Playlist
Show Playlist
Hide Playlist
The Neuromuscular Junction
-
IRheumatology II 01 Muscle Pathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
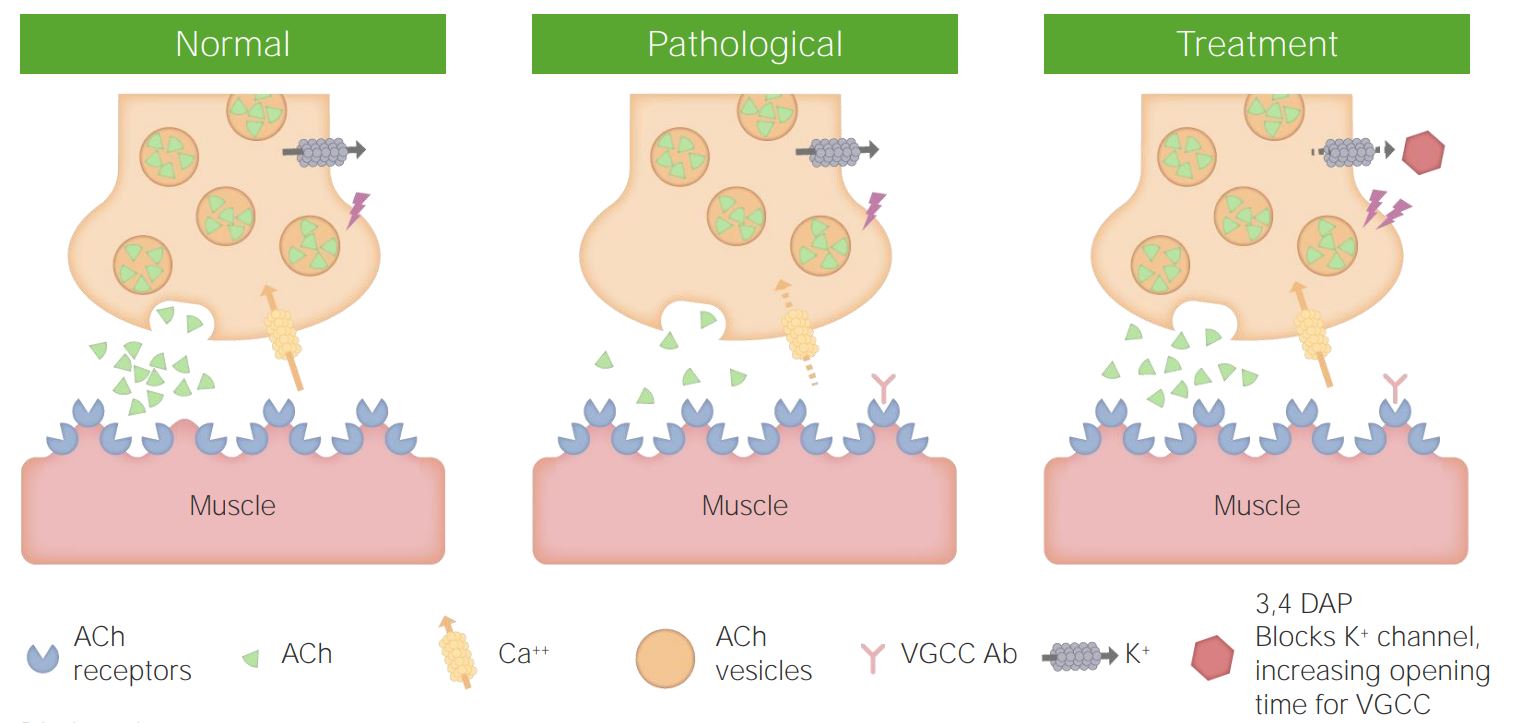
00:02 Here we’ll take a look at muscle pathology but the focus here will be the neuromuscular junction. 00:08 So please picture neuromuscular junction. 00:10 So we have a nicotinic receptor, and in your head, you should be thinking about the presynaptic terminal of the nerve which is then communicating with the motor end plate. In other words, the skeletal muscle. 00:22 In that presynaptic termina l, we have a vesicle and in that vesicle we have remind me—acetylcholine. 00:27 So what are things that you’re going to do to identify [Inaudible 00:03:39] doesn’t mean all receptors have been destroyed. 00:35 But what if there was a method that you could test and you activate those receptors? If you activate those receptors, then maybe perhaps you will find movement. 00:45 Keep that in mind. So the weakness has intensified by use. 00:49 That’s important because you’re going to be comparing myasthenia gravis with what? Lambert-Eaton myasthenia gravis syndrome. 00:56 So here, in myasthenia gravis, with use, it’s the patient that is feeling tired and recovers upon rest 3 in 100,000 would be the epidemiology. 01:07 The prevalence, as I’ve told you, would be much more in women because of its autoimmune nature—less than 40 years. 01:13 If it is a male, by chance, affected greater than 60. 01:18 Pathogenesis. You have the circulating autoantibodies that are then attacking the acetylcholine receptors, and surgically, there’s a possibility that the thymus may then be removed resulting in a thymic remnant. And by doing so, you are now actually improving the patient’s signs and symptoms. 01:38 So the thymus is [Inaudible 00:04:47] to type 2 hypersensitivity, autoantibody dependent [Inaudible 00:04:51] toxicity, try and go after those acetylcholine receptors. 01:50 Association—thymic hyperplasia and thymoma. 01:54 The pathology here [Inaudible 00:05:04] that the type 2 muscle fibers will be affected first. 02:01 What kind are these? Fast, white ATPase—lots of it. 02:09 For example, the ocular muscles. 02:13 There is absent simplification of the motor end plate, what does that mean? It means that the acetylcholine receptors are being knocked out, and depending as to the severity of the disease, you will still have residual [Inaudible 00:05:33] simplified. 02:29 Let’s go ahead and take a look at that neuromuscular junction. 02:33 On the left, is normal. 02:35 So what is that that you see here? The bulb which is coming down? The bulb that you see coming down or the flask, or whatever you want to call it, it’s the presynaptic terminal, and at the presynaptic terminal, you’ll then notice you have these vesicles. 02:49 Inside those synaptic vesicles, of course, is your acetylcholine. 02:54 What then allows for the vesicle to fuse with your presynaptic membrane? Help me out here. 03:00 Good. Voltage-gated calcium channels. 03:03 So the voltage-gated calcium channels where are they located? Not on the bottom structure—the bottom structure, what is that? That’s your motor end plate. What does that mean? That’s your skeletal muscle .So we’re trying to have movement—motor end plate. 03:19 So the voltage-gated calcium channels are on the the presynaptic terminal, on the flask, but then opens up the calcium channel. 03:29 Voltage coming from where? The axon up above. 03:34 So the action potential is going to come down the axon, come down through the presynaptic terminal and then open up that voltage-gated calcium channel. 03:45 The calcium, of course, rushes in allowing for fusion of the synaptic vesicle that you see there. 03:53 With the membrane, and out then comes whom? The acetylcholine. 03:59 That acetylcholine is then going to bind to the acetylcholine receptor and open up what kind of channel? [Inaudible 00:07:14] sodium channel. 04:08 The [Inaudible 00:07:16] acetylcholine and the receptor, of course, being on the skeletal muscle. 04:14 That’s normal on the left. 04:16 So what happens in myasthenia gravis syndrome on the right? You’ll notice autoantibodies with the thymic hyperplasia thymoma that is indicated and these are antibodies are then going to attack acetylcholine receptors, So that, all important. 04:36 Junction in communication between acetylcholine receptors, when it’s not happening, you’re not having a contraction. 04:43 What type of muscle fibers will be affect first? Type 2, your fast-twitch. I gave you the ocular muscles. 04:50 And what to test that you may want to provide or administer so you can find increase in strength? So what if you were able to give a short-acting cholinesterase inhibitor such as edrophonium in which you increased the concentration of acetylcholine in that cleft? It’s possible that the acetylcholine might then linger around and find a receptor that may actually function. 05:14 Then giving you for that brief moment in time, when you’re given that drug, an increase in strength, and by doing so, you’ve confirmed myasthenia gravis. Haven’t you?
About the Lecture
The lecture The Neuromuscular Junction by Carlo Raj, MD is from the course Muscle and Soft Tissue: Pathology. It contains the following chapters:
- The Neuromuscular Junction
- Structure of the Neuromuscular Junction
Included Quiz Questions
The neuromuscular junction is primarily involved in which of the following autoimmune diseases?
- Myasthenia gravis
- Parkinson disease
- Multiple sclerosis
- Alzheimer disease
- Systemic lupus erythematosus
Myasthenia gravis results from autoantibodies against which of the following receptors at the motor end plate?
- Acetylcholine
- Serotonin
- Dopamine
- Gamma aminobutyric acid
- Histamine
What type of receptor on the presynaptic terminal modulates the release of acetylcholine into the neuromuscular junction once the action potential has reached the nerve terminal?
- Voltage-gated calcium channels
- Voltage-gated sodium channels
- Voltage-gated potassium channels
- Gamma aminobutyric acid receptor channels
- Glycine receptor channels
Customer reviews
3,5 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
1 |
| 1 Star |
|
0 |
Hard to say what he is saying, even subtitles say that it is inaudible...
he is awesome; helps to connect the dots of concepts for me to make inferences rapidly