Playlist
Show Playlist
Hide Playlist
Patient Introduction and Review of the Abdominal Anatomy
-
Slides Physical Exam Abdominal Pain Introduction.pdf
-
Reference List Physical Examination.pdf
-
Download Lecture Overview
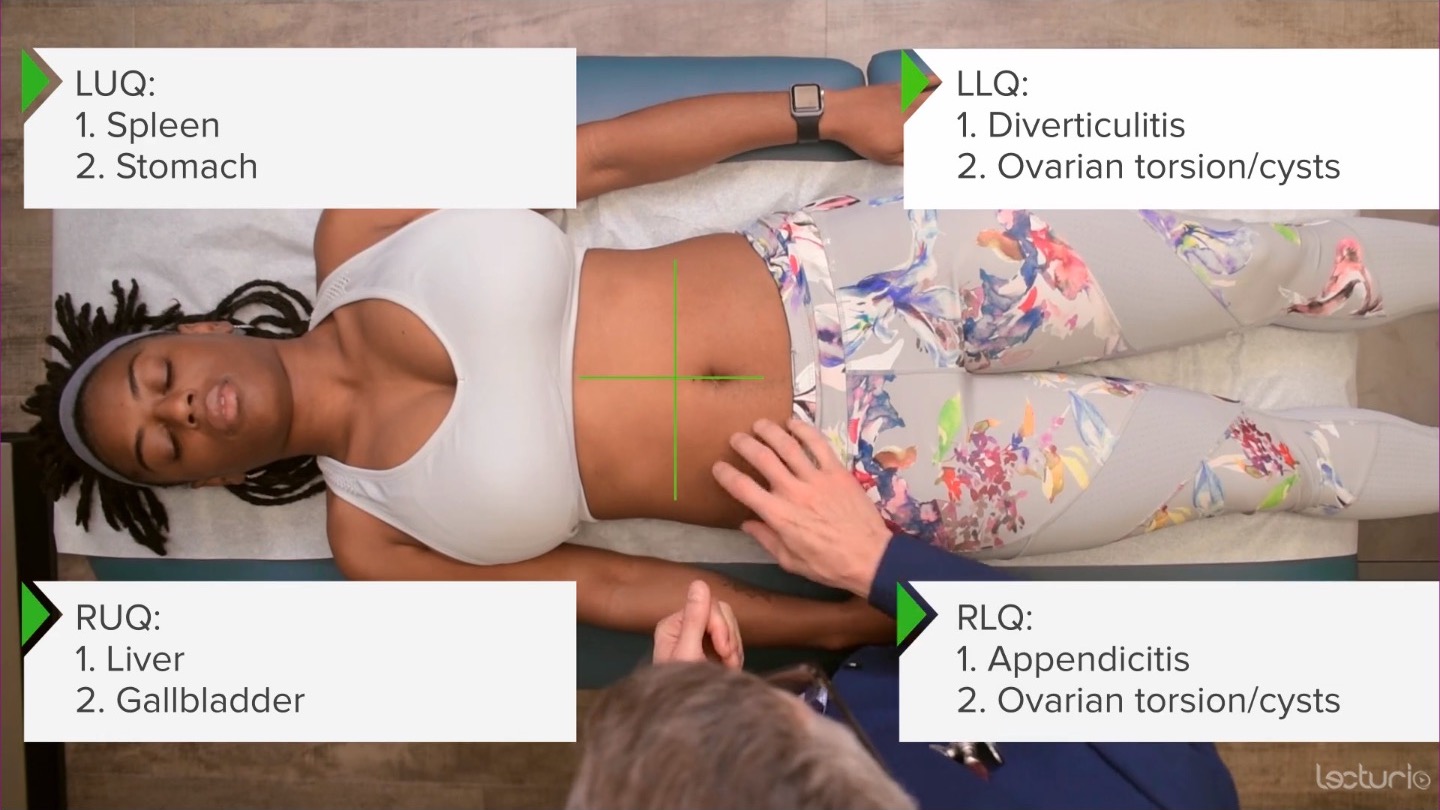
00:01 So let's talk about a case of abdominal pain. 00:05 So this is the 41-year-old woman who's presenting to her family physician with abdominal pain localized to her right upper quadrant. 00:12 She says, it's episodically occurring over the last two weeks, and it's gradually worsening. 00:17 So, when we're thinking about abdominal pain, it's important to first anchor ourselves to the different regions in the abdomen, and how they correlate with certain disease processes. 00:25 There's two primary systems for mapping out the abdomen. 00:29 The first is the abdominopelvic regions, which are depicted here. 00:33 And then the abdominopelvic quadrants, which is perhaps the more common language that we use. 00:41 Thinking about the right upper quadrant, which would also be the hypochondriac area, we're thinking about disease of the gallbladder like cholelithiasis, cholecystitis, and colangitis. 00:52 We're thinking potentially about liver: hepatitis, like alcohol related hepatitis. 00:57 Certainly stomach, while it's more midline, and epigastric, and location can have pain radiating to either side. 01:03 And then disease of the duodenum, like peptic ulcer disease can also manifest up in the right upper quadrant. 01:10 Moving over to the left upper quadrant, we're again thinking about peptic ulcer disease, particularly gastric ulcers, and much, much less commonly a splenic infarction can cause pain in that area as well. 01:22 Moving down to the right lower quadrant, certainly in younger patients we think about appendicitis so that can occur in older folks as well. 01:29 Disease of the reproductive tract in women, lots of things can cause pain regarding the ovaries, whether it's cysts that are rupturing or torsion itself and certainly in young sexually active women were worried about ectopic pregnancies as well. 01:44 And the left lower quadrant mirrors a lot of these same disease processes with the exception of diverticulitis, which can absolutely cause a subacute to acute pain in that area. 01:56 Another way of dividing up the abdomen is just into thirds with upper, middle, and lower abdominal pain. 02:02 Patients with upper abdominal pain, you always have to think about the thorax, and potentially the patient is actually having acute coronary syndrome, gastroesophageal reflux disease with that burning sensation that may start all the way up here at the base of the neck and can burn all the way down towards the epigastrium. 02:16 And of course, aortic dissection, while it usually radiates to the back, it can certainly cause anterior pain as well. 02:23 In terms of mid-abdominal pain, pancreatitis, again, usually radiating to the back, but nonetheless can cause burning abdominal pain and tenderness, anteriorly. 02:33 And then lower abdominal pain, anybody can have a urinary tract infection, prostatitis in men, and then pelvic inflammatory disease in women can be particularly severe and is an emergent condition. 02:47 I also want to highlight here something we often overlook, which is abdominal wall pain. 02:52 While a lot of things can cause pain, intra-abdominally it's important to recognize that the abdominal wall musculature itself can cause pain and often does after a period of vomiting. 03:03 Also, remember that there are cutaneous nerves that are diving or coming out adjacent to the rectus abdominis muscles and those nerves can get trapped and that can also cause very focal pain in the abdominal wall. 03:15 And we'll talk about during our exam lecture how to tease apart intra-abdominal versus abdominal wall pain. 03:23 And don't forget about shingles. 03:27 Lastly, it's important to think about is this a chronic, indolent diffuse pain or is it acute and diffuse? People with diffuse pain can't quite localize where their pain is coming from. 03:37 Classically irritable bowel syndrome and simply having constipation. 03:41 Inflammatory bowel disease is kind of a waxing and waning disease process that may have nonspecific, non-localizing pain. 03:48 And then acute painful conditions that can also present with diffuse pain would be a bowel obstruction, mesenteric ischemia, where there's pain that's out of proportion to the physical exam. 04:00 Bowel perforations can have very nonspecific findings because of peritonitis, where the entire peritoneum is inflamed. 04:08 So, looking back at the case we'd mentioned earlier, there's a lot of different things that this patient could have whether it's cholecystitis, choledocholithiasis, hepatitis, peptic ulcer disease, irritable bowel syndrome, or inflammatory bowel disease. 04:22 And we're really going to have to rely upon some really good physical exam skills to tease apart this differential diagnosis.
About the Lecture
The lecture Patient Introduction and Review of the Abdominal Anatomy by Stephen Holt, MD, MS is from the course Examination of the Abdominal Region.
Included Quiz Questions
What are the 4 abdominal quadrants called on examination?
- Right upper quadrant, left upper quadrant, right lower quadrant, and left lower quadrant
- Epigastric quadrant, umbilical quadrant, right lumbar quadrant, and left lumbar quadrant
- Right upper quadrant, left upper quadrant, epigastric quadrant, and pelvic quadrant
- Right hypochondriac quadrant, left hypochondriac quadrant, right iliac quadrant, and left iliac quadrant
- Epigastric quadrant, umbilical quadrant, hypogastric quadrant, and pelvic quadrant
What are 3 examples of common conditions associated with pain in the abdominal right upper quadrant (RUQ)?
- Cholecystitis, hepatitis, and peptic ulcer disease
- Diverticulitis, ovarian torsion, and splenic infarct
- Appendicitis, peptic ulcer disease, and diverticulitis
- Cholecystitis, prostatitis, and pelvic inflammatory disease
- Hepatitis, ovarian torsion, and appendicitis
Customer reviews
3,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
1 |
2 customer reviews without text
2 user review without text