Playlist
Show Playlist
Hide Playlist
Nephrolithiasis: Clinical Evaluation
-
Slides Nephrolithiasi.pdf
-
Reference List Nephrology.pdf
-
Download Lecture Overview
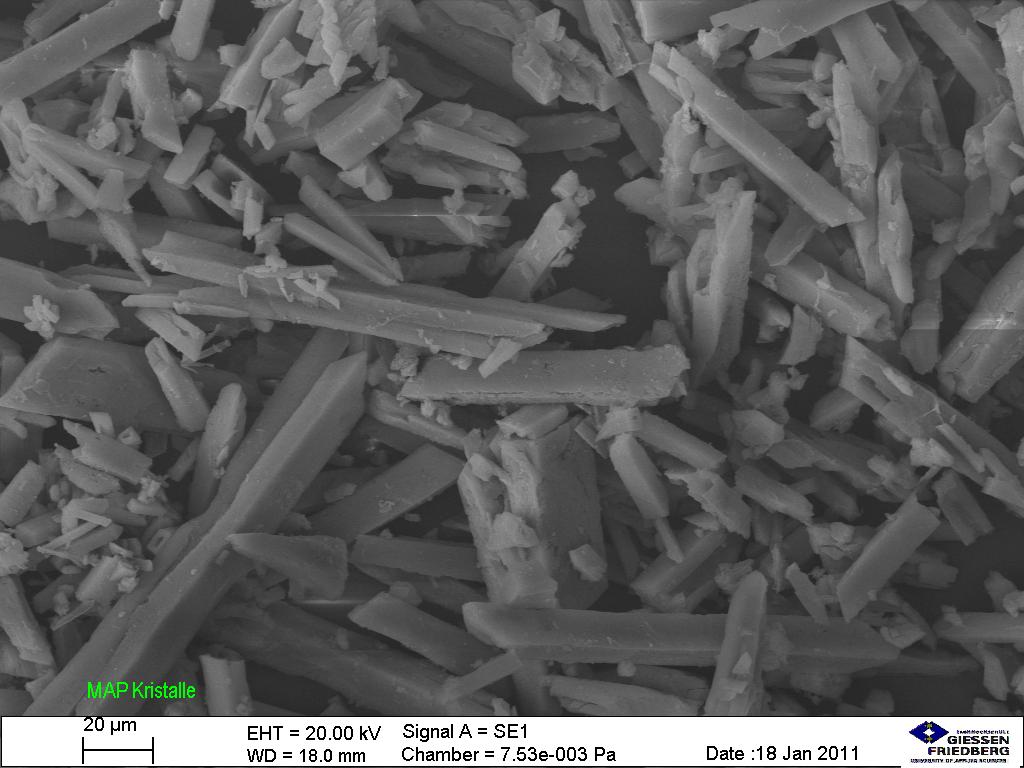
00:01 What do we do when we want to clinically evaluate that patient and when do we do it? The first symptomatic kidney stone does warrant a basic evaluation. 00:11 So there's a number of things that we want to do during this basic evaluation, number one: we want a good stone history. 00:18 That means we want to know the number of stones people have had in the past, the frequency with which they've had them, the age of first onset - were they younger, were they older? the size of the stone and the type of the stone if they know what that is, and the need perhaps for urological intervention meaning that a urologist would need to come in and break that stone up or retrieve the stone, or whether or not they've had stones in association with UTI. 00:43 Medical history is also important. 00:45 Maybe that patient has an underlying condition that would predispose them to a stone, for example there are conditions that cause hypercalcemia for calcium-based stones or hypercalciuria, that means too much calcium in the urine These are things like hyperparathyroidism, sarcoidosis or malignancies. 01:04 We'd want to know if our patient has a history of gout because that would be very critical in determining whether or not the patient has uric acid stones. 01:13 Medications will also be very important. 01:16 Calcium-based stones are often associated with something like loop diuretics. 01:20 Remember these work at that thick ascending limb of the loop of Henle and that's where we have paracellular calcium absorption when we're using a loop diuretic that will increase calciuria or calcium in the urine and potentially can increase stone precipitation. 01:35 High doses of vitamin D, remember the action of vitamin D? it causes intestinal absorption of calcium. 01:40 If our patients are on super-therapeutic doses, they can be absorbing too much calcium. 01:46 Also patients taking exorbitant calcium supplements or antacids can also be at risk and then medications like topiramate which is an anti-epileptic drug. 01:56 Uric acid-associated stones are associated with salicylate, probenecid, melamine which we don't see but has been associated with contaminated infant formula. 02:08 Medications that precipitate into stones include things like triamterene. 02:12 Remember that's that potassium-sparing diuretic, oftentimes used with hydrochlorothiazide. 02:18 Acyclovir and these are usually parenteral or intravenous high doses and then our Proteus inhibitors for ART and our HIV population which include indinavir and nelfinavir. 02:31 Occupation is also very important. 02:34 If our patients have vigorous physical activity without adequate hydration, for example working outside in high temperatures or in occupation that requires minimizing bathroom breaks and I think we as medical professionals are very guilty of that particular people who are working in the OR. 02:51 They oftentimes limit the amount that they're drinking so they don't have to interrupt their cases. 02:57 Diet intake is also important. 03:00 Patients who are taking high sodium diets, high animal protein or oxalate, purines in sugar-sweetened drinks all predispose to stone formation. 03:10 If you look at our table here, for patients who make oxalate stones, there's actually quite a few different foods that can predispose to these stones and some of our favorites might be in here like black tea. 03:21 That's what our patient was drinking. 03:23 Chocolate, I think a favourite of almost everybody and then some of the leafy greens which we may not expect. 03:29 Looking at some of the high purine foods would be things like fish, meat. 03:33 Organ meats in particular - liver, kidney tends to have a lot of purines in it and then surprisingly, some of our vegetables like the asparagus and cauliflower will as well. 03:45 Something to note is that calcium intake should be adequate. 03:49 So patients who minimize calcium can actually lead to bone demineralization and worsens stone burden because they are resorbing bone liberating it into the circulation. 04:02 And then finally, fluid intake and particularly what we're looking for are people who are minimizing the fluid intake. 04:11 Physical exam can also hold some important clues for us, we want to look for evidence of systemic disease. 04:16 Remember our patient? he had tophaceous gout. 04:19 When we see something like that, that should be an automatic association thinking about uric acid stones. 04:28 Urine studies are gonna be critical. 04:30 We want to look on the urine analysis for the pH. 04:33 Do they have a high or an alkaline pH, meaning that that pH is greater than 6.5? We're gonna be thinking about certain stones that are gonna precipitate in that environment so things like calcium phosphate or struvite stones. 04:46 How about patients with lower pH? So if you have a lower pH, so a pH of less than 5.5, then we think about things like uric acid stone formation, calcium oxalate stones. 04:57 I do want you to pay attention to that because that's a very popular board question. 05:03 Urine culture is also gonna be important because struvite stones are in particularly associated with urease-producing bacteria. 05:11 Hematuria can also be seen on that urine analysis as we talked about. 05:15 This indicates active stone or crystal passage. 05:18 And then finally specific gravity might be important. 05:21 A very high specific gravity might be a clue that your patient has inadequate hydration. 05:29 Some of the other things that urine studies show are crystals. 05:33 So in particular what I've got shown here in the first image is calcium oxalate stones and if you look on their microscopy, you'll see these beautiful crystals, they almost look like an envelope. 05:44 We can also see struvite crystals in the urine and these often appear as coffin lids and that's how they've been described. 05:53 We also want to get serological or blood work as well. 05:56 We want a look at our patient's serum electrolytes, their creatinine, their calcium and phosphorus and uric acid -these are all things that would help us with clues in terms of what is going on with their underlying condition. 06:08 If we're concerned for example of hypercalcemia or high calcium levels, we want to get a serum parathyroid level. 06:16 Stone analyses are very helpful so if you have a retrieved stone either from your urological intervention or a patient is passing stones and oftentimes they will bring a stone right into your office after they've passed it, that's really critical to get that stone to your pathologist to do a chemical analysis. 06:37 Imaging is also important when it comes to our basic evaluation of stone workup. 06:41 So at the very least, you can get it abdominal radiograph. 06:45 Abdominal radiographs will show radio-opaque stones but I want you to remember, it's not gonna show all stones because uric acid stones are radiolucent. 06:55 The pros or the advantages of getting an abdominal radiograph is that it's inexpensive, it's available maybe all settings. 07:04 The cons, the disadvantages are that it doesn't detect radiolucent stones like uric acid and it's radiation, we can't use it during pregnancy. 07:15 So the image on the right here is an abdominal radiograph and what you can see our two arrows pointing to is that this patient has a radioopaque densities, these are stones in both of his kidneys. 07:27 So another imaging modality and probably what people do most commonly is a non-contrast CT of the abdomen and pelvis, without contrast. 07:36 These stones here are going to appear as bright densities. 07:40 Advantages of doing this? very high sensitivity and specificity for detecting ureteral stones and obstruction. 07:47 It's rapid, you can do it relatively quickly. 07:50 The disadvantages to doing this is that we're really exposing our patients to a fairly high dose of radiation. 07:56 And we certainly can't use it during pregnancy. 07:58 So this is an image on the right that shows an axial section of the CT scan taken through the kidneys, and what you can notice here is that this patient has hyperdensities, so bright densities seen in both the right and left kidney, and these are consistent with stones. 08:15 Now a third imaging modality that we may do is an ultrasound. 08:20 An ultrasound will show stones as an echogenic focus or a bright focus. 08:25 Advantages of doing an ultrasound, it does have a high specificity meaning that if we see the stone, we know it's there There is no radiation exposure and we can use it during pregnancy as well. 08:39 Disadvantages - sensitivity is not as high as CT so if we don't see a stone, it doesn't necessarily rule out that the patient has a stone. 08:50 So that's our basic evaluation. 08:53 What about a complete evaluation? Who needs a complete evaluation? There's certain populations that we really need to think about. 08:59 Any child who presents with stones will need a complete evaluation. 09:04 Non-calcium stones like our patient with the uric acid stones will need a complete evaluation and people who have had multiple recurrent stones that have been particularly increasing in size and number absolutely will need a complete evaluation. 09:19 What is the complete evaluation?pp It's a 24-hour urine collection that will include: volume, phosphorus content, urinary calcium, uric acid, oxalate and citrate.
About the Lecture
The lecture Nephrolithiasis: Clinical Evaluation by Amy Sussman, MD is from the course Nephrolithiasis (Kidney Stones).
Included Quiz Questions
Which of the following medications increases the risk of calcium-based stones?
- Loop diuretics
- Probenecid
- Salicylates
- Acyclovir
- Indinavir
Which of the following kidney stones is radiolucent on abdominal radiographs?
- Uric acid stones
- Calcium phosphate stones
- Calcium oxalate stones
- Struvite stones
Which of the following is characterized by envelope-shaped crystals?
- Calcium oxalate stones
- Struvite stones
- Cystine stones
- Uric acid stones
Which of the following is formed at alkaline pH?
- Calcium phosphate stones
- Cystine stones
- Calcium oxalate stones
- Uric acid stones
Which of the following is a limitation of using non-contrast CT in diagnosing kidney stones?
- It cannot be used during pregnancy.
- Its preparation process is time-consuming.
- It cannot be used in an emergency setting.
- It has low sensitivity for calcium oxalate stones.
- It has low sensitivity for ureteral stones.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |