Playlist
Show Playlist
Hide Playlist
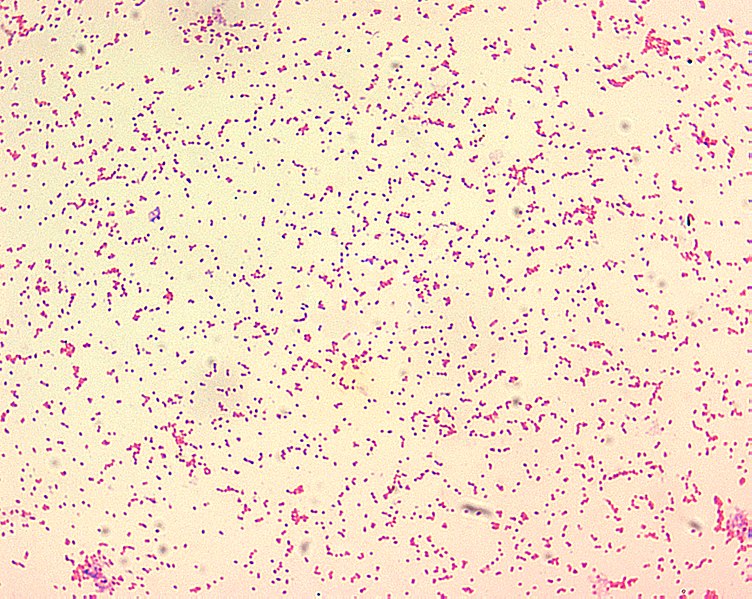
Pasteurella
-
Slides Pasteurella.pdf
-
Download Lecture Overview
00:01 Pasteurella, a bacteria. 00:03 Pasteurella are short, encapsulated, gram-negative rods such as you see on the gram-stain on the slide. 00:11 They have bipolar staining meaning that their staining is more dense, the ends of the organism. 00:17 Making them look almost like a barbell or a dumb bell. 00:20 The pasteurella are normal flora of domestic cats and dogs so even if those animals don't travel outside their flat, they will still most likely be colonized with the organism. 00:33 Therefore when those animals with their normal flora bite on humans, ingesting them or doing whatever to show their affection, then they can transmit that normal flora into, and past that skin barrier which is our best defense causing infection. 00:51 When human infection occurs it is most often caused by pasteurella multocida. 00:57 Here we see an active transmission of pasteurella multocida into the finger of a helpless victim in the upper image. 01:07 Yes, that is a normally pleasant cat that is transmitting its pasteurella after having it's ears groped, fondled or rubbed. 01:18 I'm not quite sure what, in any event that is where the actual transmission occurs. 01:22 Importantly, the transmission is penetrating the organism deep into the soft tissue of that victims finger because the sharp fangs of the cat are much longer than they are seen in dogs or other chewing type animals. 01:39 When infection develops it is preceded by swelling, followed by redness or cellulitis and then a bloody or purulent discharge coming out to the site of the inoculum of the wound. 01:51 If the infection is unrecognized and untreated, it has great potential to spread to nearby joints, infecting cartilage and bone and therefore causing infectious arthritis and also abscesses. 02:04 Cat bites especially because they are so deep and so difficult to treat effectively have great potential to keep on going because bone infections known as osteomyelitis. 02:16 Dog bites account for 90% of animal bites but cat bites of the more commonly infected. Because cat teeth deliver deep puncture wounds. 02:24 Nearly 50% of bites from a cat become infected versus just 7% for dogs. 02:30 In assessing the patient the first step is to perform a good physical exam, starting with a good global picture. 02:37 You then assess the patient's overall hemodynamic status. 02:40 Next, take special care to assess the structures near the wound, especially in cases with deep wounds on the head, neck, trunk or joints. 02:49 Fractures and ligament injuries are very common in severe dog bites. 02:54 Finally, you must always assess the neurovascular status distal to the wound and treating the wound. 02:59 Of course, the first step is to achieve hemostasis, typically by applying direct pressure. 03:04 Next, a thorough irrigation of the wound should be performed using local anesthetic as needed. 03:10 If an infection is suspected, obtain cultures prior to initiating antibiotics finally apply an appropriate dressing to the wound. 03:18 Keeping in mind that the vast majority of bite wounds should not be sutured, especially those deep penetrating cat bite wounds. 03:25 Occasionally, however, facial bites or other sensitive areas may need to be sutured to prevent scarring and to protect cosmetic outcome. 03:33 There are multiple considerations that impact our treatment choice. 03:37 Bite wound infections typically are polymicrobial, with an average number of cultured organisms actually being five or more. 03:45 Pasteurella is found in 75% of cat bites and 50% of dog bites. 03:50 Other bacteria to consider are capnocytophage which can cause a fatal sepsis in asplenic patients. 03:56 Bartonella commonly transmitted by cat scratches or fleas, such anaerobic bacteria as Bacteroides and fuser bacteria, and of course normal flora and human skin such as staph or strep, which has been inoculated into the wound. 04:11 The empiric treatment of choice is amoxicillin-clavulanate orally, but intravenous antibiotics can also be considered for more severe infections, especially those with rapidly progressive erythema, delayed wound healing or bite that is near an indwelling device. 04:27 Treatment and can be guided by results of cultures as needed. 04:31 The next thing to consider is a patient's immunization status for tetanus and to provide updated prophylaxis if needed. 04:38 Finally, one was always assess the patient's risk of rabies. 04:42 If the animal is wild or feral and or cannot be caught for testing. 04:47 Rabies prophylaxis should be given consisting of both rabies immunoglobulin and rabies vaccine. 04:53 So, pasteurella multocida coming from our animal friends in the home situation most often when they bite, the key to respond to such a bite is to wash out effectively. 05:06 Don't suture it. 05:07 Consider the use of ampicillin which should be quite effective. 05:11 But most importantly, be nice to our animal friends so they don't bite us in the first place.
About the Lecture
The lecture Pasteurella by Sean Elliott, MD is from the course Bacteria.
Included Quiz Questions
Which of the following features best describe Pasteurella species?
- Short, encapsulated, gram-negative rod
- Short, encapsulated, gram-positive rod
- Short, encapsulated, gram-negative coccus
- Short, unencapsulated, gram-negative rod
- Short, unencapsulated, gram-positive coccus
Which of the following conditions can be caused by Pasteurella multocida due to a cat bite?
- Osteomyelitis
- Osteoporosis
- Osteomalacia
- Osteosarcoma
- Osteogenesis imperfecta
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |