Playlist
Show Playlist
Hide Playlist
Perimenopause
-
Slides MenopauseManagement Menopause.pdf
-
Download Lecture Overview
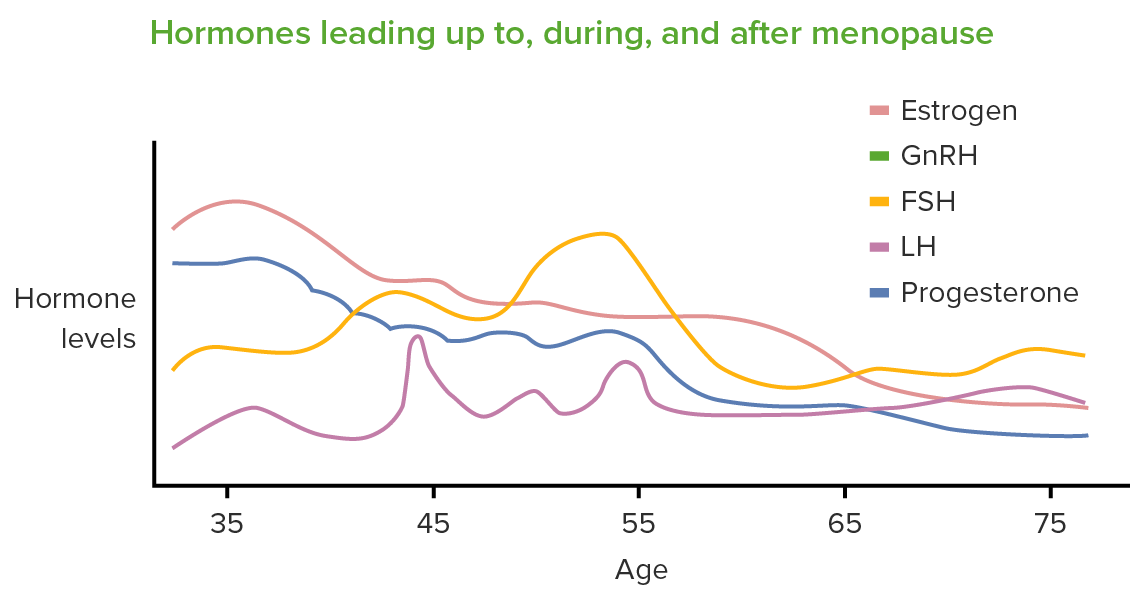
00:01 Hi. Now we're gonna talk about menopause management. 00:05 What's the difference between menopause and the perimenopause? Are they really that different? Well, let's see. 00:13 Menopause is the permanent cessation of menses due to decreases in ovarian estrogen production. 00:19 This is evidenced by 12 consecutive months of no menstrual bleeding. 00:24 So it's usually a retroactive diagnosis versus the perimenopause or the climacteric which is the transitional period which can occur from 2 to 8 years from reproductive to nonreproductive stage. This is marked by a menstrual irregularity. 00:40 Let's review how the perimenopause works. In another lecture we reviewed oogenesis. 00:48 Oogenesis begins at 4 weeks and the peak oogenesis occurs mid gestation and then we lose follicles through atresia after that time through birth, puberty, and all the way to the menopause. At birth, we have 1 to 2 million oocytes in our ovarian reserve. By puberty we have about half a million and by the age 30 to 35 when you're advanced maternal age you have a hundred thousand. By the time we get to menopause, we have less than a thousand. 01:18 Let's talk about the hormones that are actually increased. 01:24 So we know that follicle-stimulating hormone or FSH increases during the menopausal period. 01:30 We also see a corresponding decrease in estradiol production. 01:34 So mechanisms that increase FSH are follicular atresia leading to decreased ovulation, decreased estradiol, and that increases FSH. 01:44 The remaining aging follicles exhibit diminished capacity to secrete inhibin B. 01:51 This also leads to increased FSH. Premenopausal FSH level should be less than 10 ideally. Sometimes in the perimenopause we can already start to see an elevation in the FSH and by postmenopause we see that the FSH is greater than 30. 02:09 In the perimenopause be careful, women can still become pregnant and in fact they're more likely to ovulate twice and have twins. 02:17 Let's now talk about estrogens. Estrogen levels do not gradually wane, but remain stable and at sometimes they are slightly elevated due to the high FSH. 02:28 Let's talk about the different types of estrogens. 02:32 We have E2 or estradiol and estrone. Estradiol seems to be the only one to decrease less than a year before menopause so when premenopausal women usually we make about 30-200pg/ml. 02:48 In the postmenopause, we have much less at 25-30pg/ml. 02:54 We're gonna talk about how that feels for a woman after being exposed to estrogen her entire reproductive life and then losing estrogen. Then we're gonna talk about estrone. 03:04 This is an extragonadal estrogen as it's usually made peripherally but can also be made in the ovary. This is the primary estrogen in the menopausal woman and the premenopausal levels are between 35-500pg/ml and the postmenopausal range it's 10-15pg/ml. 03:22 So how does this work? The hypothalamus usually gives input through FSH to the ovary. Typically, FSH works upon the ovary to make steroidogenesis actually occur with the addition of luteinizing hormone. 03:40 Aromatase converts androgens to estrogens and the estrogens feedback to the pituitary and the hypothalamus. 03:48 This happens when we are in our normal reproductive phase. 03:50 Aromatase in the postmenopausal woman actually causes peripheral estrogen production, primarily estrone, which also feeds back to the hypothalamus and pituitary. 04:03 Let's now discuss the endocrine profile in the perimenopause. 04:07 I don't want you to think that you need to check hormone profiles on women to determine if they're in their perimenopause or menopause. 04:13 Remember that menopause is a clinical retroactive or retrospective diagnosis that you can only make after the patient has 12 consecutive months with no menstrual bleeding. However, I do wanna call your attention to the fact that there are some hormones that start to decrease or increase in the perimenopause. One such hormone is anti-mullerian hormone and it starts to decrease to undetectable levels, 5 years before the final menstrual period and the decreasing AMH actually corresponds to an increase chance of twinning. 04:44 Therefore, women in their perimenopause need adequate contraception. 04:48 Let's now review inhibin B. Inhibin B starts to decrease in women who are 35 years of age and older. 04:56 Remember that 35 years of age in obstetrics is advance maternal age. 05:02 Finally, luteinizing hormone, because of the decrease in inhibitory factors LH is increased during the menopause. 05:10 Lastly, testosterone decreases by about 25% due to adrenal cortex hypoplasia and the loss of cyclical LH surges.
About the Lecture
The lecture Perimenopause by Lynae Brayboy, MD is from the course Menopause.
Included Quiz Questions
When is the peak of oogenesis?
- At mid-gestation (approximately 20 weeks after conception)
- During the early gestational period
- At birth
- At puberty
- During reproductive age
Which of the following best describes the hormonal profile of a woman in perimenopause in comparison to a normally menstruating woman?
- Testosterone - decreases; LH - increases; FSH - increases; Anti-Müllerian hormone - decreases
- Testosterone - increases; LH - increases; FSH - increases; Anti-Müllerian hormone - decreases
- Testosterone - decreases; LH - decreases; FSH - decreases; Anti-Müllerian hormone - increases
- Testosterone - decreases; LH - decreases; FSH - decreases; Anti-Müllerian hormone - decreases
- Testosterone - decreases; LH - increases; FSH - decreases; Anti-Müllerian hormone - decreases
A 50-year-old woman comes to the general clinic for hot flushes and sweating. She also describes a mild bloating sensation and feels she has put on weight. Her hormonal profile reveals testosterone and inhibin being decreased and FSH and LH being increased. What is the next best step in management?
- Explain that the profile matches a normal perimenopausal woman.
- Explain the need to screen and monitor ovarian cancer.
- Explain that the profile matches a normal postmenopausal woman.
- Explain that the profile matches a normally menstruating woman.
- Explain that the hormonal profile is inconclusive and is NOT the best way to diagnose her condition.
Which of the following is a FALSE statement regarding perimenopause and menopause?
- Follicular atresia causes a decrease in estradiol production causing a decrease in FSH.
- Oogenesis begins at 4 weeks of gestation and the number of oocytes decreases as age increases.
- The decrease in the anti-Müllerian hormone increases the chances of twinning in pregnancy.
- Aging follicles decrease the amount of inhibin formation and can cause an increase in FSH.
- The decrease in the inhibitory factors causes an increase in LH.
By definition, how long must a woman go without menstruating to be considered to have attained menopause?
- 12 consecutive months
- 12 months intermittently
- 6 consecutive months
- 6 months intermittently
- 24 months intermittently
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |