Playlist
Show Playlist
Hide Playlist
Pathophysiology – Heart Failure
-
Slides 08 Cardiology Alpert.pdf
-
Reference List Cardiology.pdf
-
Download Lecture Overview
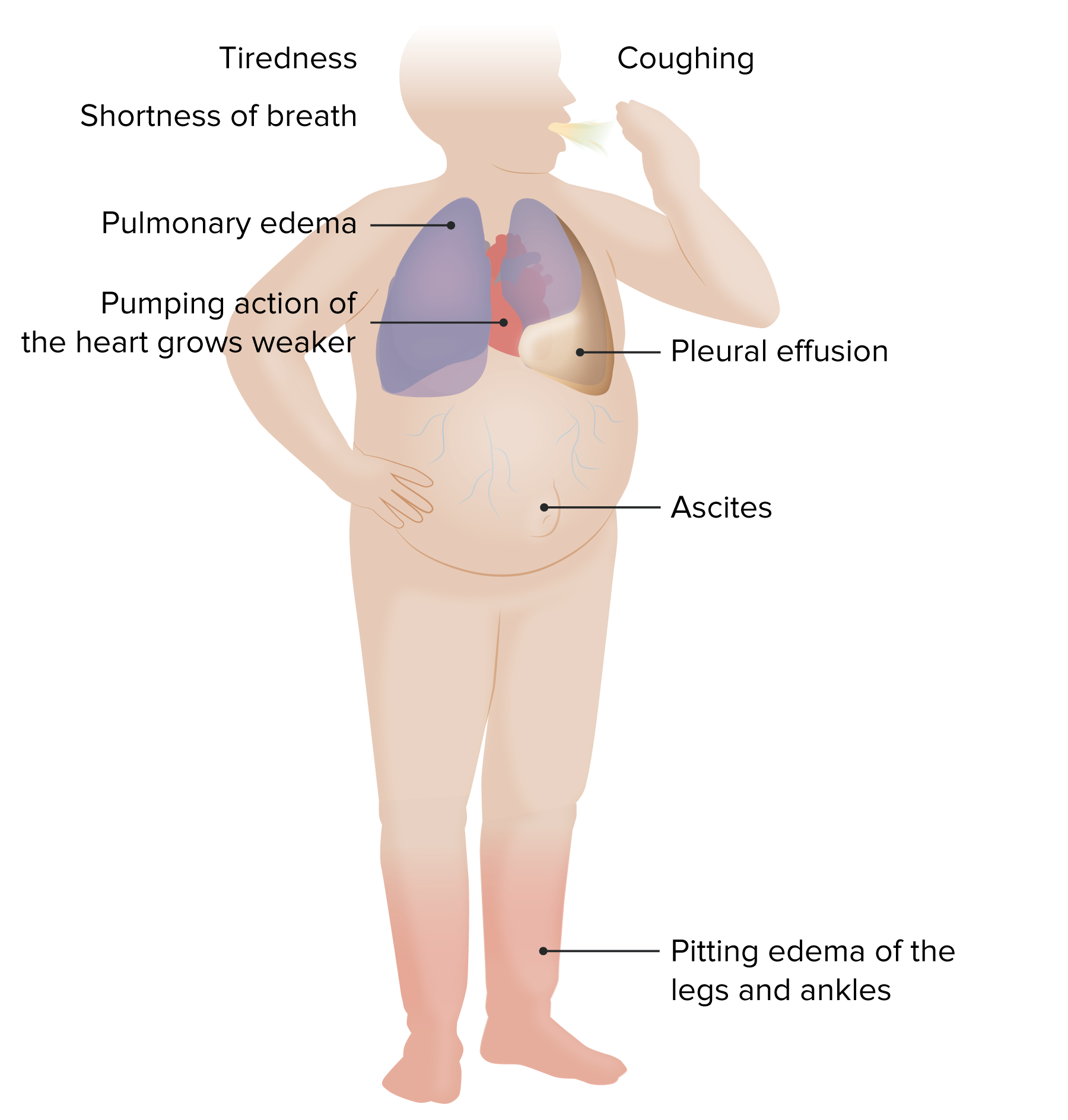
00:01 Now there are a number of compensatory mechanism that the body sets off when it sees heart failure. 00:09 Remember I mentioned them just a few moments ago. 00:12 What are the compensatory mechanisms? Well, let's think, why would the body compensate for decrease cardiac output. 00:19 For decrease pumping of the blood. 00:21 The reason the body compensates it's because it interprets heart failure as if there had been hemorrhage or blood loss or dehydration. 00:32 In other words, the reduced pumping ability the body interprets as, oh, there's a lack of blood from a hemorrhage or there's a lack of fluid in the circulation because of dehydration. 00:44 And it sets off a whole bunch of compensatory mechanisms aimed at holding on to fluid, water and salt. 00:53 Unfortunately, this is exactly the opposite of what we would want. 00:58 Because in holding on the fluid you actually create a setting where patients put some of that fluid into the tissues, both in the legs as edema or in the lungs as pulmonary edema. 01:11 So, the activation of these, neural-humoral system that is Central Nervous System, initiated activity to correct the heart failure situation actually makes the situation worse. 01:26 These systems work great if there's dehydration, you're caught in the desert without water. 01:30 They work great if there's a hemorrhage, you've been cut somewhere, or you're bleeding from an ulcer in your stomach, but they work, unfortunately, in a negative manner, in the patient with heart failure. 01:42 Let's just talk for a moment about why these compensatory mechanisms work. 01:47 They work because of something I mentioned before, Starling's Law, the so-called Rubber Band Law of the heart, the more you fill it, the more it contracts, so what the compensatory mechanisms were trying to do is to increase the filling of the heart so it will squeeze more. 02:02 As I've said, unfortunately, that leads to elevated pressures that back up in the system and result in edema. 02:08 But the, the Rubber Band Law of the Heart says that the force of contraction is related to how much you stretch the heart muscle cells and this increases contractility. 02:19 So you see why the body is trying to increase the pumping ability of the heart, and this works fine if it's a hemorrhage or dehydration, but it doesn't work well when the patient has heart failure. 02:32 So remember, stroke volume is the number of cubic centimeters that the heart puts out with each time it squeezes times heart rate, that's cardiac output. 02:44 So when we have a reduction in stroke volume because the heart has been injured, sometimes you'll even see the heart rate go up because the Central Nervous System says, oh, cardiac output is falling, we have to increase the heart rate. 02:58 We have to increase our ability to hold on to salt and water and increase the blood volume and use the Starling Law to increase the contractility of the heart. 03:06 Again, unfortunately, it's not the right setting for that and this leads to overfilling of the circulation, increased pressures in the circulation, and increased fluid getting out into the lungs and into the tissues. 03:23 So, the central factor in heart failure, of course, is depression of the heart muscle at least for systolic heart failure. 03:33 But also in diastolic heart failure, the heart is supposed to actively relax and there's also depression of that. 03:39 But the commonest form of heart failure as you've seen in the previous slide, was systolic, and it is usually because there's been some injury to the heart muscle, most commonly from ischemic or a coronary artery disease with heart attacks. 03:54 And, again, we've talked about the compensatory mechanisms, here are the compensatory mechanisms listed. 04:01 First of all, they're initiated by the Central Nervous System. 04:04 One of them is a signal that sends to the kidneys and the kidney actually does on its own, the kidney is the regulator of the blood pressure in the body. 04:14 It sees a drop in blood pressure, a drop in cardiac output and it releases compounds in something called the renin-angiotensin system which holds on to salt and water. 04:27 It's hormones that actively tell the kidney, hey, don't, don't pee out the sodium and water, hold on to it because the circulatory system needs some volume. 04:38 There are also hormones that are released from the Pituitary, so-called anti-diuretic hormone, which tells the kidney, hey, hold on to water. Don't let the water go out in the urine. 04:50 In addition, you also will have activation of the sympathetic nervous system which is part of the fight or flight system. 04:58 This sends adrenalin to the heart muscle to try and get it to contract more vigorously and it also clamps down a little bit on the periphery, in an attempt to shrink the volume that the heart has to pump into. 05:12 All of these compensatory mechanisms you can see, they work great if we're talking about dehydration or hemorrhage, but they work in the wrong direction when the patient already has a depressed left ventricle. 05:25 The other thing that happens is that the heart muscle remodels, it reconstructs itself if you will. 05:32 You can see in this diagram on the left, there's one form of remodeling, left ventricular hypertrophy, where the ventricle markedly thickens. 05:41 For example with aortic stenosis, as we talk about, with the patient in the last lecture. 05:45 On the other side, is the sort of thing you see in cardiomyopathy, the heart dilates, thickens a little bit but predominantly what it does is it dilates. 05:54 And you've all heard someone say, oh, so and so's in trouble. 05:57 They have a quote, "big heart" that's because the heart's dilated, that's often the final stage of heart failure when the heart has exhausted all of its other compensatory mechanisms to get the cardiac output up, then you start to see this dilatation of the left ventricle.
About the Lecture
The lecture Pathophysiology – Heart Failure by Joseph Alpert, MD is from the course Cardiac Diseases.
Included Quiz Questions
In heart failure, how do the kidneys try to compensate for the heart's decreased ability to pump blood?
- Increase fluid and salt retention
- Release anti-diuretic hormone
- Decrease sodium reabsorption in the loop of Henle
- Release epinephrine
- Increase myocardial contractility
According to Starling's law, what effect does increased end diastolic volume have within a healthy heart?
- Increased stroke volume
- Increased myocardial chronotropy
- Decreased stroke volume
- Increased pulmonary congestion
- Decreased end organ perfusion
Customer reviews
3,5 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
3 |
I love Dr Alpert. He is so neat in his explanations and so kind in his answers. He would be one of the best professors in the earth. Thank you so much Lecturio for bringing him to us!
This lecture couldn´t be clearer! I understood everything completely even though I'm not even a native english speaker
Many time i do not understand the pathology of heart failure, especially on compensatory mechanisms
clear logical excellent use of visual and examples to embed the information about types of compensatory mechanisms
3 user review without text