Playlist
Show Playlist
Hide Playlist
Neurocognitive Disorders: Causes
-
Slides Dementia Psychiatry.pdf
-
Download Lecture Overview
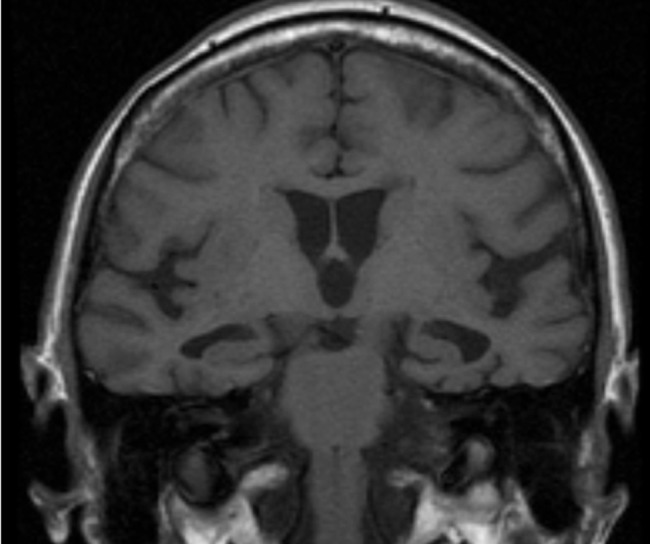
00:01 There are other cognitive disorders that are really important to know about. 00:04 So let's start with Alzheimer's disease. 00:06 The cause of this is low levels of acetylcholine. 00:11 The assessment is actually made postmortem. 00:15 When you're evaluating your actual patient. 00:18 What you're looking for is a progressive decline in their cognitive abilities. 00:23 However, the diagnosis cannot be definitively made until after they've passed, at which point you'll be able to see on the autopsy enlarged ventricles and senile plaques, neurofibrillary tangles and tau proteins, which are the hallmarks for Alzheimer's disease. 00:42 Although the treatment is mostly physical and emotional support, there are some medications that can boost up acetylcholine that can be useful, such as donepezil. 00:53 So these are things to consider in your management plan. 00:57 Vascular dementia is caused by the microvascular disease of the brain with small infarcts. The assessment can be made with an MRI. 01:08 And while the treatment is largely supportive in nature and encouraging good nutrition and exercise, you can also work with your patient to mitigate the risk factors for further cerebrovascular accidents. 01:21 So, for example, making sure their blood pressure and cholesterol are under very good control, possibly with medication management. 01:30 Another cognitive disorder to consider is Pick's disease. 01:35 This is caused by atrophy of the frontal temporal lobes, and it's often called frontal temporal lobe syndrome. 01:42 So here you want to make your assessment by looking at your patient for any acute personality changes. 01:50 It may be helpful to talk with their family members, who can give you some good information to tell you that this is an acute change and that the personality has in fact been affected. 02:01 Post mortem there can be pick bodies found or intra neuronal inclusion bodies. 02:08 The treatment here is very supportive again Again, sometimes cholinesterase inhibitors are useful, as are low dose benzodiazepines or antipsychotics. 02:18 For the patients who are extremely agitated and possibly suffering from some psychotic symptoms. Huntington's disease is an autosomal dominant genetic disorder, something important to note for your exam. 02:33 Autosomal dominant. 02:35 The onset is around 30 years old, up to 50, and it involves bizarre movements. 02:41 Basically chorea form type movements. 02:44 Often patients will be depressed and also have some psychotic symptoms. 02:48 The diagnosis can be confirmed through genetic testing and also MRI imaging can show caudate atrophy. 02:57 The treatment here is largely supportive. 02:59 Patients tend to have early mortality. 03:03 One thing you can offer to family members is possible genetic testing, to see if anybody's carrying that autosomal dominant gene. 03:11 Parkinson's disease is a prominent due to prominent neuronal loss of the substantia nigra. Basically, it leads to dopamine depletion. 03:22 And in your patient this will look like several things. 03:25 They may be Brady kinetic or have cogwheel rigidity, pill rolling tremor, a masked faces, a shuffling gait, and possibly dysarthria. 03:35 The treatment is multiple. 03:38 A lot of medications can be helpful here, including levodopa, carbidopa, amantadine, anticholinergic medications, dopamine agonists, and MAOIs. 03:49 Also, support and family education is extremely important. 03:54 Lewy body dementia is another type of dementia of unknown etiology. 04:00 It is characterized by the presence of Lewy bodies, which are abnormal aggregates containing alpha synuclein, a presynaptic protein with unknown function. 04:10 Lewy bodies are found predominantly in the cortex and the substantia nigra of the patients with the disease. 04:16 The presentation mimics that of Parkinson's dementia and includes cognitive decline, hallucinations, especially visual and the motor features of Parkinson mentioned above. 04:27 The difference between Parkinson's dementia is that in Lewy body dementia, signs and symptoms of dementia occurs before the Parkinsonian motor. 04:36 Symptoms. Multiple regimens have been used for the treatment of Lewy body dementia. 04:42 These include acetylcholinesterase inhibitors such as rivastigmine, donepezil, and galantamine. 04:50 Atypical antipsychotics such as quetiapine, aripiprazole, clozapine, memantine, and levodopa. Carbidopa. 05:02 Cjd is a prion disease and its rapidly progressive, and that's one of its key features. So patients will often progress to dementia within 6 to 12 months. 05:13 It's a very quick course. 05:15 Another key feature is that patients will present with myoclonus. 05:20 The treatment here is really supportive to the patient and their family while there's no cure. Normal pressure hydrocephalus is another cognitive disorder and this is caused by enlarged ventricles within this that lead to CSF pressure being greatly increased. 05:40 And the key signs of this are that your patient's going to look wet, wacky and wobbly. So they're going to be incontinent, they're going to have dementia and also some gait disturbance. 05:54 The way to treat this is actually fairly simple. 05:58 So you want to put in a shunt to relieve pressure in the CSF. 06:04 Now that concludes our discussion about dementia and cognitive disorders. 06:10 You have an understanding of some of the more common diseases and also how to rule out general medical conditions, medications and psychiatric disorders that can mimic dementia.
About the Lecture
The lecture Neurocognitive Disorders: Causes by Helen Farrell, MD is from the course Mild and Major Neurocognitive Disorders.
Included Quiz Questions
What are the neurochemical changes seen in Alzheimer’s disease?
- Decreased acetylcholine and norepinephrine
- Increased norepinephrine and acetylcholine
- Increased glutamate and norepinephrine
- Increased dopamine and glutamate
- Decreased dopamine and acetylcholine
Which of the following is NOT a post-mortem finding seen in Alzheimer's disease?
- Intraparenchymal cysts
- Enlarged ventricles
- Senile plaques
- Neurofibrillary tangles
- Tau proteins
Which of the following is an autosomal dominant disease that features dementia and caudate atrophy?
- Huntington’s disease
- Picks disease
- Parkinson’s disease
- Alzheimer’s disease
- Creutzfeldt-Jakob disease
Which of the following is NOT seen in normal pressure hydrocephalus?
- Myoclonus
- Incontinence
- Dementia
- Gait disturbance
- Enlarged ventricles
Which of the following is FALSE regarding Creutzfeldt-Jakob disease?
- Death typically occurs within 6 months.
- It is a prion disease.
- Patients worsen over a short period of time due to the rapidity of the disease.
- Myoclonus is an associated finding.
- There is no effective treatment for this condition.
What is the key MRI finding of Huntington’s disease?
- Atrophy of the caudate nucleus
- Atrophy of the frontotemporal lobes
- Prominent neuronal loss of substantia nigra
- Enlarged ventricles
- Small infarcts
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |