Playlist
Show Playlist
Hide Playlist
Neuromuscular Junction and Myasthenia Gravis
-
Slides 07 PolyneuropathyIndusIntellect Neuropathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
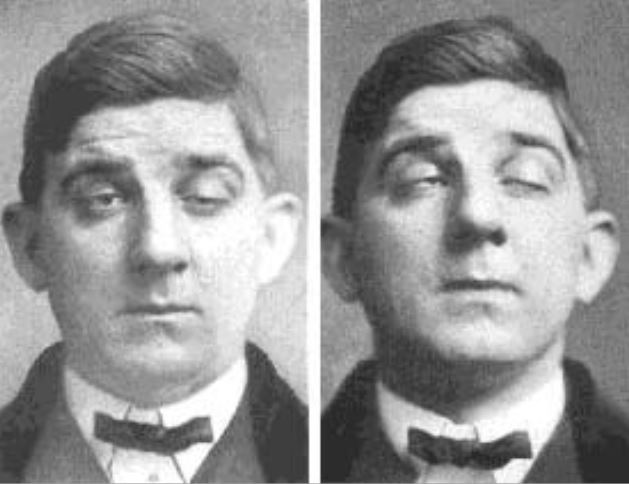
00:01 Once again, I bring this illustration to your attention cuz I want you to know where we are and what we’re dealing with. 00:08 So we’re doing neuromuscular diseases and we spend an awful lot of time with peripheral neuropathy and such and we talked about diseases of the anterior horn motor neuron diseases such as Amyotrophic lateral sclerosis. 00:21 With peripheral neuropathy we went through plexopathy, we went through mononeuropathy, mononeuritis multiplex and worked through polyneuropathies. 00:29 And then what we have left now is going to be neuromuscular junction diseases and then we’ll have our myopathies including our what's known as your muscular dystrophies, Duchenne and company. 00:41 At this junction, pun intended, is the neuromuscular junction - let’s begin. 00:47 So with neuromuscular junction what are we looking at? What if the problem is presynaptically and that’s where the disease was, so think about where you are first - neuromuscular junction, you’re gonna release what at the neuromuscular junction? Acetylcholine, what does it bind to? Your acetylcholine receptors aka nicotinic receptors these are ligand-gated this then opens up your sodium channel and in comes the sodium, right? But in order for you to release that acetylcholine what do you need to bring in presynaptically so you can release it? Ah, both is you got a calcium channel. 01:22 Presynaptic disease, Lamber-Eaton Myasthenic Syndrome - we have already talked about this as being possibly paraneoplastic with small lung cancer. 01:31 Botulism, what does that do? Well, if you’re injecting botulinum, right, why? Because her botox, right? That’s amazing to me but you’re trying to - I don’t know if the wrinkles by inhibiting the release of acetylcholine presynaptically and something called tick paralysis presynaptically. 01:56 Post-synaptically, the infamous Myasthenia Gravis, that’s where we’ll begin its Myasthenia Gravis. 02:03 Clinical features, what happens here? Well, most likely in an autoimmune disease, autoimmune disease automatically puts you into the gender or sex of females, right? In addition to that what else might you find here? The thymus in a 40 year old female, well, normally, should be non-existent but then they give you a chest x-ray or you’ve been shown a chest x-ray and then all of a sudden in this 40-year-old female, you find a thymic shadow, fascinating - a thymic shadow in a 40-year-old? Why in the world was there a thymoma to begin with or maybe because this female had Myasthenia Gravis and what happened, well, she had fatigable weakness. What kind of muscles? The proximal versus the distal and you have different types of muscles, don’t you? You have type 1 and type 2. 02:54 The fast twitch would be type 2 that you’ll have to memorize in your own special way but type 2 would be the fast muscle fiber, they require quite a bit of energy so therefore your - think about your eyelids, fast twitch. 03:05 So your patient is now complaining of, hey, doc. 03:09 I wake up in morning, hey, I feel great and I go to work and then around lunch time I’m having a hard time seeing and about the time 4 o’clock rolls out I am barely able to get out of my chair. 03:23 So prominent ocular involvement because the first type of muscle fibers to be affected would be fast twitch - ptosis and diplopia. 03:31 Continue. Pupils never get involve because why, this is neuromuscular junction is that clear? It has nothing to do with oculomotor parasympathetic. 03:40 Bulbar musculature frequently involved and deep tendon reflexes usually preserved. 03:46 Around 4 o’clock, why does the patient feels so incredibly tired because now the pathogenesis which we’ll talk about in a second, the acetylcholine receptors type II hypersensitivity had been destroyed. 03:59 If you don’t have these receptors, it might be difficult for you to move - where in the world are you supposed to have an action potential in the neuromuscular junction if your receptors are obliterated. 04:11 The pathophysio - what is it? Antibodies directed against the postsynaptic acetylcholine receptors. Where? On the muscle fiber, hence the oculomotor wasn’t affected, right? What was affected? Oh, the muscle, that’s right the type 2 muscle fibers. 04:30 Frequently associated with thymic hyperplasia, stop there, absorb that. 04:34 I told you about this female who had a thymic shadow at the age of 40, remember the thymus is responsible for educating our T cells and once the T cells are educated and then the self T cell undergo apoptosis then you -- we really - the thymus undergoes involution itself. 04:55 Next, the thymoma’s older onset which may need to be removed and that’s what I was referring to in your chest x-ray, will then reveal a thymic shadow. 05:05 Next, or what happens on your nerve conduction test? NCS, decremental response with low frequency repetitive stimulation. 05:14 Increased jitter on single fiber EMG. 05:18 So what do you think you might want to do in which you can increase the strength of the muscle? If the problem is that the acetylcholine receptors never worked, why not increase the concentration of acetylcholine? That sounds like a fantastic idea Doctor Raj, it is because if you do increase the concentration of acetylcholine, guess what, you might actually get a response where the muscle fiber might increase in strength. 05:43 You’re gonna use this for your diagnostic purposes and actually long-term management of your patient. 05:50 Are you having fun yet? Let’s do this. 05:52 Management of myasthenia gravis, what do you want to do? Increase the concentration of acetylcholine in the synaptic cleft, can you picture that? Are you there? A wonderful place to be, you inhibit the acetylcholinesterase, think about drugs such as pyridostigmine. Steroid, possibly. 06:12 And steroid-sparing agents, and so here, immunomodulators, right? Azathioprine, if necessary, methotrexate and company. 06:22 IVIG and plasmapheresis, especially if there's a crisis. 06:27 Remember, this is an autoimmune disease and so therefore attacking the acetylcholine receptors and if you get - if you start getting to a point where it's refractory and it’s really not responding, then you really not left much of a choice. 06:39 And then it is shown that by removing the thymus, this hyperplastic thymus or thymoma is that the patient’s symptoms might subside.
About the Lecture
The lecture Neuromuscular Junction and Myasthenia Gravis by Carlo Raj, MD is from the course Polyneuropathy. It contains the following chapters:
- Neuromuscular Junction
- Myasthenia Gravis
Included Quiz Questions
Which of the following neuromuscular diseases affects the postsynaptic region?
- Myasthenia gravis (MG)
- Lambert-Eaton myasthenic syndrome (LEMS)
- Botulism
- Tick paralysis
Which of the following is NOT involved in the pathology of myasthenia gravis?
- Pupils
- Eyelids
- Lateral rectus muscle
- Medial rectus muscle
- Bulbar musculature
A 45-year-old man presents to your office with fatigue for the past several weeks. He says he feels great during the early hours of the day but complains he is unable to drive back home from his office because of severe weakness. Which of the following statements is true about his likely condition?
- It affects proximal muscles more than distal muscles.
- It affects the presynaptic region.
- It always involves pupils.
- It affects distal muscles more than proximal muscles.
- It does not cause ptosis.
Which of the following findings in the chest X-ray of a patient with myasthenia gravis is most relevant in the management?
- Thymic shadow
- Fundus
- Cardiac silhouette
- Lung nodules
- Pleural cavity
Customer reviews
3,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
1 |
buena presentación, el expositor explica con mejores palabras y no lee solo las diapositivas
The subtitles do not go according to the doctor's explanation