Playlist
Show Playlist
Hide Playlist
Peripheral Arterial Disease: Diagnosis and Treatment
-
Slides VascularDisease CardiovascularPathology.pdf
-
Download Lecture Overview
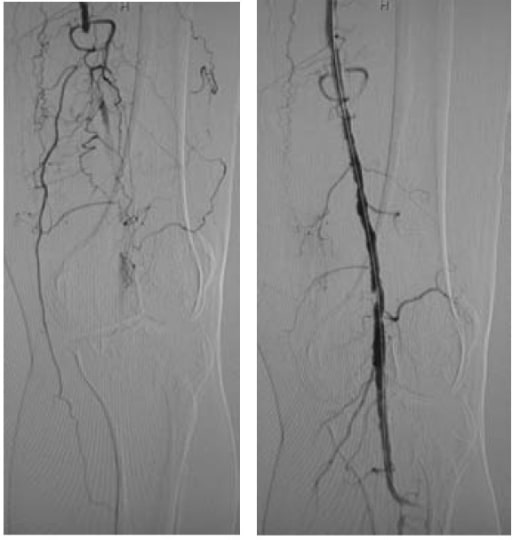
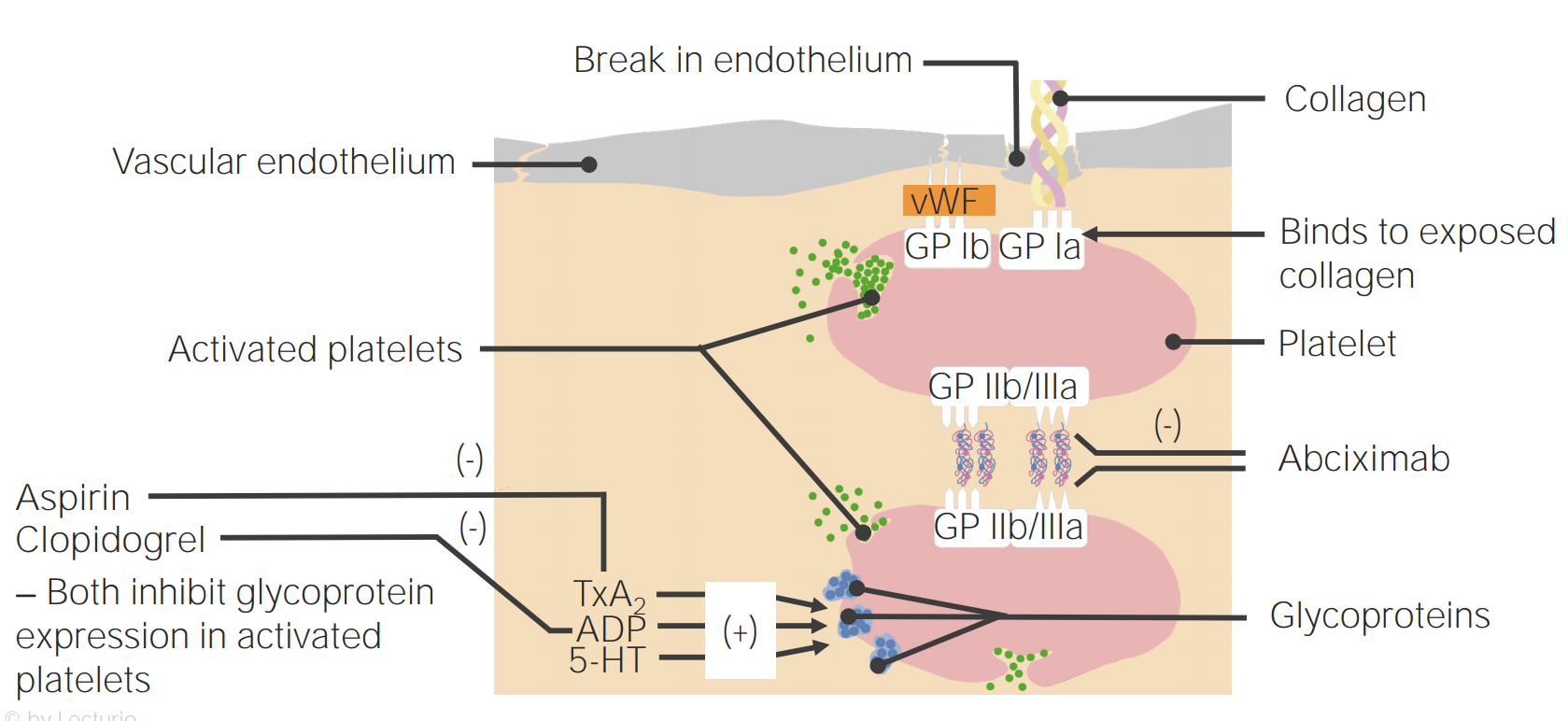
00:01 Clinical history. Well, setting of the risk factors would be exactly as to what we talked about earlier with coronary arterial disease and we'll look into that in a little bit. 00:10 Non-invasive testing, okay, so now, this would be the first time in which we're not using the EKG obviously here. It makes no sense. 00:19 We're not in the heart, we're down in the periphery, okay? So, what kind of non-invasive test? How important is this? Really important. 00:25 Because the more that you are able to come up with non-invasive testing and it being efficient and effective, the better off you'll be in every possible way. 00:35 You'll be respected by your peers and in terms of next step in management, any question that you get, here it is. 00:41 It's called ankle-brachial index and that's the one that we'll pay attention to. 00:45 Now, there are a couple of others that you may do as well, but at least, get this one down. 00:49 Once you have understood ABI, ankle-brachial-index, in other words, you're going to take or you're going to measure the pressure in the ankle. 01:02 You're going to measure the pressure in the brachial, upper extremity, are you there? And you're gonna do a ratio. When you do that ratio, you're gonna get a particular number and this is what I'd like for you to understand. 01:17 You can sit there and memorize all this stuff but why would you wanna do that? In the long run, it's really not gonna help you. There's just too much to memorize. 01:24 Really, just too much to memorize, isn't it? So, what I'd like for you to do is think about, well, what exactly is happening with the pressures in the two extremities and what can you expect with the ratio and once you do that, you're gonna be much better off and we will, ladies and gentlemen, we'll be doing this and we have been doing this for every single organ system from like BUN:creatinine ratio to, you know, tubular fluid to plasm ratio in nephrology, I mean you name it. Every type of ratio that we've done has been the fact that it's all about understanding and what you can expect normally so that you can then identify the abnormal. 01:58 So, take a look at this. So, we're gonna do either right or left and we'll put both up here and ankle A, then, brachial, do alphabetical order. 02:08 The ankle will be on top, this is the ratio, the math, the ankle will be on top, A, the B, brachial will be in the denominator as you see here, okay? So, that would mean ankle and then, you have your brachial, the arm. 02:22 The blood pressure in the arm and the leg should normally be about the same. 02:26 For example, if the arm systolic blood pressure was one 30 millimeters of mercury in the leg, systolic blood pressure was one 20 millimeters of mercury that would give you an ankle brachial ratio index of one 20 over one 30 or 0.92, which is considered normal if the blood pressure was significantly lower in the leg, then that would give you an ankle brachial index below 0.9 indicating peripheral vascular disease. 02:48 Why are we doing this? Because we're trying to identify non-invasively whether or not your patient is suffering from peripheral arterial disease. 02:56 Okay, now, use common sense now. If this peripheral arterial disease, am I supplying adequate amounts of blood down to the dorsalis pedis? Of course, not. So, what would you expect that pulse and the pressure to be? Decreased, are we clear? Of course, not. So, what would you expect that pulse and the pressure to be? Decreased, are we clear? Let's move on and let's confirm this. You measure your ABI, interpretation of it. 03:18 Abnormal, absent pedal pulses. I can't feel it. Age, greater than 20 and you find that your patient has a history of smoking, diabetes mellitus, wow, that's gonna confirm this noninvasively. 03:32 You find your ABI, ankle-brachial index to be less than 0.9. 03:39 Please know that you have confirmed diagnostic of peripheral arterial disease. 03:47 Once you find the lower ratio, what have you done? You've confirmed PAD. 03:51 What exactly is that number? Less than 0.9. Then, you memorize the number. 03:56 You do that every single time with the Fractional Excretion of Sodium later on in nephrology. 04:01 You understand the concept first, and then, you memorize the numbers if you must but the concept will never leave you. Let's do another one. 04:10 This is normal. Between 0.9 and you can go all the way up to 1.3. 04:14 The ankle pressure is a little bit -- a little bit higher. 04:18 So, therefore, this is normal, no further testing is required. 04:21 What if you find your ankle to brachial index to be greater than 1.3? Then, your next step in management is your Doppler. 04:30 So, now, you started thinking about ultrasound and such, duplex Doppler or something else called toe pressure. Just keep these in mind as your next step of management. 04:38 If you find your ABI to be greater than 1.3. Less than, take a look, we've confirmed PAD. 04:45 Now, if it is greater than 1.3 and you found this to be confirmed with a Doppler waveform, then, you started thinking about diabetes mellitus and even end stage renal disease may have falsely elevated levels. Renal failure in nephrology. 05:04 We've talked about quite a bit with end stage renal disease and there, oftentimes, you find your blood pressure to be quite high, don't you, right? Why? Because you don't have proper GFR, cuz if your GFR drops, then, you're going to build up more volume. Welcome to hypertension. 05:20 So, you might have falsely elevated levels with ESRD, end stage renal disease. 05:26 At this point, your focus should be peripheral arterial disease and how we confirm that by having a low ratio. Let us move on. 05:34 Modifiable risk factors, these are the same ones that we saw earlier with any type of atherosclerotic disease. 05:40 These include if you can try to implement, implement smoking cessation programs, blood glucose level for diabetes, the treatment of dyslipidemia. 05:51 Here treatment of hypertension, all these are modifiable risk factors. 05:56 Conservative treatment of peripheral vascular disease includes exercise and antiplatelet medications such as aspirin, clopidogrel or similar drugs for patients with worsening claudication at rest. 06:05 Pain. 06:06 Then patients may need surgical bypass in the lower extremities. 06:10 Amputation may be necessary for complications such as infected ulcers or gangrene.
About the Lecture
The lecture Peripheral Arterial Disease: Diagnosis and Treatment by Carlo Raj, MD is from the course Arrhythmias: Basic Principles with Carlo Raj.
Included Quiz Questions
What is the diagnostic test of choice for peripheral arterial disease?
- Ankle-brachial index (ABI)
- Doppler waveform
- Duplex doppler
- Glomerular filtration rate (GFR)
- Arterial blood gas (ABG)
Which of the following is a modifiable risk factor in peripheral arterial disease?
- All the above
- Smoking
- Hypertension
- Dyslipidemia
- Glucose control
Which of the following is not true regarding an ABI that is greater than 1.3?
- Combined with Doppler waveform, it can point towards vasculitis.
- Combined with Doppler waveform, it can point towards diabetes mellitus.
- Combined with Doppler waveform, it can point towards endstage renal disease with falsely elevated levels.
- Duplex doppler must be pursued when ABI is greater than 1.3.
- Pressure in the toes must be measured when ABI is greater than 1.3.
Which of the following is not true about the ankle-brachial index?
- Ankle pressure is greater than the arm pressure.
- Ankle pressure is less than the arm pressure.
- ABI ratio of 0.91 to 1.3 is considered normal.
- ABI of less than 0.91 is considered diagnostic of PAD.
- ABI greater than 1.3 may indicate non-compressible arteries.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |