Playlist
Show Playlist
Hide Playlist
Pediatric Diarrhea: Pathology
-
Slides Gastroenteritis.pdf
-
Download Lecture Overview
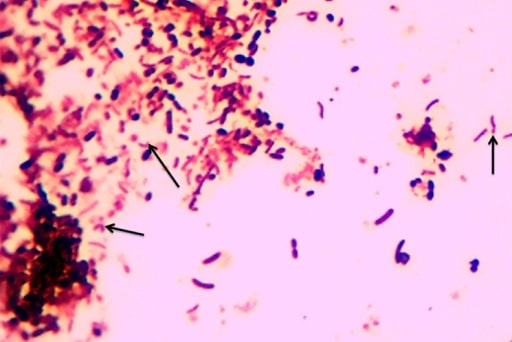
00:01 So what about a patient with diarrhea? The definition of diarrhea is more than 10 cc/kg per day of fluid loss through stools. 00:12 That might be on the test, I find it fairly useless in terms of a definition mostly because it's almost impossible to measure how many cc/kg per day of stool is coming out the child. 00:26 The leading cause of death worldwide in terms of morbidity and mortality in children is infections diarrhea. 00:36 Rota virus is a killer in the developing world. In the United States much less common because we have a medical system where children can come and get help if they are feeling dehydrated. 00:47 Generally, we will define diarrhea as acute or chronic. 00:53 The vast majority of diarrhea is acute and it is less than two weeks prior to presentation. 00:59 If a patient has more than two weeks of duration of diarrhea, we will call that chronic and we'll go through in a bit what the differences are in terms of etiologies of these various types of problems. 01:11 So let's go through types of diarrhea because this is important to understand and can sometimes show up on exams as well. 01:19 Secretory diarrhea is when intestinal epithelial cells are actively secreting water into the entero intestinal compartment and electrolytes are going along with it and through osmotic forces are causing water loss out into the stools. 01:40 The classic examples here is cholera toxin. 01:43 Osmotic diarrhea is much more common. 01:47 This is generally because of ingested solutes which are poorly absorbed causing water to get excreted into the intestinal compartment and then stooled out. 01:58 An example of this is a child who drinks too much juice, unfortunately we see this a lot. 02:05 We sometimes even see children who are failing to thrive because of excessive juice consumption. 02:10 So children who eat large amounts of osmotic material will start to stool out. 02:17 Motility disorders can occur occasionally happen which can decrease transit time. 02:24 Generally, this is through bacterial overgrowth. 02:28 This is not too common. Lastly, and especially in children with things like short gut syndrome, patients may have decreased surface area and thus an inability to actually absorb material creating what is effectively an osmotic diarrhea. 02:47 Short gut syndrome is really common in some of our NICU graduates especially those who have made it through an experience of surgical necrotizing enterocolitis. 02:58 So let's drill down into the causes of acute diarrhea. 03:02 By far and away the most common cause is infectious; and among infectious causes by far and away the most common is viral etiologies. 03:12 Viral illness used to be more in the spring with rota virus outbreaks, that's less common now because of the vaccination that we do so it now tends to be a little bit more in the summer and perhaps into the fall, as well, and of course in the winter we see some viral gastroenteritis as well. 03:30 Bacterial etiologies are not uncommon. 03:33 We see campylobacter, e. coli, salmonella, shigella, even yersinia and all of these can cause bloody stools. 03:43 In patients who've been exposed to antibiotics you may see C. difficile. 03:48 There may be systemic infections that are causing children to have acute diarrhea especially younger children who may just have that as a response to their general infection and parasites are possible although more common in developing countries. 04:03 In older children you may see that with food poisoning although with food poisoning which is ingestion of a preformed toxin rather than the actual bacterial causing the problem more commonly patients have vomiting as well. 04:17 There are of course noninfectious causes of acute diarrhea. 04:22 Antibiotic associated diarrhea is common with some antibiotics such as amoxicillin and clavulanic acid which may cause diarrhea in up to 40% of the patients who are taking the drug. 04:37 Hirschsprung toxic colitis is an unusual but important condition to know about. 04:43 I say noninfectious because the patient has an underlying problem with Hirschsprung disease, as you recall and there is another lecture on Hirschsprungs, patients will have a lack of ganglions in their rectal muscular tissue which causes them to be tonically constricted and get constipation. 05:04 However, if these patients get diarrhea and acute viral gastroenteritis or bacterial gastroenteritis, they can get very, very, sick because the diarrhea has a hard time getting out and bacteria can invade the intestinal wall and these patients can go into shock. 05:23 Neonates and we're seeing more of this than ever before are exposed to opium or opiates in-utero and as they come out diarrhea is a common result of withdrawal from opioid exposure. 05:38 Patients with congenital adrenal hyperplasia will often have diarrhea at birth. 05:44 In older children we again see the antibiotic associated diarrhea. 05:47 Appendicitis may cause diarrhea but it's more common that you have vomiting and abdominal pain. 05:52 Chronic diarrhea can also cause problems in children although it's much less rare than acute diarrhea. 05:58 Examples in both infants and older children include parasites and abscesses around the appendix as in an old perforated appendix that's healed up and there have some residual diarrhea left over. 06:12 Patients may have malabsorption problems and again this will cause more of that osmotic diarrhea so examples would be post infectious after their diarrhea children can rub off the lactase in their intestinal wall and be transit in lactose intolerant. 06:31 Patients can have food protein intolerance or allergy. 06:36 Children can get cystic fibrosis, celiac disease, toddler's diarrhea. 06:42 In older children we do see true lactose intolerance even though that's much rarer in the younger children and infants. 06:49 Adolescence who are trying to lose weight inappropriately may use Laxido. 06:55 Celiac disease and very, very, rarely secretory neoplasms can cause a secretory diarrhea. 07:03 Of course, auto inflammatory processes occur in younger children we see eosinophillic gastroenteritis and in older children we would add in the diet potential diagnosis of inflammatory bowel disease. 07:17 All of these diseases are where children would have prolonged areas of diarrhea going on for a long period of time and you start to drill down into some of these diagnoses in such a patient. 07:30 Additionally, you may see children with immunodeficiency. 07:34 These children will usually get other infections as well things like severe combined immune deficiency or HIV. 07:41 Again, adrenal insufficiency can cause this as can hyper or hypoparathyroidism. 07:47 So endocrinopathies can also cause chronic diarrhea. 07:51 Other problems can cause chronic diarrhea as well. 07:55 Rare things like lymphangiectasias in children, toxins exposure, and rarely congenital bowel disorders. 08:02 In older children you may see constipation causing what appears to be diarrhea when in fact it's not. 08:08 It's just encopresis, liquid stools squirting around the hard ball of stool that the child can no longer get out. 08:16 Irritable bowel syndrome starts to happen in older children and of course toxins can rarely cause this as well.
About the Lecture
The lecture Pediatric Diarrhea: Pathology by Brian Alverson, MD is from the course Pediatric Gastroenterology.
Included Quiz Questions
Which of the following is a cause of secretory diarrhea?
- Cholera
- Viral gastroenteritis
- Eosinophilic gastroenteritis
- Pancreatic insufficiency
- Bacterial overgrowth
A 6-year-old boy is brought to the clinic due to loose watery stool for 1 day. His parents tell the doctor that he has been drinking a lot of fruit juice recently. Which of the following is the most likely type of diarrhea this patient has?
- Osmotic diarrhea
- Secretory diarrhea
- Motility disorder
- Decreased absorptive surface area of the intestinal epithelium
- Physiologic diarrhea
A 4-year-old boy is brought to the clinic with loose watery stool since morning. He has no other signs and symptoms. Which of the following is the most likely cause of diarrhea in this age group?
- Viral gastroenteritis
- C. difficle
- Bacterial enteritis
- Parasites
- Systemic infection
A 10-year-old boy is brought to the clinic by his parents complaining of loose stool for the past 8 weeks. Which of the following would NOT be a likely cause of his diarrhea?
- Viral gastroenteritis
- Parasites
- Lactose intolerance
- Inflammatory bowel disease
- Celiac disease
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent lecture. Good overview of vomiting and diarrhoea with the definitions, etiologies and the most frequent diagnoses. Good explanation of the questions to ask to the parents.
A good introduction for an everyday problem in pediatric consults. And a good review for MDs.