Playlist
Show Playlist
Hide Playlist
Obstructive Sleep Apnea
-
Slides 10 RespiratoryDisorders RespiratoryAdvanced.pdf
-
Download Lecture Overview
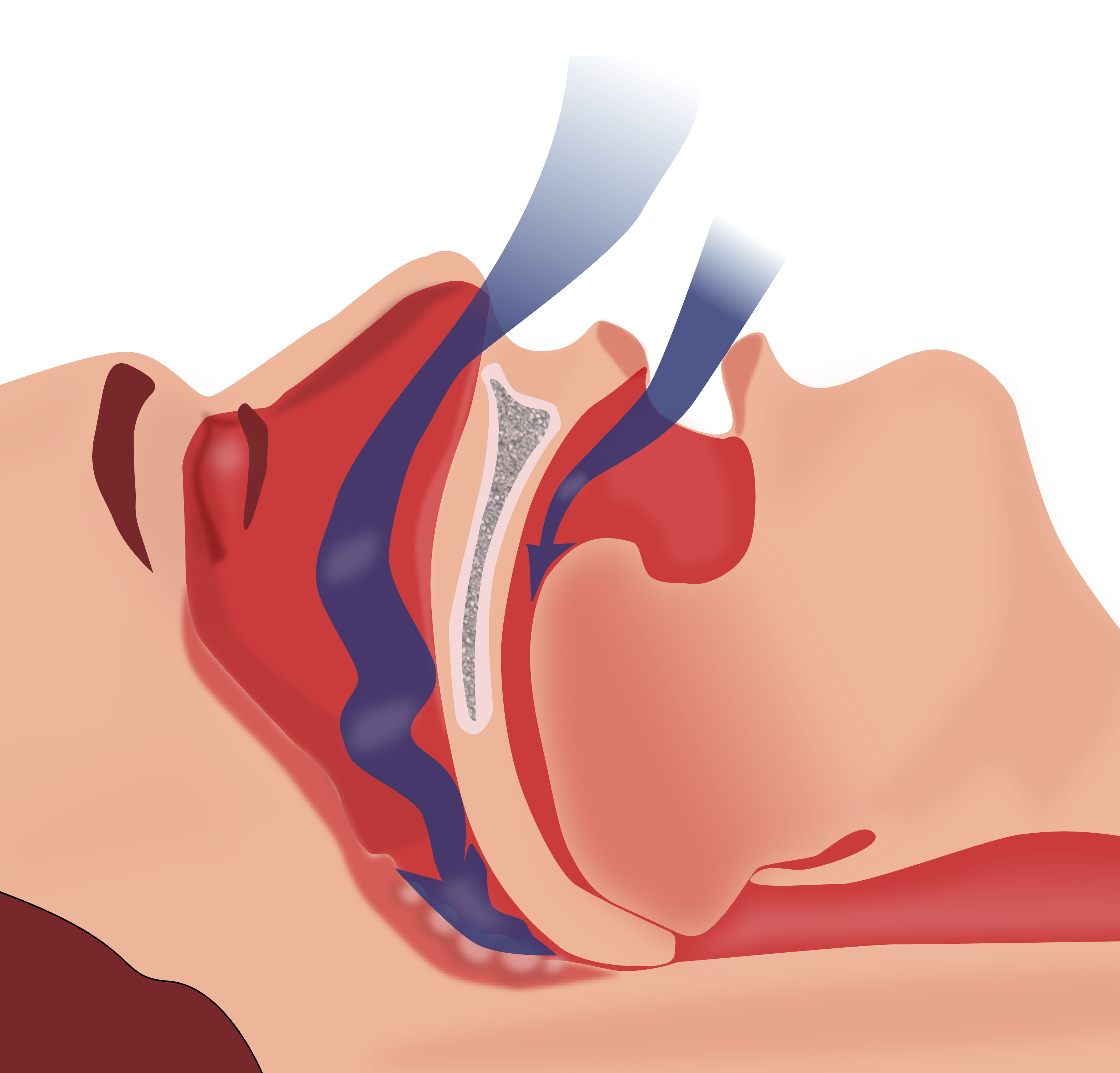
00:01 So moving on to obstructive sleep apnea, this is one of the commonest respiratory diseases, it's up there with asthma and COPD, not quite as common as those conditions but it is very common. Now, what happens in this is that you have some degree of upper airways obstruction when asleep and the reason for that is that the fat that accumulates, as you get older in life is deposited, in men specifically, around the neck, and that compresses the pharynx and makes it narrowed during sleep. Especially this is important during sleep because as you sleep your muscles relax and that allows the effects of this obstruction to be more obvious and the narrowed pharynx occurs as you sleep. And that generates the noise, one cause of snoring, but in addition, it generates obstruction to get in the air from the atmosphere down into the lungs and that leads to cyclical desaturations in your blood levels of oxygen. 01:04 It's a hypoventilation disorder that occurs repeatedly throughout the night. This leads to poor sleep quality not surprisingly, and as a consequence of that, patients tend to be very sleepy during the day and could fall asleep very easily during everyday tasks such as reading, watching television etc. driving a car in fact. And the physiological disturbance at night has bad consequences for the cardiovascular system, leading to hypertension precipitating ischemic heart disease and if it is very severe you might develop type II respiratory failure and pulmonary hypertension or cor pulmonale type situation. 01:43 Now this can affect about 1% of men in the Western world, it's much commoner in men than it is in women and the reason for that is not entirely clear but it seems to be about fat distribution. Most patients will be over 40 years of age and they'll be obese, they'll have a significant BMI and with that, their neck circumference will be large, over 43 cm. As I mentioned earlier, sedative drugs may cause a type II respiratory failure and hypoventilation worse, so drinking alcohol before you go to bed would make patients of OSA have more severe symptoms. Occasionally they may have an existing pathology of the upper airways which might make them more likely to get obstruction, a deviated septum, and the position of the jaw micrognathia, a small jaw or a jaw that projects backwards or forwards would make you more likely to get OSA and acromegaly disease, a growth hormone production very rarely is a predisposing factor for OSA. So the thing about obstructive sleep apnea is that actually it remains undiagnosed in lots of people. Many people snore, many of those will be snoring actually will be having a degree of OSA as well. The patient actually might complaint about daytime sleepiness and feeling un-refreshed after a night's sleep. 03:01 They might have to get up at night to pass water and they may have a poor concentration and memory due to this recurrent hypoxia occurring at night. The patient's spouse might say “I get scared because he stops breathing in the middle of the night, and then gives a big snort and starts breathing again”, that's a fairly common and that's an apneic episode where the problem with ventilation, actually the obstruction completely stops the breathing for a few seconds. There aren't really many signs in OSA, you can look at the back of the throat and there is a is a score that you can use to see whether the obstruction is quite likely to present, depending on what's visible at the back of the throat, but we don't need to know that in detail. What are the problems of OSA? Well, the serious consequences are car traffic accidents; a classic example would be, a heavy goods vehicle driver, 45-year-old man, drinks a bit before he goes to bed, might be weighing 20 stone, obstructive sleep apnea, chance of him having an accident is much higher than if he doesn't have OSA and that can have very serious consequences clearly. The OSA itself in severe cases can lead to pulmonary hypertension, cor pulmonale, and type II respiratory failure and there are these consequences on the cardiovascular system with hypertension, ischemic heart disease, dysrhythmias and there is a relationship between OSA and diabetes as well. 04:31 The biggest differential diagnosis is just simple snoring, snoring without obstructive sleep apnea. You can investigate these patients to identify whether it's just snoring or OSA, and the way to do that is by the sleep study, and I'll discuss that in a little bit more detail in a while. Other tests we may want to do, chest X ray, spirometry, blood tests, and these are all to look for associated diseases, for example co-existing COPD is quite common, hyperthyroidism is a cause of OSA etc. There's something called the Epworth sleepiness score, which is a method of marking how sleepy somebody is during the day and therefore whether they potentially have OSA, or not. Personally, I don't think it's particularly helpful, but it does identify patients who have significant sleep disturbance and therefore may need to have a sleep study. Now the sleep study, the simplest one is where you just record the overnight oxygen saturations when the patient is asleep and if you have obstructive sleep apnea, they fall repeatedly throughout the night. There are more complex sleep studies that can be done that measure chest wall movement, a sleep state using EEG, muscle movement using EMG, carbon dioxide levels etc. etc., but they're not usually required for very standard cases of obstructive sleep apnea. 05:54 This is a sleep study with moderately severe OSA and you can see the saw tooth pattern of recurrent hypo apneic episodes where the desaturation is occurring several times a minute, several times an hour out during the night. And you can define how severe OSA is by how may desaturations occurring throughout the night, with over 30 an hour meaning severe disease. How do we treat? Well very simply, if the patient can lose a lot of weight that will make a substantial difference, they need to stop drinking alcohol while having sedatives at night. You treat the hypothyroidism the acromegaly. If people have mild OSA, then there is a mandibular advancement device that pushes their mandible forward a little and that actually improves the obstruction at the back of the throat, and has substantial benefits in patients with milder disease. 06:46 Chronic disease needs treatment with continuous positive airways suppression. This is a small amount of airways pressure given as the patient breathes in, and that splints open the back of the pharynx, and is a very effective treatment for severe and moderate OSA. Surgery is not really effective unless there is a very specific problem of the upper airways that can be corrected by the surgical intervention. A very important point is that because of this risk of road traffic accidents, driving should be forbidden with patients with severe disease unless they have been effectively treated.
About the Lecture
The lecture Obstructive Sleep Apnea by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Other Respiratory Disorders.
Included Quiz Questions
Fat deposition in what area may lead to obstructive sleep apnea and cyclical desaturation?
- Around the neck
- Around the chest
- Around the nostrils
- Around the cheeks
- Around the mouth
Which of the following does NOT worsen upper airway obstruction in obstructive sleep apnea?
- Pneumonia
- BMI > 30
- Neck circumference > 43 cm
- Sedative drugs and alcohol
- Deviated septum
Which of the following is NOT a typical sign of uncomplicated obstructive sleep apnea?
- Prominent neck veins
- Snoring
- Nocturia
- Daytime somnolence
- Nocturnal apneic episodes
Which of the following is the treatment for severe obstructive sleep apnea?
- CPAP during sleep
- Mechanical ventilation
- Sleeping on a double pillow
- Use of a sedative
- Use of alcohol to induce sleep
What number of desaturations recorded during an overnight sleep study are necessary to classify a case of obstructive sleep apnea as mild?
- 5–14 desaturations/hour
- 15–30 desaturations/hour
- 31–45 desaturations/hour
- < 4 desaturations/hour
- > 45 desaturations/hour
Which of the following is NOT a common complication of sleep apnea?
- Asthma
- Cor pulmonale
- Car accidents
- Cardiac arrhythmia
- Ischemic heart disease
Which of the following is seen on a sleep study in a patient with sleep apnea?
- Repeated sawtooth dips in oxygen saturation
- Repeated sawtooth peaks in oxygenation
- No changes in oxygenation
- Alternating peaks and troughs in oxygenation
- Parts of the sleep study showing gaps
Customer reviews
4,0 of 5 stars
| 5 Stars |
|
0 |
| 4 Stars |
|
1 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
1 customer review without text
1 user review without text