Playlist
Show Playlist
Hide Playlist
Neurofibromatosis (NF) and Sturge Weber Syndrome
-
Slides TSandCNFandSWS Pediatrics .pdf
-
Download Lecture Overview
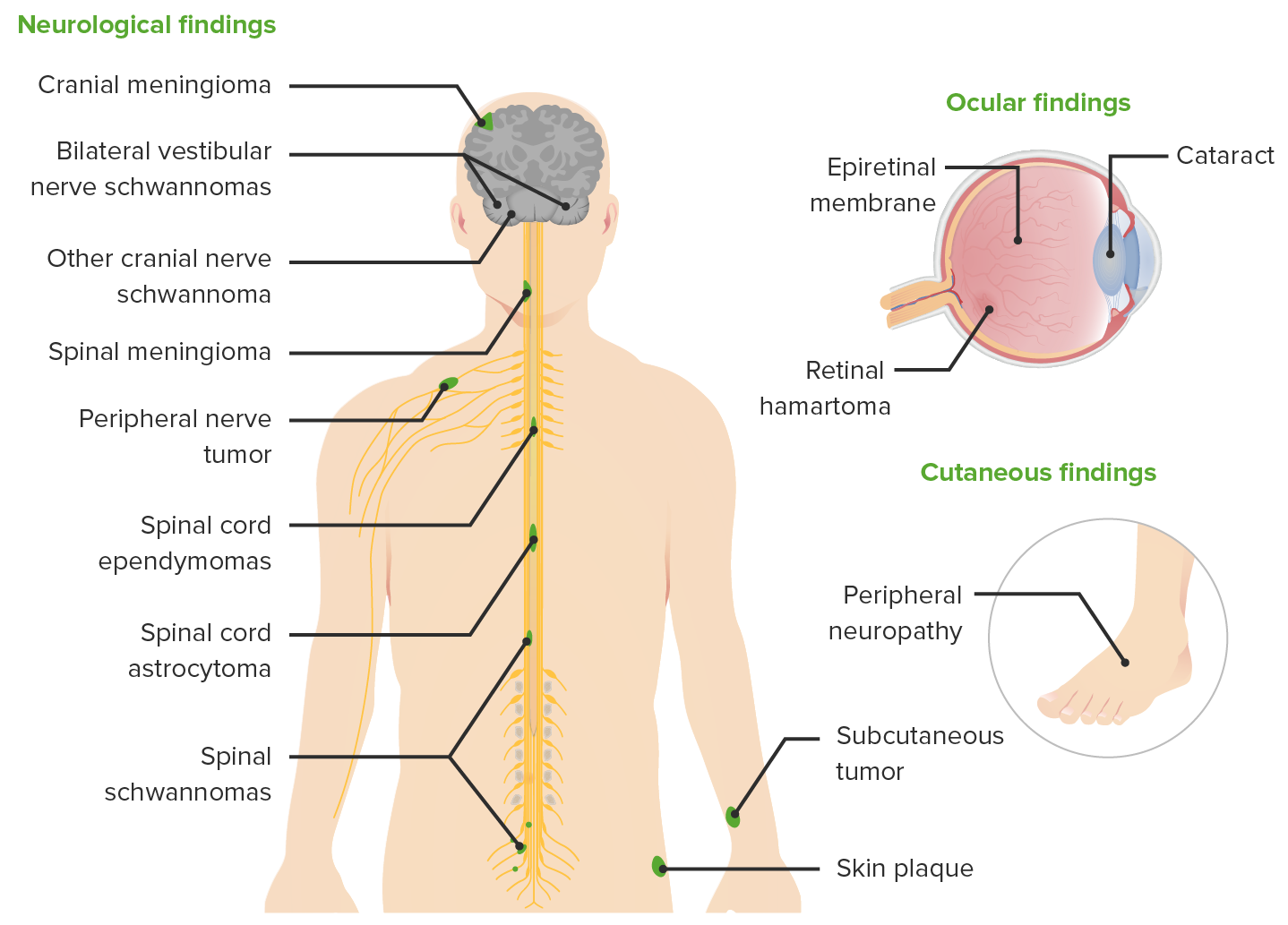
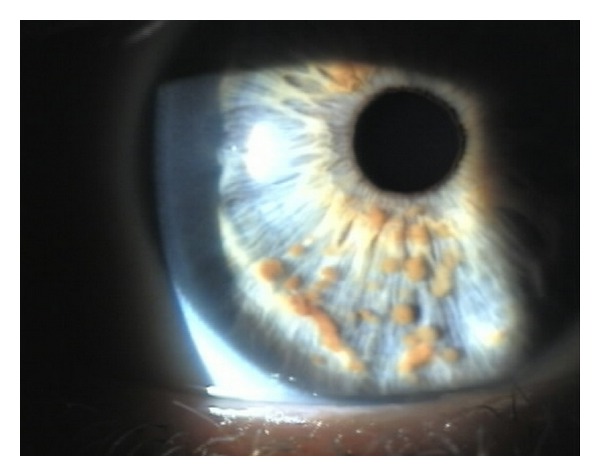
00:01 Let's switch to now to Neurofibromatosis. 00:05 Specifically neurofibromatosis comes in two types. Type I and Type II. 00:11 Type I is more common. 00:13 For type I neurofibromatosis, a patient has to have several findings to make the diagnosis. 00:20 First off, they only need two or more of the following major criteria This will be six cafe-au-lait spots larger than 5mm if prepubertal or larger than 15mm if post pubertal. 00:38 Keep in mind that these lesions are sort of like the opposite of an Ash leaf spot. 00:45 These are flat, macular but this time hyperpigmented lesions. 00:50 They look a bit like birthmarks, which sometimes people have. 00:55 So, this can be confusing. 00:57 Another criteria for which they need for two or more for the diagnosis is having two or more neurofibromas. 01:05 Neurofibromas are fleshy, rubbery, firm and non tender lesions that show up on the skin. 01:10 It's hard to miss them and you can see some here. 01:13 They may also have one plexiform neurofibroma and that will satifsy that criteria. 01:19 Another criteria we see commonly on children before neurofibromas show up is axillary freckling. 01:26 And you should keep an eye out for that for patients with cafe-au-lait spots. 01:30 Axillary freckling looks like little freckles in the armpits. 01:34 They may also show up in the inguinal area. 01:38 Another lesion that these patients may develop is the Optic glioma. 01:42 This is a lesion that is behind the eye that can cause a unilateral proptosis as you can see in this picture here. 01:50 One interesting finding, which is very very rare but is pointed out a lot sometimes on test questions is that these patients may have a pulsaltile exopthalmus because the retinal artery is pulsing with blood and the eye can actually be seen to bounce up and down or in and out as a result of that pulse. 02:13 Another finding which is consistent with the neurofibromatosis is having two or more Lisch nodules. 02:21 Lisch nodules are seen here in this patient. 02:24 These are little brown lesions that are found in the iris. They are a little bit easier to see in blue-eyed individuals for obvious reasons. 02:36 Another typical finding in neurofibromatosis is a distinctive bony lesion. 02:41 This usually happens on long bones or flat bones and they can show up on both xray or in this case on a bone scan. 02:50 Another criteria, which is actually one of the more common criteria to be satisfied is having a first degree relative with neurofibromatosis. 02:59 Remember, patients with neurofibromatosis can live long and fruitful lives and may have children themselves. 03:04 And their children are at an increased risk because it is inherited. 03:10 So, there are many other lesions that you can see in neurofibromatosis. 03:16 And you should probably read through them as a way of remembering and familiarizing yourself of the disease. 03:22 Some findings that one might see in this disease include sphenoid bone dysplasia. 03:29 Congenital hydrocephalus can be seen. 03:32 Patients may develop pseudoarthrosis. 03:36 Patients can develop Dermal neurofibromas as we've seen in this lecture. 03:43 Attention Deficit Hyperactivity Disorder is associated with neurofibromatosis. 03:49 As is speech and language delay and even Asperger's syndrome. 03:55 All of these are potential complications of neurofibromatosis type I. 04:01 Remember, neurofibromatosis comes in two types. Type I and Type II. 04:06 This two can be distinguished in many ways but a good way to remember it as a student when you are just getting started is Type I will frequently affect the eyes and type two frequently affects the ears. 04:17 The eye finding on type I is the optic glioma which we discussed earlier. 04:22 And in Type II they can have acoustic neuromas. 04:26 The criteria for type II are different from the criteria for type I and they bare looking at. 04:33 Let's switch gears now to Sturge Weber Syndrome. 04:37 Sturge Weber Syndrome is another neurocutaneous syndrome where patients will get classicaly a port-wine stain as it's pictured here on this patient usually in a trigeminal distribution over their face. 04:51 Sturge-Weber is usually present at birth as an agioma. 04:58 about 70% of patients will have an associated glaucoma at birth or soon after birth in the affected area around the eye. 05:08 So, these patients need to be seen by an opthalmologist. 05:12 Patients can have neurologic manifestations from inter cranial vascular anomalies associated with a skin lesion. 05:20 So, for example classically, they may have a seizure disorder, because of neurologic involvement, deep to that red lesion. 05:29 In Sturge Weber, management is largely supportive including anti-seizure medication And aspirin prophylaxis if that complex vascular area is prone to clot and eventually stroke. 05:44 For Cosmesis purposes, we can also provide laser therapy to these patients to allow them to look better as they function throughout their lives. 05:54 That is my summary briefly of the neurocutaneous syndromes. 05:58 Thanks for your attention.
About the Lecture
The lecture Neurofibromatosis (NF) and Sturge Weber Syndrome by Brian Alverson, MD is from the course Pediatric Neurology. It contains the following chapters:
- Neurofibromatosis
- Sturge Weber Syndrome
Included Quiz Questions
Which of the following is a sign of type 1 neurofibromatosis?
- Café-au-lait spots
- Adenomatous sebaceum
- Ash leaf spots
- Shagreen patch
- Periungual fibroma
Which of the following findings would be sufficient to satisfy one of the diagnostic criteria for type 1 neurofibromatosis?
- 1 plexiform neurofibroma
- 1 neurofibroma
- 10 or more Café-au-lait spots
- Acoustic neurofibroma greater than 2 cm
- Racemic neurofibroma more than 2
A patient with type 1 neurofibromatosis has small, brown-colored lesions in her iris. What are these lesions called?
- Lisch nodules
- Optic glioma
- Basal cell carcinoma of the eye
- Neurofibroma
- Hamartomas
Which among the following is NOT associated with type 1 Neurofibromatosis?
- Obsessive-compulsive disorder
- Sphenoid dysplasia
- Congenital hydrocephalus
- Asperger’s syndrome
- Pseudoarthrosis
Which statement is FALSE about Sturge-Weber syndrome?
- Sturge-Weber usually presents as a hamartoma at birth.
- The port-wine stain is present in the trigeminal distribution area on the face.
- Glaucoma is seen in about 70% of the patients.
- Sturge-Weber patients can present with seizures.
- Neurological manifestations are due to intracranial vascular anomaly.
How is the port wine stain in a patient with Sturge-Weber syndrome managed?
- Laser therapy
- Aspirin
- Carbamazepine
- Iodine wash
- Bevacizumab
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent lecture. It's good to have knowledge about these neurocutaneous syndrome.