Playlist
Show Playlist
Hide Playlist
Peripheral Neuropathy: Diagnostic Testing
-
Slides Introduction to Neuropathy Disorders.pdf
-
Download Lecture Overview
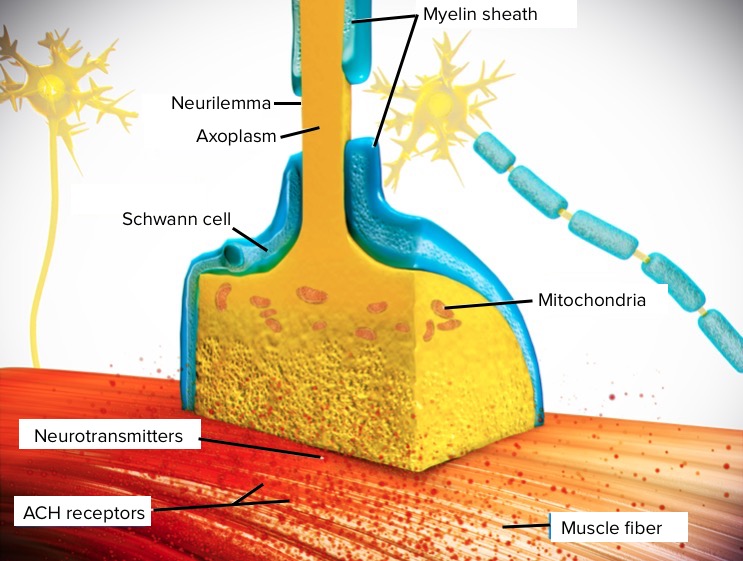
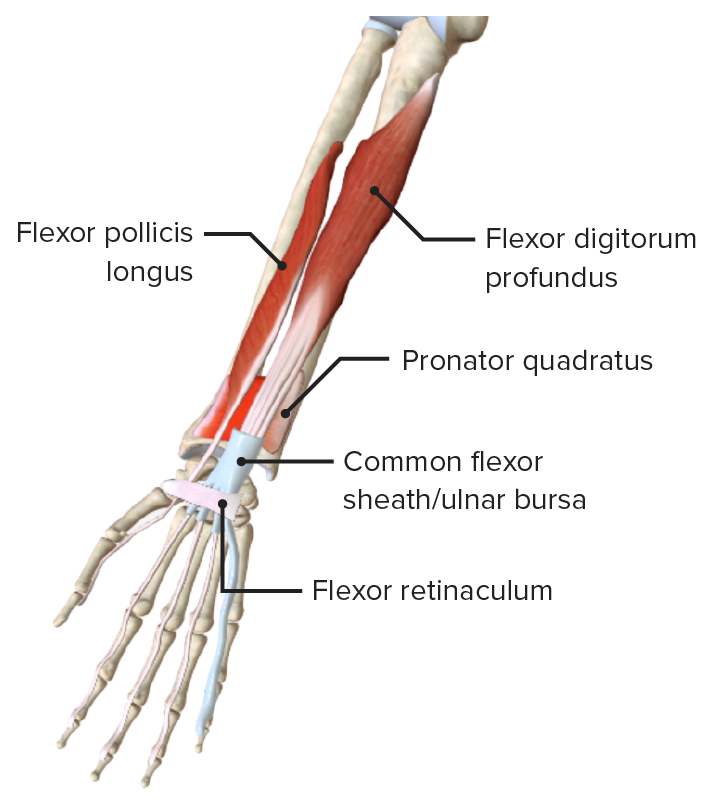
00:01 Now, let's talk about diagnostic testing. How do we evaluate the peripheral nerves? Well, it starts with our history, continues with the physical exam, but there are a number of studies that are essentially the extension of our physical exam that help us to determine where the neuropathy is coming from. 00:18 And here are some of the common studies that are performed, and we'll walk through a few of these. 00:22 Nerve conduction studies, electromyography, repetitive nerve stimulation, single fiber EMG, stimulated single fiber EMG, and neuromuscular ultrasound. 00:33 And I'd like for you to understand how we perform some of these studies and the information it gives us, and how it helps us to take a broad differential diagnosis and narrowed into a single leading or multiple leading diagnosis. 00:46 Let's start with the nerve conduction study. 00:48 Nerve conduction studies evaluate peripheral nerve complaints, things like weakness or numbness, by measuring a number of aspects of how the nerve is functioning. 00:57 We can look at the amplitude of a nerve firing and that tells us about the axonal integrity. 01:02 We look at the latency and speed of nerve potentials or nerve action potentials, which tells us about the myelin and the axon. 01:11 And we can look at both sensory problems and motor problems and sensory motor nerve dysfunction. 01:17 In general, when we're conducting a nerve conduction study, as you can see in the schematic, we have a stimulating electrode that will send a pulse, it will shock the nerve, in a recording electrode. 01:27 We can record on sensory nerves where we're looking at the integrity of the sensory nerve. 01:32 We shocked the sensory nerve and measured the signal down the sensory nerve and we're looking for an interruption. Or we can measure the muscle. 01:39 Shock the sensory nerve, and we record in the muscle, and we're measuring the integrity of that sensor - of that motor nerve travelling down and synapsing in the neuromuscular junction to activate the muscle. 01:52 We commonly test a number of different nerves to evaluate which nerves are involved in a peripheral neuropathy. 01:59 Some of the motor nerves that are commonly tested include the tibial and fibular, as well as median and ulnar, which are mixed nerves. 02:05 We can look at pure sensory nerves like the sural nerve or median and ulnar, again, which are mixed nerves. They carry both sensory and motor information. 02:14 And other mixed nerves can be evaluated as well. 02:17 And we're putting all this information together to understand whether the neuropathy is sensory only, motor only, sensory and motor, or whether something else appears to be the problem. 02:27 Now, let's talk about how we conduct a nerve conduction study. 02:30 Interpretation of the study really involves a logical and stepwise progression through the test. 02:35 And I'm going to talk about the four steps that we use to walk through a nerve conduction study. 02:41 The first is we evaluate for sensory involvement. 02:44 And if there is sensory involvement in a neuropathy, we're worried about problems with the nerve plexus or the terminal nerve branches. 02:52 If there are no sensory findings on our nerve conduction test, there may still be a nerve problem, but it may be in the nerve root, which is a problem proximal to the dorsal root ganglion that we don't see on the nerve conduction study. 03:05 Or it may mean that the problem is not in the nerve at all. 03:08 And it's a neuronopathy or a neuromuscular junction disorder or a problem in the muscle. 03:13 Our second step is to evaluate the part of the nerve that is involved. 03:18 Is the myelin affected, the axon affected, or both? We look for demyelinating neuropathies by looking at things like the distal latency and conduction velocity. 03:28 We're looking at how fast that signal travels down the nerve. 03:31 Loss of the myelin results in slowing of the signal travelling down the nerve. 03:37 We can also look for findings that would support an axonal neuropathy. 03:41 The axons are all of the things they're sending the signal. 03:44 So, a reduction in the number of axons really leads to a reduction in the amplitude of the signal. 03:51 And then, lastly, our fourth step is to look for symmetry. 03:54 Often, things that are inherited present very symmetrically and things that are acquired may present asymmetrically. 04:02 When we do a nerve conduction study, we evaluate the sensory nerves and the motor nerves. 04:07 Our sensory nerve evaluation begins with interrogating the sensory nerve action potential. 04:14 This is a summation of all sensory nerve fiber action potentials into the SNAP or the sensory nerve action potential. 04:23 We're shocking a sensory nerve and measuring distally at that - at a sensory nerve ending and evaluating for some pathology that may be impairing the signal. 04:33 Some of the parameters that we look at in the SNAP or sensory nerve action potential are the latency. 04:39 How quick does it take that signal to travel down a sensory nerve? And we can look at the peak latency or the onset latency to tell us how the sensory nerve is functioning. 04:48 We also look at the amplitude. 04:50 From baseline to peak and from peak to peak, what's the size of that signal? How many nerves are able to fire? And you can see here a schematic of how we conduct a sensory nerve action potential. 05:00 We have a stimulating electrode at one part of the nerve and a recording electrode at the other part of the sensory nerve. 05:06 We can measure orthodromically down the sensory nerve or antidromically up the sensory nerve. 05:13 And both of those signals will give us information about the integrity of the sensory nerve. 05:18 Lastly, we can look at the conduction velocity and this is really important. 05:24 This is a calculation about how fast signal is travelling down a sensory nerve. 05:28 We see reduced conduction velocity in demyelinating neuropathies. 05:33 And so, looking at the conduction or speed of the signal is critically important in evaluating patients who present with neuropathy. 05:41 The second step is to evaluate the muscles and the motor nerves. 05:44 And we do that with the compound muscle action potential. 05:48 Here, we're stimulating the sensor - excuse me, here, we're stimulating the nerve and recording at the muscle and looking at muscle contraction. 05:56 We stimulate nerve axons, and this causes the muscle to contract, and we record at the body of a muscle. Responses are typically in millivolts, which is much larger than our sensory nerve action potentials. 06:09 And you can see the type of recording we get here. 06:11 That up and downward deflection is contraction of the muscle. 06:15 We can look at the onset of the signal, the peak latency of the signal, and the amplitude of contraction. 06:21 Problems with the motor nerves or with the neuromuscular junction and muscle can result in loss of amplitude when there's less nerves that are able to fire or slowing of the latency or conduction velocity when the motor nerves are demyelinated. 06:36 So, what is the compound muscle action potential? It is the summation of all stimulus action potentials from many muscle fibers in the same area. 06:46 It's the signal recorded as a result from depolarization of all the muscle fibers innervated by a single motor nerve. 06:53 Unfortunately, we can't pick out individual nerve fibers in the muscle fibers that they innervate. 06:58 We shock the entire motor nerve and look at action potentials down all of its branches into all of the muscles that it innervates. 07:07 We use these findings, the SNAPs and CMAPs to look at the pattern of nerve involvement. 07:14 Amplitude - reduction in amplitude of CMAP or SNAP points towards an axonal pattern of disease, and there are a number of conditions that primarily affect the nerve axon. 07:24 So, when we see reduction in amplitude, we think about the axonal neuropathies. 07:29 Distal latency, which is the amount of time between a stimulus and that electrographic response is prolonged in demyelinating disorders. 07:40 And so, problems with distal latency or prolonged distal latency suggest a demyelinating pattern. 07:46 And then, lastly, the conduction velocity is a very important component of the nerve conduction study. 07:51 This is the speed of the action potential from stimulus to recording site. 07:55 And problems with conduction velocity or reduction in conduction velocity may suggest a demyelinating pattern. So, when we interpret CMAPs and SNAPs, the nerve conduction velocity study, we're looking for axonal findings and axonal patterns such as low amplitude, which results from fewer axons being able to be fired, and slowed conduction velocity, which is not as prominent as what we see in demyelinating neuropathies. 08:23 The demyelinating pattern is a reduction in speed and velocity of the signal. 08:27 We see prolonged distal latency, markedly slowed conduction velocity, prolonged F waves, which also tell us about the integrity of the entire sensory motor loop, and we can see conduction block where there is a decrement between the distal and proximal sites of a nerve stimulus. 08:47 Now, let's talk about electromyography. 08:50 Typically, when patients are undergoing electrodiagnostic studies, it starts with the nerve conduction study, and then ends with electromyography. 08:58 The EMG is the needle examination where we evaluate the nerve and the muscle integrity through assessment of spontaneous and activated muscle movements through a needle examination. 09:10 In this test, we use both recording electrodes, and you can see those pads placed on this patient's arm, and an activating needle. 09:18 This is a very, very thin, small needle that's inserted into the muscle, and the needle listens to what the muscle is doing. 09:25 We're listening to the muscle at rest to see whether the muscle will spontaneously move or depolarize, which would be abnormal, and then looking at the degree of activation of the muscle as a result of active contraction. 09:38 The normal resting membrane potential of the muscle is minus 70 to minus 90, and we're looking at changes in that resting and action potential to guide us in terms of the types of pathology that may be causing the patient's symptoms. 09:53 Interpretation of the EMG also involves a logical and stepwise progression through this part of the test. 09:59 First, we want to know, does the problem appear neurogenic? Is it a neuropathy where we see reduced recruitment? When the muscle tries to activate, we can't activate other muscles to help support motor function, and this results from neuropathy. 10:14 Or do we see a myopathic pattern where there's early recruitment of extra muscles? When the muscles are damaged, the nerves work, they tell that we can't generate as strong of a force, and they quickly recruit other muscles to help us to generate a force. 10:28 So, we're looking for neurogenic patterns that suggest a nerve problem or myopathic patterns that suggests a muscle disorder. 10:36 The second thing we're looking for is whether this problem is acute or chronic. 10:40 Acute problems often cause small, short motor units, whereas chronic neurogenic problems cause long, large motor units, and this is a result of reinnervation. 10:50 In a chronic neurogenic or neuropathic disorder, there's reinnervation of muscles, and this results in larger units, more muscles that are recruited by a single nerve. 11:00 Third, we want to know whether the problem is acute or resolved. 11:04 Acute problems are also often characterized by increased spontaneous activity. 11:10 Right when a muscle is denervated, we see the muscle fires on its own spontaneously. 11:15 Over time, as a problem resolves, we don't see that spontaneous activity which goes away, and so the present spontaneous contraction of the muscle guides us in terms of whether this is an acute new or a chronic resolved problem. 11:28 And then, we can also look at ancillary findings to support specific neurogenic pathology. 11:35 Next, let's talk about neuromuscular ultrasound. 11:37 This is one of the latest tests to be used to evaluate peripheral nerve and muscle disorders. 11:42 Diagnostic ultrasound is also called sonography. 11:45 It's where we use sound waves to evaluate the nerve, the muscle, and the peripheral nervous system and body. 11:51 We use high frequency sound waves to pierce through the skin and tissues within the body and produce an image or echogenicity contrast as a result of how the sound waves reflect off of different densities of material. 12:06 Neuromuscular ultrasound focuses on the peripheral nerve and sometimes the muscle and surrounding structures to determine types of pathology that may cause patient symptoms. 12:15 And there are a number of advantages of neuromuscular ultrasound over our typical nerve conduction study and EMG. 12:21 And this includes that ultrasound is painless. It doesn't hurt. 12:24 We're not sticking needles into muscles or shocking nerves to evaluate the patient. 12:29 So, often well tolerated and safe and can be very effective, particularly in children where nerve conduction and EMG can be quite difficult. 12:36 This also gives us the ability to evaluate dynamically how the peripheral nervous system is interacting with the surrounding. 12:43 We can look at vascularity at the mobility of a muscle or a nerve and use that to help guide us. 12:49 Let's look at an example of what a neuromuscular ultrasound or an ultrasound picture looks like of a nerve. Here, we see a typical picture. 12:58 This is the right median nerve. We're looking at the median nerve in cross section. 13:02 So, we've basically taken off the hand and we're looking inside at the wrist and cross section. 13:09 The surface of the skin is at the top and the deep part of the body is at the bottom. 13:14 So, we're really looking right back through the wrist in cross section. 13:20 Here, we're looking at the median nerve, which is this very large structure that we're looking at in high resolution. I can draw a line around the median nerve. 13:28 And so, you can see its circumference. 13:31 And we can also see all of the little nerve fascicles which are those dark spots within the nerve. 13:36 With median nerve pathology like carpal tunnel, we see that the median nerve swells, and so the perimeter of the nerve is increased. 13:43 We can also see changes in individual character of the nerve fascicles. 13:48 We can see increased echogenicity or whiteness in certain disorders and decreased echogenicity in others. 13:55 This is a very helpful tool to evaluate specific pathology within the peripheral nerve. 14:00 All right. Let's put it all together. When we think about electrodiagnostic testing, how does this help us to differentiate different types of disorders? Here, we're going to look at a number of things that we do with electrodiagnostic testing. 14:17 We look at the conduction velocity, which tells us about the myelin. 14:20 The CMAP amplitude, which tells us about the number of axons in a motor nerve. 14:24 The SNAP amplitude, which tells us the number of axons in a sensory nerve. 14:28 We can use repetitive stimulation to repeatedly shock and evaluate a nerve and see whether there is fatiguability or problem with the neuromuscular junction. 14:38 And then, we can also perform our EMG study to see what type of neuropathic or myopathic process may be going on. 14:45 Let's start down at the bottom of this table with upper motor neuron disorders, things in the central nervous system. 14:51 We really don't see any problems with EMG nerve conduction study. 14:54 Conduction velocity is normal, the signal is propagated down the nerve normally. 14:59 The CMAP, the motor nerves, the SNAP, the sensory nerves work normally. 15:03 There's not a problem with repetitive activation of a nerve in neuromuscular junction. 15:08 And when we stick our needle into the muscle, there's not changes that are occurring out in the peripheral nervous system. 15:13 So, everything is normal in an upper motor neuron or central nervous system disorder. 15:18 And in those patients, we need to interrogate the central nervous system. 15:21 With muscle diseases, we don't see a problem with conduction velocity because the nerve is normal. We do see reduced CMAP amplitude, so there's less contraction of the muscle as a result of the muscle disease. 15:34 The sensory nerves are normal. 15:36 We don't see a problem with the neuromuscular junction with repetitive stimulation. 15:39 And often our motor units are small. Small myopathic motor units on EMG. 15:46 With neuromuscular junction disorders, again, the conduction velocity is normal because the nerve is unaffected. 15:53 Our motor nerves and our sensory nerves are normal, but the problem is a decrement or decreased CMAP on repetitive stimulation. 16:01 As we repeatedly and repetitively activate that nerve, we see less and less response as a result of pathology in the neuromuscular junction. 16:10 With peripheral polyneuropathies that are demyelinating, we see a reduction in conduction velocity because that's really interrogating the speed of the signal travelling down the nerve. 16:20 We may see normal or reduced CMAP amplitude and SNAP amplitude. 16:25 We don't see a decrement with repetitive stimulation, there's not a problem with the neuromuscular junction, and motor units may be enlarged or normal. 16:33 With axonal polyneuropathies, the conduction velocity is normal because the speed travelling down the nerve is normal, but we see significant reductions in CMAP amplitude, and potentially SNAP amplitude if the sensory nerves are involved. 16:46 There's no problem with repetitive stimulation because it's not a neuromuscular junction disorder, and here, the motor units are large, particularly in chronic or reinnervated conditions.
About the Lecture
The lecture Peripheral Neuropathy: Diagnostic Testing by Roy Strowd, MD is from the course Introduction to Neuropathy Disorders.
Included Quiz Questions
Which of the following is typically the first electrodiagnostic study used to evaluate peripheral neuropathies?
- Nerve conduction study
- Electromyography
- Electroencephalogram
- Neuromuscular ultrasound
- Electrocardiogram
Which of the following tests uses a needle electrode to assess the integrity of the nerve and muscle at rest and when activated?
- Electromyography
- Nerve conduction study
- Neuromuscular ultrasound
- Electroencephalogram
- Echocardiography
Which of the following locations is most likely to be affected when decreased sensation is found during a nerve conduction study?
- Nerve plexus
- Neuromuscular junction
- Nerve cell body
- Ventral nerve root
- Muscle
Which of the following findings is consistent with axonal pathology during a nerve conduction study?
- Reduced amplitude
- Increased amplitude
- Reduced distal latency
- Prolonged distal latency
- Increased conduction velocity
A neurogenic pattern on electromyography will show which of the following?
- Reduced muscular recruitment
- Increased muscular recruitment
- Early muscular recruitment
- Late muscular recruitment
- Normal muscular recruitment
Which of the following is an advantage of using neuromuscular ultrasound compared to electromyography?
- It is painless.
- It is a static depiction of the nerve.
- It is an easier way to estimate conduction velocity.
- It is a quantifiable way to see how many motor units are being recruited.
- It is the best way to quantify the sensory loss in a dermatome.
Which structure is typically seen at the top of the screen when performing a neuromuscular ultrasound?
- Skin
- Nerve
- Nerve sheath
- Muscle
- Subcutaneous fat
Which of the following disease states is most likely to show a decreasing CMAP amplitude with each stimulation?
- A neuromuscular junction disorder
- An upper motor neuron lesion
- An anterior horn cell disorder
- A muscular disorder
- A demyelinating polyneuropathy
Which of the following disease states is most likely to show decreases in conduction velocity?
- A demyelinating polyneuropathy
- A muscular disorder
- An anterior horn cell disorder
- An upper motor neuron lesion
- A neuromuscular junction disorder
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |