Playlist
Show Playlist
Hide Playlist
Pain Team – Pathophysiology of Pain
-
15 -The Pathophysiology of pain.pdf
-
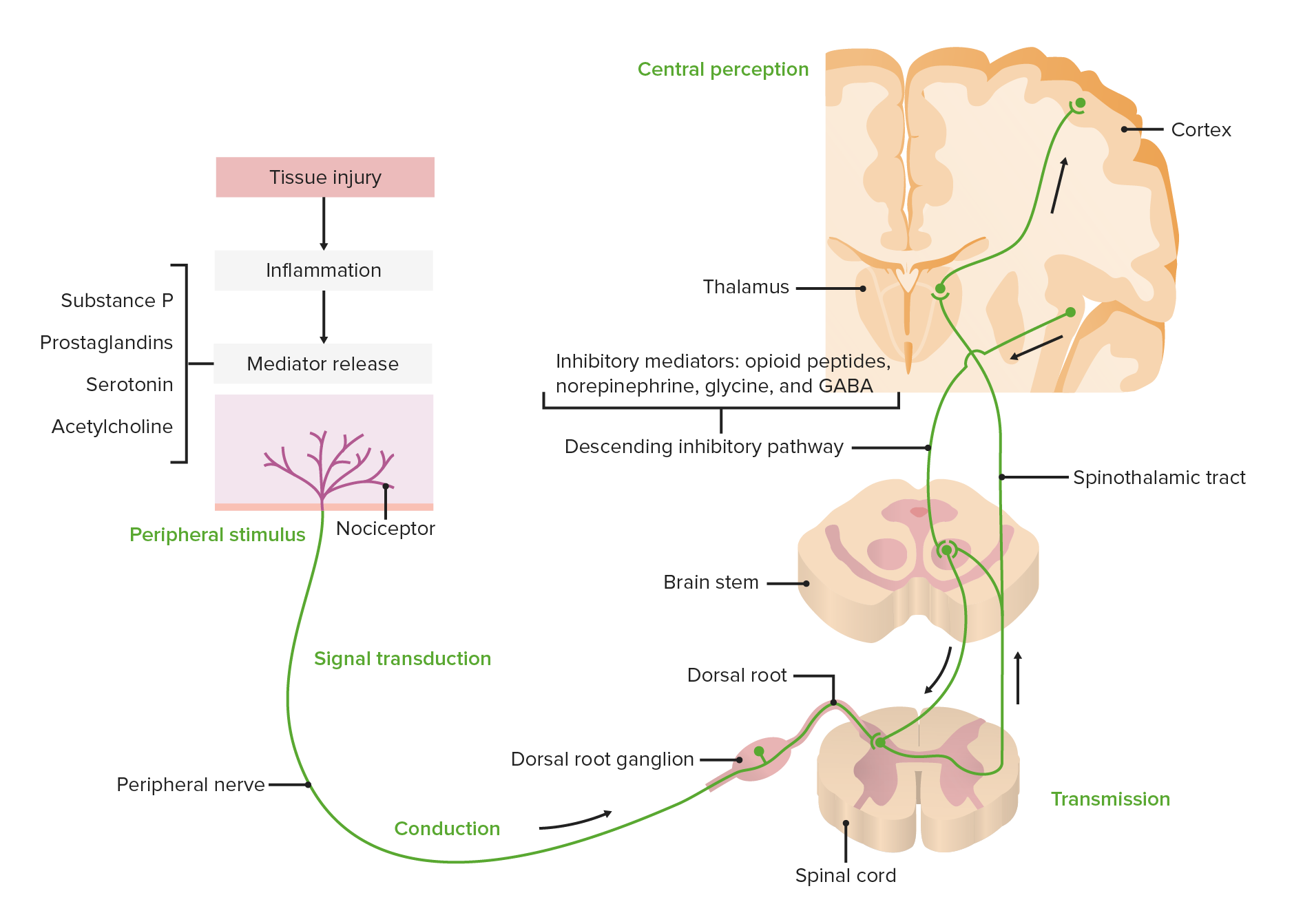
Download Lecture Overview
00:00 So the most important thing that I can convey to you in this lecture is the importance of the Pain Team. 00:08 The evidence on treatment of chronic pain has shown repeatedly that the only model of treatment that works consistently is a Multidisciplinary Pain Team approach to care. None of us individually, none of the disciplines by themselves are adequate to help people with chronic pain. 00:32 The lead member of that team is the patient himself or herself. And included in this should also be the patient's family, loved ones etc. Nurses (nurse clinicians), anesthesiologists, clinical pharmacologist, psychiatrist, physiatrist, physiotherapists, pharmacists, social workers, occupational therapist, radiologist, neurosurgeon, social workers, the family as I've already mentioned, and pastoral care are all part of the Pain Team. With obstetrical pain, it's the patient, the partner, the coach, the midwife, the obstetrician, and the anesthesiologist just as well. Acute pain, such that is caused by surgery or injury, can be managed by anesthesiology, but there should be access to the other professionals as well. And we've already covered some of acute pain, we'll cover a bit more again in this talk, but in honesty, most of the treatment of acute pain is over-the-counter medications such as acidanphetamine, paracetamol, or prescribed medication such as opioids. The treatment of chronic pain is much more complex. The incidence of chronic pain is unbelievably common and is largely ignored in our societies. It appears to be independent of race, culture, economic status. And it is said that about 30% of adults have chronic pain at any given time. And you'll recall the IASP definition we gave in an earlier lecture, that is continuing pain for 3 months, some people say 6 months, but an extended period of time in either case. 12% of people have severe pain. So at any given time, in each of our societies, 12% of the total country is suffering from severe pain. And 2% have such disabling pain, that they're essentially unable to function. Disabling pain is more common than cancer or heart disease, and more costly to the medical system or to the health care system than both cancer and heart disease combined. So pain neurotransmission. This is a simplified diagram just to give you some understanding of the process that the brain and the central nervous system go through in responding to pain and recognizing pain. 03:02 So, any kind of injury peripherally, or any kind of sensation peripherally, is picked up by nociceptive receptors. Nociceptive receptors are receptors that respond to, not so much injury, but to irritation, to almost anything that causes discomfort of any sort. The transmission is through the peripheral nerve to the dorsal horn of the spinal cord, and going through dorsal root ganglion on the way to the spinal cord. And then is transferred to the opposite side of the spinal cord and up through the nervous, central nervous system in the spinal cord to the cortex. And the cortex immediately responds to that pain by sending messages peripherally to subdue the pain. So in essence what's the brain is saying is, “OK. I know that there's pain out there, but let's turn off the excitement a little bit, let's reduce the acuity a little bit so we can deal with the whole issue.” So there's a constant modulation of pain that occurs at the brain level in the cortex, in the brainstem, in the spinal cord and peripherally. So initially the pain can be very severe, and you've probably noticed this, very severe when you first develop it, and then in a few minutes it's not quite as bad, it's still there, but it's not quite as bad. So Modulation, which is this process of moderating the pain, occurs at all levels and it's mediated by opioid peptides, we mentioned very briefly, enkephalins and other naturally occurring narcotics in our bodies. Norepinephrine, which is a neurotransmitter almost everywhere in the body, certainly in the central nervous system. Glycine and GABA. GABA is glutamic-aminobutyric acid and for many years it's been known to be involved in pain, both pain recognition and pain modulation. But drugs that work directly on GABA seem to have little effect on pain perception, and we'll get to that in a few minutes.
About the Lecture
The lecture Pain Team – Pathophysiology of Pain by Brian Warriner, MD, FRCPC is from the course Pathophysiology of Pain.
Included Quiz Questions
Which description applies to the pain team?
- Is the only evidence-based process for successfully treating chronic pain
- Is a collection of doctors who treat chronic pain
- Utilizes drugs only to treat chronic pain
- Is made up of basic scientists who study pain in animal models
- Should only include the patient and the pain physician
In managing chronic pain, who is the lead member of the pain team?
- Patient
- Anesthesiologist
- Pharmacist
- Nurse
- Psychiatrist
Which of the following structures is NOT involved in the nerve conduction of pain?
- Anterior horn cells
- Thalamus
- Hypothalamus
- Brainstem
- Dorsal root ganglia
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Style of explaining was amazing , simplifying subject, knock off pain concept in very unprecedented ways