Playlist
Show Playlist
Hide Playlist
Neurally Mediated Syncope: Definition, Pathophysiology, and Classification
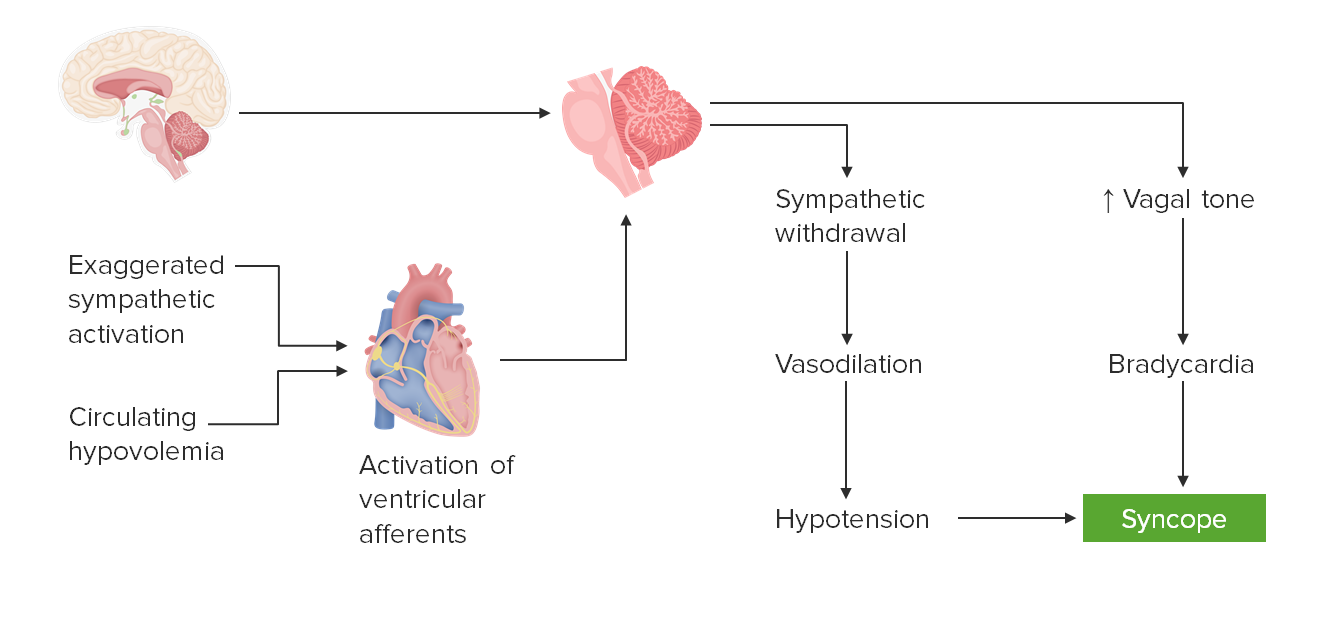
00:01 It's important to recognize that neurally mediated syncope comes from two things, the development of arterial vasodilation in the setting of relative or absolute bradycardia. 00:13 It's an important sentence, so let's break it down a little bit. 00:16 Typically, when the vessels dilate, the heart will speed up. 00:20 And that's a normal reflexive action in the body. 00:22 When the vessels dilate, blood flow goes down, blood pressure goes down, the heart recognizes this through the carotid bulb, and the heart rate will speed up or there's reflexive tachycardia. 00:35 Similarly, if the heart rate slows down, the blood vessels will recognize this through neural innervation and vasoconstrict and that will increase blood pressure in the setting of relative bradycardia. 00:49 With neurally mediated syncope, that process goes awry for some reason there is paradoxical arterial vasodilation and cardiac bradycardia which is always abnormal. 01:01 In the literature, this has been described through many words and is known as vasovagal reaction or vasovagal syncope, neurocardiogenic syncope emotional fainting, reflex of syncope. 01:14 I think the best categorization the best word to use is neurally mediated syncope, and we'll walk through what that is and how to think about it in the next few slides. 01:26 So what's the pathophysiology? How does neurally mediated syncope work? Well, it ends with a patient passing out or fainting and that's syncope. 01:36 One of the inputs one of the causes of that is hypotension. 01:40 There is relative hypotension too little blood in the vascular compartment. 01:45 At the same time, we see bradycardia again that paradoxical vasodilation, hypotension and bradycardia. 01:53 An abnormal paradoxical finding for some reason. 01:57 Hypotension occurs through vasodilation, which typically develops as a result of sympathetic withdrawal. 02:04 We know that the autonomic nervous system is composed of the sympathetic and parasympathetic nervous system. 02:10 The sympathetic nervous system speeds us up, it vasoconstricts it increases blood pressure, it's that fight or flight system, The parasympathetic is equal and opposite. 02:20 And those should be in balance. 02:22 In the setting of syncope, which is abnormal, the system is going awry. 02:27 And typically we see sympathetic withdrawal. 02:30 There's not that fight or flight response, and the blood vessels will vasodilate, causing hypotension. 02:37 At the same time, we often see increased parasympathetic tone. 02:41 So again, there's a paradoxical response going on. 02:44 There's no balance between the sympathetic and parasympathetic systems. 02:48 Sympathetic withdraw and parasympathetic activation. 02:52 The major nervous mediator of the parasympathetic system is the vagus nerve. 02:56 And so we see increased vagal tone, which slows the heart down and causes bradycardia. 03:02 So how is neurally mediated syncope working? What's happening is sympathetic withdrawal and increased basal tone. 03:09 There are a number of causes of that and we'll walk through those. 03:13 At the end of the day, the brainstem is the critical regulator. 03:17 It's what controls that autonomic nervous system. 03:20 And sometimes the brain is telling the nervous system to work arwy for some reason, and that's called central neurally mediated syncope. 03:29 And we'll walk through that. 03:31 Sometimes the input is coming from the heart from activation of ventricular afferents as a result of an exaggerated sympathetic activation or circulating hypovolemia. 03:42 So, neurally mediated syncope at the end result of syncope. 03:46 It is developed because of vasodilation in the setting of bradycardia, which is paradoxical. 03:52 Typically, that's from sympathetic withdrawal, and parasympathetic over activation. 03:56 And there are three inputs: the central nervous system, the brain, and exaggerated sympathetic activation, or circulating hypovolemia. 04:06 This is an important way to understand what's going on for patients presenting with neurally mediated syncope, and how to diagnose and treat those patients? So let's talk about those three inputs: the central, postural, and situational causes of neurally mediated syncope. 04:23 At the end of the day, there is sympathetic withdrawal, and an increased vagal tone or increased parasympathetic tone that results in hypotension, bradycardia, reduced blood flow to the brain, cerebral hypoperfusion and the patient passes out. 04:39 So what's going on in the body is the same, the input is a little different. 04:44 So let's start by talking about central syncope. 04:48 Central syncope is induced by a strong emotional stimulus. 04:51 You can think about a sudden scare, anxiety, or panic. 04:55 Like when someone scares you when they jump out from behind a wall. 04:59 The end result is activation of vagal tone and sympathetic withdrawal. 05:03 That's what's happening in all of the neurally mediated syncope. 05:07 Here, the driver for that starts within an exaggerated sympathetic activation. 05:13 That initial scare drives a sympathetic response and then overcompensation of the parasympathetic response. 05:22 So let's see what that looks like. 05:24 Again, with an initial scare, there's an exaggerated sympathetic activation. 05:29 And in the case of central syncope, there is not an equal compensation of parasympathetic tone, but an overcompensation of parasympathetic tone. 05:40 As a result, their sympathetic withdrawal relative sympathetic withdrawal, leading to vasodilation and hypotension. 05:46 An increase in vagal tone increase, or exaggerated overcompensating parasympathetic tone with bradycardia. 05:54 And the final common pathway and result is syncope. 05:58 So the first clinical scenario for neurally mediated syncope is central syncope, which is often induced by a strong emotional stimulus. 06:06 And the treatment then is to avoid that emotional stimulus. 06:12 Next, let's turn to the second situation. 06:14 Postural Syncope. 06:16 Postural syncope results from pooling of blood in the venous system. 06:21 There's reduced venous return of that blood to the heart. 06:25 There's a lack of reflexive tachycardia speeding of the heart, resulting in inability to compensate for this situation. 06:34 And some of the drivers of postural syncope include orthostasis, dehydration, antihypertensive medications, and autonomic neuropathy. 06:46 So let's see what's happening in this situation. 06:49 Well, the inciting event is circulating hypovolemia. 06:52 The most common situation is when a patient stands. 06:55 When we stand the blood rushes to our feet as a result of gravity. 07:00 The normal process is for the nerves around the vessels around the veins to recognize this and for there to be venoconstriction Vein constriction pushes blood back to the heart. 07:12 The heart recognizes this relative hypovolemia and speeds up, there's reflexive tachycardia. 07:19 And as a result, we maintain our blood pressure and maintain cerebral perfusion pressure. 07:26 In postural syncope, something goes awry with that situation. 07:29 And most commonly, this is as a result of an abnormality in nervous system tone around the blood vessels in the leg. 07:37 Those nerves don't sense the relative venodilation and venoconstrict. 07:43 There's not the relative reflex tachycardia to speed the heart rate up, and there's a reduction in cerebral perfusion pressure. 07:51 So we don't activate the ventricular afferents in the heart. 07:54 The brainstem doesn't recognize this problem with relative hypotension. 07:59 And in reflex tachycardia, there's sympathetic withdrawal, leading to vasodilation and hypotension. 08:05 There's increased parasympathetic tone, resulting in relative bradycardia. 08:10 And the final result is syncope. 08:12 This is the most common cause of neurally mediated syncope and that is orthostasis. 08:17 When the patient stands, the blood pressure drops. 08:21 The vascular tone doesn't increase to drive that blood back to the heart, and patients have decrease perfusion pressure, decrease blood flow to the brain. 08:30 The interventions then become to manage that orthostasis. 08:34 To take patients off or reduce antihypertensive medications to evaluate autonomic neuropathy, to avoid dehydration, and to counsel on lifestyle modifications for orthostasis. 08:49 And then the third clinical scenario for neurally mediated syncope is situational syncope. 08:55 This is syncope that is induced by micturition, defection, there can be post-tussive of syncope or valsalva induced syncope. 09:04 This specific stimulation is of sensory and visceral afferents and that's the driver of this phenomenon. 09:10 There's activation of strong parasympathetic tone without compensatory sympathetic counterbalance. 09:18 And we can see this in patients with autonomic neuropathy. 09:22 So what's going on there? Well, in this situation, we have an exaggerated parasympathetic activation with micturition or defecation or valsalva, the driver of those, the stimulus is strong parasympathetic activation without sympathetic counterbalance. 09:39 As a result, we see relative sympathetic withdrawal, vasodilation, and hypotension. 09:45 We see an exaggerated parasympathetic response or increased vagal tone and bradycardia, and the final result is syncope. 09:53 And so, for the situational syncope, we counsel patients to avoid situations that may induce the syncopal event.
About the Lecture
The lecture Neurally Mediated Syncope: Definition, Pathophysiology, and Classification by Roy Strowd, MD is from the course Vertigo, Dizziness, and Disorders of Balance.
Included Quiz Questions
Which statement is the most accurate when broadly discussing neurally mediated syncope?
- It presents with arterial vasodilation in the setting of bradycardia.
- It presents with arterial vasoconstriction in the setting of tachycardia.
- It presents with arterial vasodilation in the setting of tachycardia.
- It presents with arterial vasoconstriction in the setting of bradycardia.
- It presents as arterial vasodilation and is unrelated to the heart rate.
Which statement is the most accurate with respect to central syncope?
- Treatment options include avoiding emotional stimuli.
- There are no pharmacological treatments.
- The parasympathetic system is insufficiently activated.
- The sympathetic system is insufficiently activated.
- It is caused by the pooling of venous blood.
Which statement is the most accurate with respect to postural syncope?
- Postural syncope can be precipitated by antihypertensive drugs.
- Postural syncope ultimately results in increased cerebral perfusion.
- Postural syncope is related to a rapid increase in the venous blood return to the heart.
- Postural syncope is common in patients who are sitting upright for an extended period.
- Postural syncope is caused by the overactivation of reflex tachycardia.
Which statement is the most accurate with respect to situational syncope?
- It can be induced by an episode of severe coughing.
- The initial cause is due to the decreased activation of visceral afferents.
- There is underactivation of the vagal parasympathetic system.
- It is usually related to emotionally charged events.
- It is directly related to hydration levels.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Great lecture. I think the concepts were well explained in a concise way.