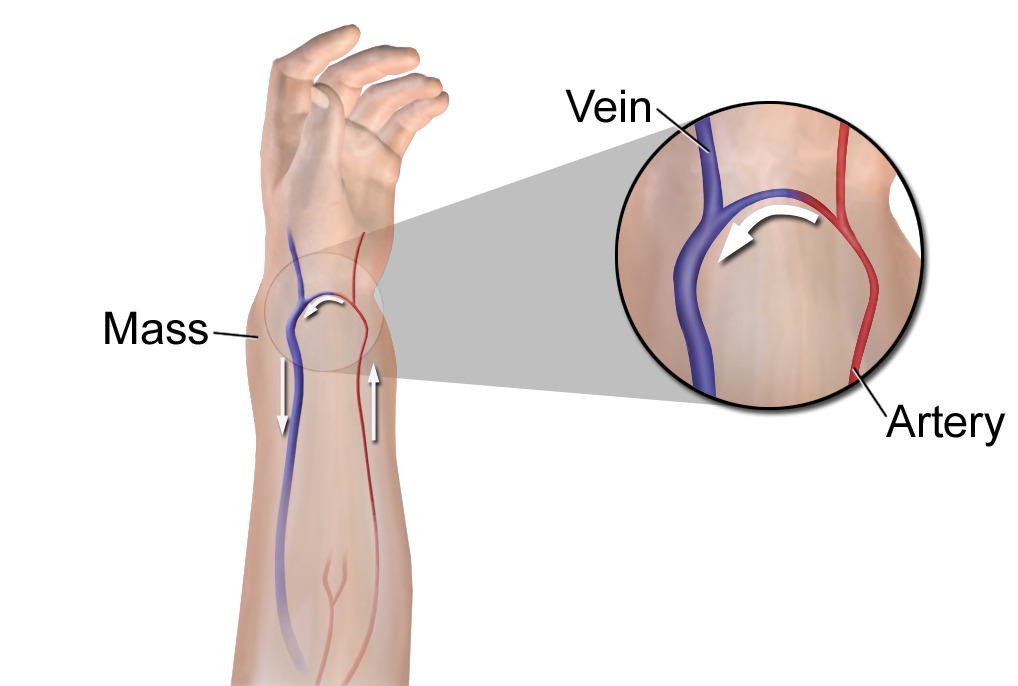
00:01 Here's an image of bypass surgery. 00:04 On this angiogram, the arrow demonstrates a mid-superficial femoral artery occlusion. 00:10 How do we fix this problem? That's right. 00:14 With a vascular bypass. 00:16 Here is a schematic of what happens in vascular surgery bypasses. 00:20 I enjoy vascular surgery because, conceptually, it's very straightforward. 00:25 We need to have excellent inflow. 00:28 We need to have excellent outflow. 00:30 And between the two, a bridging of conduit. 00:34 Any breakdown in any of those three elements can lead the patient to peripheral arterial occlusive disease. 00:40 As you can see in this schematic, the inflow on the left of the screen and the outflow appear normal in size. 00:47 However, this segment in the middle is stenotic. 00:51 There's going to be a significant flow and pressure differential as the vessel diameter goes from normal to stenotic or occlusive. 01:00 Vascular surgeons will then bypass this region as demonstrated by the arc. 01:05 In general, the bypass has the longest patency if we’re able to use a autogenous vein as opposed to synthetic graft. 01:15 Sometimes, it's not an option and grafts are used. 01:20 Let me pose another question to you. 01:23 Thus far, we've discussed atherosclerotic arterial occlusive disease. 01:27 What if the patient has a history of atrial fibrillation and now presents with an acute leg pain? What are your thoughts? What's going on in your mind? I'll give you a second to think about this. 01:41 Let's say, now you go to the bedside and examine the patient, but you feel no pulse in the dorsalis pedis or posterior tibial vessels. 01:49 And the contralateral extremity has strongly palpable posterior, tibial and dorsalis pedis pulses. 01:56 What's going on here? I’ll give you a second to think about this. 02:03 That's right. 02:04 The atrial fibrillation may have caused the clot, and that clot – called an embolus – likely dislodged from the heart and is now occluding a distal vessel. 02:13 This is considered an emergency. 02:16 Very important, if a clinical scenario is presented to you, this is considered an acute threatened extremity and intervention needs to occur right away. 02:26 If the question suggests, what is the next step of management, do you know what to do? First, we will usually use an unfractionated heparin drip. 02:38 The PTT goal is titrated and is variable. 02:42 This is to reduce further propagation of clot. 02:45 Next, most patients with threatened extremities require what's called a surgical embolectomy. 02:51 I’ll get to that in a second. 02:53 And lastly, when the embolectomy is completed, we want to make sure that flow has been restored. 02:58 This is done by an on-table angiography. 03:02 Here's an example of an embolectomy. 03:05 A Fogarty catheter is inserted into the vessel of interest, past the area where we think that there may be a clot, the balloon is inflated and the entire catheter is withdrawn. 03:17 The idea is, as a balloon is withdrawn, clots are brought out through the arteriotomy. 03:22 Here, you can see three large clots. 03:24 These clots, remember, in our patient, came from atrial thrombus. 03:29 After the clot is dislodged, we do an on-table completion angiography. 03:34 The angiogram then should show a normal flow to the distal vessels. 03:40 If the angiography shows persistent occlusion, you should try the Fogarty catheter again. 03:46 And as I mentioned, don't forget to do a completion angiography before closing the incision. 03:52 I’d like to pose another question to you. 03:54 What if this patient that had the atrial fibrillation and suspected of an embolic phenomenon and an acute threatened extremity has been experiencing a cold and pulseless extremity for now eight hours? What’s going on in your mind? What’s the next step of management? That's right. 04:13 You’re thinking compartment syndrome. 04:17 Here's a picture of a four-compartment fasciotomy. 04:20 Remember, any ischemic time greater than six hours puts the patient at a high risk of compartment syndrome. 04:28 Compartment syndrome occurs when edema in the region surpasses the ability of inflow and venous obstruction. 04:37 In these situations, it's usually related to a re-perfusion injury. 04:41 Remember, pulselessness, coldness of the foot are also late signs of arterial occlusive disease or embolic phenomenon. 04:51 Have a low threshold to perform a four-compartment fasciotomy. 04:54 Remember, you can do all the vascular bypass you want, patient is still going to lose their leg or foot if you don't complete your four compartment fasciotomy. 05:05 Now, let's move on to a different topic called Subclavian Steal Syndrome. 05:09 It's rarely seen, but a high-yield topic. 05:13 Subclavian Steal Syndrome occurs with retrograde vertebral artery flow due to a subclavian artery stenosis or occlusion. 05:23 As a result, you may find a reduced ipsilateral upper extremity, pulse or a blood pressure, typically described as a differential pressure between the affected arm and the normal arm. 05:34 As a result of the retrograde vertebral artery flow, the patient can experience syncope, vertigo and confusion. 05:41 This is due to the stealing of the blood from the vertebral artery. 05:45 As a reminder, the vertebral artery supplies the posterior circulation. 05:49 You’ll remember, of course, that the cerebellum contributes to one's positional sense and stability. 05:56 In severe cases of subclavian steal and subclavian artery stenosis, limb ischemia may occur. 06:04 And the treatment is a very advanced carotid to subclavian revascularization. 06:10 Here is a schematic depicting normal arch anatomy. 06:15 Notice the common carotid takeoff on the left side and the subsequent vertebral artery takeoff. 06:21 Now, let's review some high-yield information from peripheral vascular disease. 06:26 Remember, for patients with claudication, surgery is not the first line therapy. 06:31 You can add cilostazol, exercise, smoking cessation. 06:36 Remember, surgery is not the first line therapy. 06:41 Next, patients who present with a cold lake or pulseless should be considered a surgical emergency. 06:47 No further workup should be done. 06:49 The patient should be taken to the operating room and you can do your diagnoses and therapeutics on the table. 06:55 Therapeutically and diagnostically, angiographies are very important and can be performed intraoperatively. 07:04 And remember, any patient with a period of extremity ischemia are at high risk for compartment syndrome. 07:10 Before leaving the operating room, consider performing a four-compartment fasciotomy. 07:16 Thank you very much for joining me on this discussion of peripheral vascular disease.
About the Lecture
The lecture Peripheral Vascular Disease – Bypass Surgery by Kevin Pei, MD is from the course Special Surgery.
Included Quiz Questions
Subclavian artery stenosis causes which of the following phenomena that leads to subclavian steal syndrome?
- Retrograde vertebral artery flow
- Retrograde external carotid artery flow
- Retrograde common carotid artery flow
- Retrograde internal carotid artery flow
Which of the following options is the first-line treatment for claudication?
- Medication and lifestyle changes
- Cilostazol
- Surgical embolectomy
- Balloon angioplasty
- Primary amputation
A 45-year-old male comes to the emergency department because of a 9-hour history of a cold and painful left lower extremity. He also has a history of atrial fibrillation. There is no pulse in the dorsalis pedis or posterior tibial vessels. The contralateral extremity has strong, palpable pulses. What would be the first step in the surgical management of the patient?
- Heparin drip
- Arterial bypass surgery
- Balloon angioplasty
- Arterial stenting
- Embolectomy
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |