Playlist
Show Playlist
Hide Playlist
Perforated Viscus: Examination
-
Emergency Medicine Bord Perforated Viscus.pdf
-
Download Lecture Overview
00:01 The classic history for perforated viscus is a sudden onset of severe abdominal pain. 00:07 You wanna ask about if the patient had any prior abdominal pains. 00:13 So do they have a history of having significant epigastric abdominal pain? Or diverticulitis’ pain, that’s classically in the left lower portion of the abdomen? So have they had any of that kind of pain recently? Have they ever had any kind of abdominal surgeries? Finding out whether or not patient has that surgery on their belly really can be helpful in trying to figure out what the underlying causes of the perforation or potentially to make you more concern that someone could get a perforation. 00:42 And then lastly, medications. 00:44 So is your patient on a PPI? That’s a proton pump inhibitor. 00:48 Are they on any GI related medications? Medications that would point you in the direction that they were having long term history of peptic ulcers. 00:58 Are they on an H2-blocker such as famotidine? Finding out what medications the patients are on can be very helpful. 01:06 Now, for patients with the perforated viscus, they’re gonna present with a variety of things. 01:12 So they may have fever, they may have tachycardia, tachypnea, hypotension, and possibly even sepsis or shock. 01:20 Generally, these patients are gonna be very sick appearing. 01:23 When you have a hole in your intestines it sets off a whole bunch of inflammatory markers and that’s what causes the patient to have all of these vital sign abnormalities. 01:33 To look very ill, to appear uncomfortable. 01:35 And then in the abdominal exam, so early on in the course you may have focal tenderness to the area of perforation. 01:43 For example, if someone developed a hole in their stomach, they may just be tender in the epigastric area. 01:49 Late in the course is when patients develop peritoneal signs. 01:53 These are patients who potentially maybe laying still in bed, they might not wanna move because potentially moving may make the pain worse. 02:01 They may have diffuse tenderness of their abdomen. 02:04 Their belly may be rigid, so when you go to touch their abdominal wall, it might feel hard almost like a board of wood. 02:12 And they may also have rebound and guarding. 02:15 So rebound tenderness is when you push down and then when you let go the patient experience more pain. 02:20 And then guarding is when patients kind—there’s both voluntary guarding which is when a patient tries to push your hand away when you push their belly and then involuntary guarding which is when the abdomen is more in that rigid state. 02:34 In the elderly and the immunocompromised patient may present atypically and may present diagnostic challenges. 02:40 The reasons that they may present atypically is that maybe a delayed in presentation. 02:45 So they might not necessarily feel that initial intense pain due to the fact that they may have altered pain proprioception, they may not feel it in the similar way to other people or possibly they have chronic abdominal pain and they feel as if it’s just the worsening of their chronic abdominal pain. 03:02 They may have pain for days rather than a patient who otherwise is younger, who will have pain for minutes or hours. 03:10 So they might present after a number of days. 03:12 And they may also have pain out of proportion to the physical exam. 03:16 So you might go ahead and feel their abdomen and their abdomen might be reasonably benign feeling. 03:22 So it might be soft, it might not have any clear or distinct tenderness and that’s what we call pain out of proportion to the physical exam. 03:30 They may be reporting a lot of pain but the physical exam might not be that exciting. 03:36 And then lastly, they may have unimpressive vital signs. 03:39 So they might have relatively normal looking vital signs. 03:42 Have a very low threshold for imaging these patients. 03:46 You definitely wanna make sure that you don’t miss this diagnosis and be sure to keep it on your differential. 03:52 So for elderly patients, immunocompromised patients, I generally will include diabetic patients in that immunocompromised subset because they’d might not necessarily perceive pain in the same way that a patient without diabetes would.
About the Lecture
The lecture Perforated Viscus: Examination by Sharon Bord, MD is from the course Abdominal and Genitourinary Emergencies. It contains the following chapters:
- Perforated Viscus Diagnosis
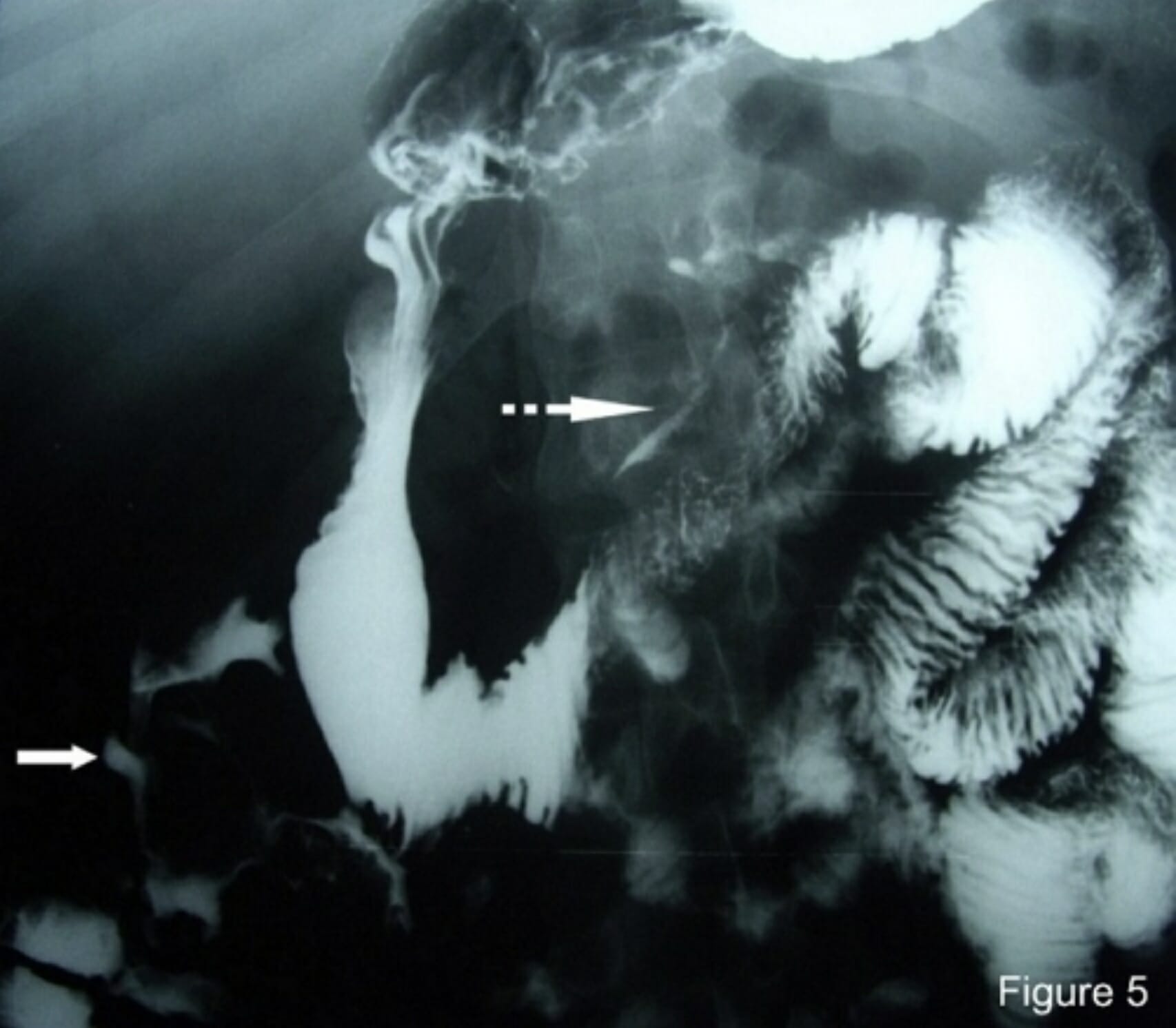
- Perforated Viscus Diagnosis: X-ray
- Perforated Viscus Diagnosis: CT Scan
- Perforated Viscus Diagnosis: Ultrasound
Included Quiz Questions
Which of the following statements regarding the presentation of viscus perforation in elderly and immunocompromised patients is NOT true?
- They typically present with hypotension at the onset of pain.
- They may show atypical signs of perforation.
- The progression of symptoms may be gradual.
- The pain may be out of proportion to physical examination findings.
- The onset of symptoms may take days to develop.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |