Playlist
Show Playlist
Hide Playlist
Peptic Ulcer Disease (PUD) with Case
-
Slides Gastroenterology 06 Stomach Disorders.pdf
-
Reference List Gastroenterology.pdf
-
Download Lecture Overview
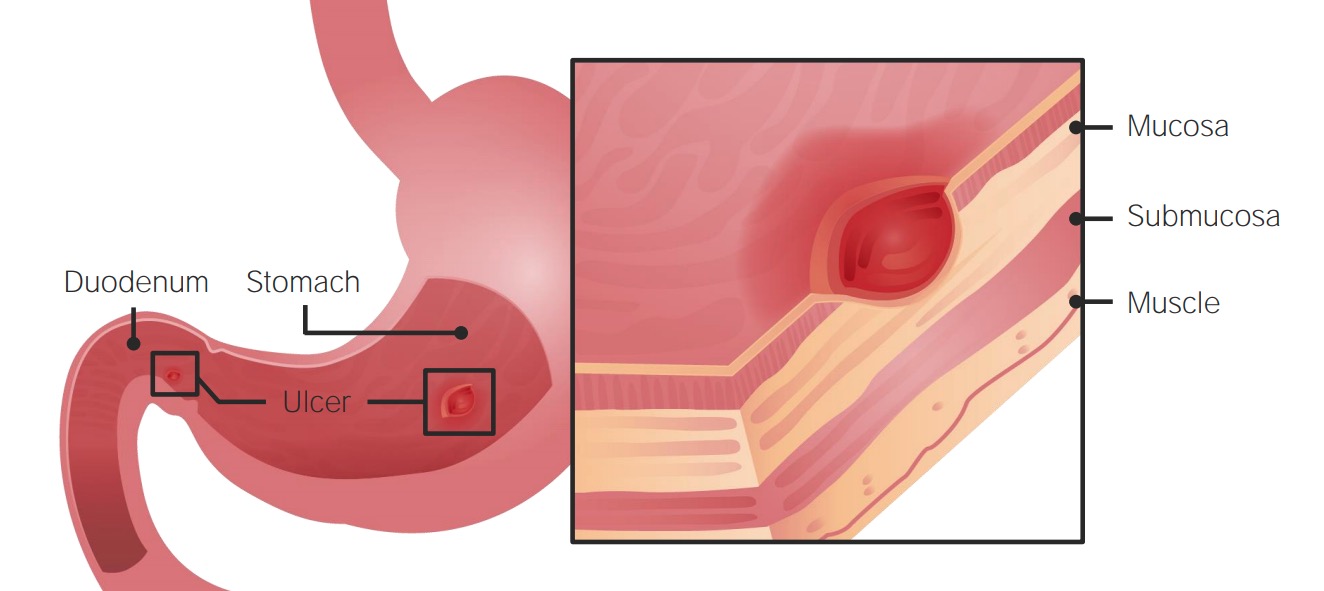
00:01 Hello. Today we'll be discussing disorders of the stomach. 00:05 As a brief outline of what we'll go through today, we'll first go through peptic ulcer disease. 00:11 We'll next go through gastritis. And lastly, we'll discuss gastric cancer. 00:17 So we'll begin with a case. 00:19 We have a 38-year-old woman seen in clinic complaining of epigastric burning and discomfort after eating for the last three months. 00:28 Her symptoms worsen at night. She takes ibuprofen several times a week for chronic headaches. 00:33 She has no family history of gastric or esophageal cancer. 00:37 She has no dysphagia, odynophagia, or unintentional weight loss. 00:42 Vitals are normal. On exam, she has mild tenderness in the epigastrium. And labs show a Hgb of 15. 00:50 What is the most likely diagnosis? So let's go through some key features of this case. 00:56 First, she has epigastric pain after eating and a history of chronic NSAID use. 01:02 Also she has no alarm features for malignancy which is reassuring. 01:08 So before we answer that question, let's talk a bit about peptic ulcer disease. 01:13 Peptic ulcer disease has several clinical features including epigastric pain and discomfort, nausea and vomiting, early satiety or feeling full quickly after eating, weight loss, and symptoms tend to worsen at night. 01:30 Patients may present with either gastric or duodenal ulcers. 01:36 And as we discussed earlier, they may have many of these clinical features. 01:40 Interestingly they often have pain that is in relation to eating; maybe either after or may improve with eating. 01:48 They may have early satiety, nausea, abdominal bloating or fullness. 01:53 So peptic ulcer disease can be complicated by many different conditions. 01:57 Four of the major complications include GI bleeding; when a ulcer can erode into blood vessel and cause bleeding. 02:05 The most dreaded complication is when the ulcer erodes completely through the wall of the stomach or the duodenum and then causes perforation into the abdomen. 02:17 The ulcer itself may also penetrate and completely through the bowel wall which can lead into an abscess or it can erode into adjacent structures such as blood vessels or the biliary system. 02:30 And if the ulcer forms in a particular area, it may also cause obstruction or a blockage. 02:36 So the diagnosis is done by upper endoscopy. Here on the right you can see two examples of peptic ulcers. 02:45 The first in panel A shows you a gastric ulcer with an exposed vessel which is at high risk for bleeding. 02:52 In panel B you can see a gastric ulcer without any evidence of active bleeding. 02:58 The treatment consists of identifying and correcting those underlying risk factors that lead to the ulcer in the first place. 03:07 And then you also give antacids or proton pump inhibitors or H2 blockers. 03:13 So what are the most common risk factors for developing peptic ulcer disease? In developed countries the most common risk factors are NSAID and aspirin use. 03:25 In developing countries on the other hand, infection with helicobacter pylori or H.pylori is still quite a common cause. 03:34 Beside those two risk factors, there's also tobacco and alcohol use which is quite prevalent, and other comorbid conditions that place people at risk for developing ulcers. 03:45 Some other things listed here include being on chronic anticoagulation medications and chronic steroid use. 03:52 Rarely you may also encounter patients who have an acid hypersecretory state like in Zollinger-Ellison syndrome. 04:02 So we spoke a bit about H.pylori and peptic ulcer disease. 04:07 It is a common cause of both peptic and duodenal ulcers especially in developing countries. 04:13 So if your patient comes from a developing country as their birthplace of origin, you should always make sure that you think about this new differential. 04:21 The diagnosis is made in several different ways. 04:25 The gold standard is by biopsy where you can examine and actually see the organisms on your pathology. 04:31 However that can be difficult to do. 04:33 So the most practical test is the H.pylori stool antigen test. 04:38 This has to be done off any antacids, proton pump inhibitors, and off all antibiotics. 04:45 You may also see a urea breath test. This is kind of an older fashioned test that we used to use. 04:52 It is not ideal any longer because of its poor sensitivity and specificity. 04:57 And lastly you may also encounter serology testing for the IgG antibody. 05:02 Note that this will only show you if the patient has been infected at any time in their life, it will not differentiate between an active infection or a prior infection. 05:13 Treatment is done with triple therapy. 05:17 So what that consist of is proton pump inhibitor, amoxicillin, and clarithromycin. 05:25 In addition, after you've treated the patient you should always make sure to repeat testing to confirm that you've eradicated the organism. 05:33 So as we mentioned, since H.pylori is quite prevalent in developing countries, you should always test for it in any patient who's under age 60 who has confirmed peptic ulcer disease. 05:47 So now let's return to our case. 05:52 We have a 38-year-old woman who is having some epigastric pain after eating, she does have some chronic NSAID use, luckily she has no alarm features for malignancy. 06:01 So the most likely diagnosis in this case is peptic ulcer disease. 06:07 Her underlying trigger is maybe her chronic NSAID use or H.pylori since she is under age 60. 06:13 So she should undergo endoscopy and have H.pylori stool antigen testing.
About the Lecture
The lecture Peptic Ulcer Disease (PUD) with Case by Kelley Chuang, MD is from the course Disorders of the Esophagus and the Stomach.
Included Quiz Questions
Which of the following is the most common risk factor for peptic ulcer disease in low-income countries?
- H. pylori infection
- NSAIDs
- Age
- Diet
- Smoking
Which of the following is the treatment of choice for peptic ulcer disease caused by H. pylori infection?
- PPI, amoxicillin, and clarithromycin
- H2 blockers
- Erythromycin
- PPI and erythromycin
- PPI and azithromycin
Which of the following is the gold standard diagnostic test for H. pylori?
- Biopsy
- H. pylori stool antigen
- Urea breath test
- Serology for IgG
- pH monitoring
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |