Playlist
Show Playlist
Hide Playlist
Mycoplasma Pneumoniae
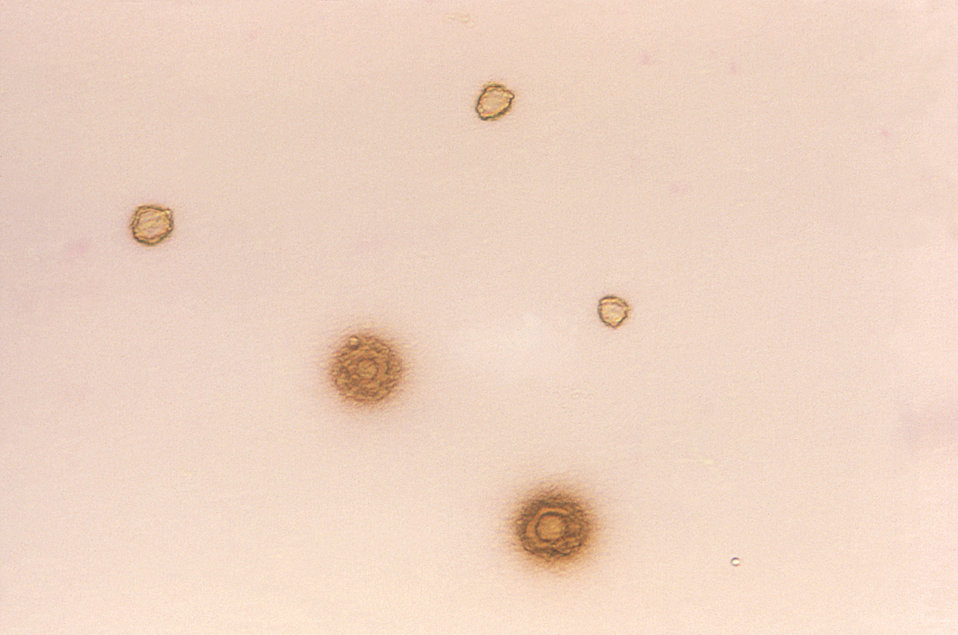
00:01 If we look now specifically at mycoplasma pneumoniae, how does it cause disease? The first step, as it is with pretty much all the bacteria, is an adhesion step. 00:12 In this case, with the P1 adhesin protein. 00:15 This allows mycoplasma pneumoniae to bind tightly to respiratory epithelia. 00:21 Next, it is able to start a cascade of enzymes, lytic, or lysing enzymes, as well as release of super oxides, hydrogen peroxide. 00:32 All of which are going to ultimately trigger an inflammatory cascade. 00:37 If we look at the image, we start with mycoplasma on the left side of the image entering the trachea and then passing down through into the main stem and left and right main stem bronchi. 00:52 Looking then briefly to the right part of the image, we see the mycoplasma binding to the ciliated epithelial or respiratory cells through the P1 adhesin protein. 01:05 When that happens, and this happens at this level of the small airway vessels including into the alveoli, then phagocytosis may occur as an antigen presentation by alveolar macrophages, which are represented by AM on the lower right part of the image. 01:24 An activated alveolar macrophage can then trigger an inflammatory cascade by activating neutrophils on the far right and then lymph structures or lymphocytes, B lymphocytes and T lymphocytes through a normal humoral or antibody associated mechanism of inflammation. 01:46 All of this then, as it precipitates the inflammatory reaction, starts to cause damage to the ciliated epithelium to which the mycoplasma is attached. 01:57 In a way of innocent bystander damage, the activated immune cells, especially the neutrophils will start to cause damage to the affected or bound epithelial cells. 02:10 In addition, as the ciliated epithelial cells are damaged, they start to lose their function with the cilia. 02:18 The cilia, remember, participate in the mucociliary elevator which is a way of bringing mucosal secretions from deep in the lungs up and out to where they're swallowed. 02:29 So, immediate effect of the inflammatory response to the mycoplasma bound the epithelial cells is to poison the mucociliary elevator and cause decreased clearance of those upper airways. 02:43 This then allows further bacteria to spread further into the lungs. 02:48 It's a self-fulfilling prophecy. 02:51 After that, and while that process is occurring, then the organisms are able to elicit a superantigen activity which further elicits an inflammatory cascade and further causes systemic symptoms and very importantly, this whole process only occurs in human cells. 03:12 So, only humans will develop infection from mycoplasma pneumoniae. 03:17 What then does mycoplasma pneumoniae disease look like? It is a principal cause of atypical pneumonia. 03:25 You see in quotes here the term "walking pneumonia", of reference to a pneumonia that is not so severe so that the patient can walk about and in fact, some people say the patient was not that sick, he walked into my office, so how sick could he be? Well, he actually does have a primary infection although it is not a classic lobar pneumonia. 03:48 Transmission of mycoplasma occurs via inhaled aerosolized respiratory droplets from other infected individuals. 03:56 Many patients who are infected actively with mycoplasma pneumoniae, however, may not yet have symptoms and yet they can still be contagious. 04:07 So, its transmission from those carriers, so called, or from somebody who's actively infected that can occur and cause ongoing transmission. 04:17 It helps for transmission for there to be carriers and healthy people in the same close living environment, such as you might see in military recruits, in the barracks and then prisons. 04:29 Once infection develops though, it is an interstitial pneumonia, meaning in the spaces between the alveoli, not in the alveoli themselves, the alveoli do not become inflamed with any sort of exudative fluid. 04:44 Clinical manifestations. 04:47 The patient with Mycoplasma pneumoniae caused pneumonia, on atypical pneumonia, will typically have low-grade symptoms. 04:57 They'll start with some malaise, they'll start with low-grade fever, they'll start with a headache. 05:01 Pretty much what you would imagine is the start of a cold. 05:04 After several days, maybe as many as four days, the patient then develops a nonproductive cough, right, they're not bringing up anything, it's just a dry, irritative cough that they cannot seem to get rid of. 05:16 In addition, if one listens to their lung fields at this time, one will hear the presence of fluid, that interstitial edema, occurring in terms of rales or rhonchi, coarse, rattly or crackly breath sounds which one could hear in the lung fields. 05:33 The patient will then say, "I just feel awful." And they do because they have associated myalgias. 05:39 Their muscles hurt, they have this dry irritative cough, they can't seem to shake, and they have the headache. 05:46 Some patients in a direct antibody mediated response to mycoplasma antigen will also have a hemolytic anemia. 05:55 This is quite rare but it is a known cause of immunoglobulin M-mediated hemolytic anemia. 06:02 Here is a chest radiograph, a chest X-ray showing an atypical pneumonia. 06:07 Note that all the lung fields, both sides have interstitial consolidations. 06:15 So the streaky patchy opacities which you can see prominently especially on the left side of the image or the patient's right chest. 06:24 But one can also see those streaky densities on both sides. 06:28 Perhaps to further clarify an atypical mycoplasma-caused pneumonia from that of a typical or lobar pneumonia, we'll compare and contrast mycoplasma pneumonia and pneumococcal pneumonia. 06:45 Pneumococcal. Streptococcus pneumoniae, a very classic cause of a typical lobar pneumonia. 06:51 Mycoplasma pneumonia remember is interstitial. 06:55 Pneumococcal pneumonia is alveolar, causes flooding of the alveolar spaces. 07:00 Patients with mycoplasma pneumonia many times have a preceding pharyngitis. 07:06 Again, which they may misinterpret as a viral flu or even sometimes streptococcal pharyngitis, strep throat. 07:14 Patients with pneumococcal pneumonia typically launch right into their pneumonia symptoms. 07:19 They don't have preceding findings. 07:21 The onset for mycoplasma, gradual, slow onset, 2-4 days. 07:27 Pneumococcal pneumonia is boom, they're suddenly sick over the course of one or two days with high fevers, shaking chills, rigors, severe malaise. 07:37 The fever I just noted for mycoplasma is low grade. 07:40 The fever for pneumococcal pneumonia, very high grade. 07:43 Again, you're getting a sense of very different severities for these two. 07:48 The cough with mycoplasma pneumonia is nonproductive, it's paroxysmal sometimes but again, the sharp discrete cough as we've mentioned before. 07:57 In pneumococcal pneumonia, the cough is very productive. 08:01 The sputum, which comes out is mucopurulent. 08:04 Many times, it's rusty colored so brownish, orange-ish, it's really quite prominent when one notes that. 08:11 The presence of pleuritic chest pain in mycoplasma pneumonia is absent but is very present in pneumococcal pneumonia. 08:19 Pleuritic chest pain, what happens when the pleura, the lining of the lungs, is inflamed and stretches. 08:26 Pain fibers are present in the pleura themselves, not in the lung parenchyma. 08:30 So in severe pneumococcal pneumonia, stretching the pleura is quite painful, causing a pleuritic chest pain. 08:37 That does not happen in mycoplasma pneumonia. 08:40 Leukocytosis, an elevation of the peripheral white blood cell count, frequently is absent in mycoplasma pneumonia because it doesn't trigger a very overwhelming immune response. 08:51 In pneumococcal pneumonia, it's quite present. 08:53 A peripheral white blood cell count well over 15 or even 20,000 per mm3 is quite, quite common. 09:01 And then, the typical age for patients with mycoplasma pneumonia, it is by and large a disease of younger age, especially of younger adults. 09:11 Beginning in children at around age four or five years old, going up to roughly 30 years of age. 09:18 Although, of course, cases occur on both ends of those extremes. 09:22 In pneumococcal pneumonia, patients at highest risk for severe disease are those who are older in age. 09:28 Age 65 and older, potentially living in a close living environment such as assisted living or nursing home, and certainly those with somewhat of a waning immunity. 09:39 And then, complications. 09:41 In mycoplasma pneumonia, most often these are relatively minor in terms of secondary infections like otitis media but there is a whole host of post-infectious immune-mediated complications such as a rash, erythema multiforme, hemolytic anemia as we mentioned before, inflammatory disease of heart tissues such as myocarditis, pericarditis, even a bullous otitis media. 10:09 In pneumococcal pneumonia, the complications are direct extension of the bacterial infection in other sites. 10:16 Typically starting with bacteremia then extending to meningitis, otitis media, mastoiditis, etc. 10:24 So, looking then at other diseases caused by mycoplasma pneumoniae, atypical pneumonia is absolutely the most common one but one can also see tracheobronchitis which simply means inflammatory disease of the bronchi and it can be several different layers or sizes of the bronchi, main stem all the way down to bronchioles. 10:47 As you see in the image here, there's variable edema of the walls of the bronchi which can variably occlude those bronchi, meaning air cannot passage, or can be so, somewhat more minimally inflamed but with purulent drainage which also can occlude the lumen, the airway of the bronchiole. 11:08 Patients with mycoplasma associated tracheobronchitis will have that same non-productive cough, but in addition, they'll have a little bit higher fever and headache, the sore throat as we talked about, and additionally pharyngeal exudates and cervical lymphadenopathy. 11:25 So, everything we talked about for atypical pneumonia, just worse. 11:29 In most cases of mild or moderate community acquired pneumonia, including that due to mycoplasma pneumonia, there's no need to confirm a specific diagnosis. 11:38 However, if the case is severe and or the patient has underlying complications, then diagnosis via PCR is a preferred modality. 11:46 This is usually typically part of a multiplex panel which picks up other pathogens, and it can be a single specimen to detect those multiple pathogens. However, and very importantly, remember that PCR does not distinguish acute active infection either from colonization or from a past infection. 12:04 We still persistence of microorganisms. 12:07 If one wishes to end to look at the possibility of acute versus past infection, then serology testing is a possibility and or one can do serology testing if PCR is not available. 12:19 In this case, immunoglobulin m antibody is the one to focus on. 12:23 Keeping in mind again that immunoglobulin m antibody can remain positive for up to a year, even after the acute infection has been cleared. 12:31 However, a high titer of immunoglobulin m more likely than not suggests a very active or recent infection. 12:39 Very importantly, in terms of test taking, Mycoplasma pneumoniae does not have a cell wall, so it won't be visible with typical stains such as the gram stain which detects cell wall. 12:51 This is frequently tested on many, many tests. 12:55 So. So staining is not going to help detect the organism. 12:58 However, culturing is possible, but it takes a special media known as Eton's Agar and it can take 2 to 3 weeks to grow that name of the agar. Eton's Eton is something which also might show up on test time to time. 13:14 Pharyngitis. This is something which is somewhat, if not unique to mycoplasma, at least it is highly associated with that. 13:23 The pharyngitis seen in mycoplasma pneumoniae infection will many times precede the atypical pneumonia. 13:31 It is a milder presentation than you might see in other sites of disease and many patients are mistakenly diagnosed with group A streptococcal or even a viral pharyngitis but at the early stages. 13:47 The image you see on the screen shows a very inflamed pharynx and they are in fact, some palatal petechiae if you look closely. 13:55 Petechiae in the palate, the hard or soft palate, many times suggests group A streptococcal infection. 14:02 But in this case, it resembles or represents mycoplasma infection. 14:06 The challenge here is that this, if this is the only manifestation of mycoplasma, may yet still associate with inflammatory, your post-infectious diseases such as Guillain-Barre Syndrome, an ascending paralysis which can be associated with immunologic mimicry between antigens expressed by the mycoplasma pneumoniae and various neurologic structures. 14:32 How to make the diagnosis of mycoplasma pneumoniae. 14:36 Again, because of its growth pattern and its intercellular growth, it's very difficult to grow on culture and when it does grow, it grows very slowly, forming these tiny granular colonies on what's called Eaton's agar. 14:54 Far more successful making diagnoses is to perform serologic tests. 14:58 Here's the problem though, many patients have been exposed to and infected with mycoplasma pneumoniae at some point in their life without knowing it or maybe they did know it but the disease passed so they may already have some immunoglobulin G antibodies, lifelong antibodies mounted to that particular organism. 15:18 So, the key to making diagnosis sirologically for mycoplasma is to look for an escalation or a rise in titer of the immunoglobulin M, the acute stage antibodies in the side of infection. 15:32 This means that one won't be making a short term diagnosis of mycoplasma infection. 15:37 One will need to do acute and convalescent sirologies and compare them, looking for at least a two, or four-fold increase in the tighter. 15:49 Treatment. Most often, treatment for mycoplasma pneumoniae is started empirically. 15:54 We've not yet had time to confirm the diagnosis and yet we don't wish for the infection to progress. 16:00 So most often we'll start with the macrolide antibiotics: erythromycin, azithromycin are examples. 16:06 Patients may not tolerate macrolide antibiotics in which case tetracyclines, fluoroquinolones such as levofloxacin are alternatives, all of which are very successful. 16:18 It's unclear that the length of symptoms with mycoplasma will shorten extensively under the treatment of an antibiotic but certainly the severity of the disease may be mitigated or lessened somewhat by the use of antibiotics. 16:35 Keep in mind again, no peptidoglycan containing cell wall means that there's no target for beta lactam antibiotics to work upon.
About the Lecture
The lecture Mycoplasma Pneumoniae by Sean Elliott, MD is from the course Bacteria.
Included Quiz Questions
Mycoplasma pneumoniae binds to the respiratory epithelial cells by which protein?
- P1 adhesin protein
- Lipoproteins
- P4 adhesin protein
- P2 adhesin protein
- Phosphoproteins
Mycoplasma pneumoniae initiates pathogenesis by releasing which compound?
- Hydrogen peroxide
- Carbon dioxide
- Nitrogen
- Carbon monoxide
- Oxygen
Which of the following groups of individuals are most likely to develop atypical pneumonia caused by Mycoplasma pneumoniae?
- Military recruits
- Fishermen
- Sailors
- Office workers
- Nurses
Which of the following symptoms and signs are most likely to be associated with atypical pneumonia caused by Mycoplasma pneumoniae?
- Nonproductive cough, rhonchi, and myalgia
- Nonproductive cough, wheezing, and myalgia
- Productive cough, rhonchi, and arthralgia
- Nonproductive cough, rhonchi, and arthralgia
- Productive cough, wheezing, and arthralgia
Which of the following features differentiates infection with Mycoplasma pneumoniae from pneumococcal infection?
- Preceding pharyngitis
- Fever
- Cough
- Infiltrates on chest X-ray
- Association with otitis media
Which of the following is a complication of atypical pneumonia caused by Mycoplasma pneumoniae?
- Erythema multiforme
- Meningitis
- Bacteremia
- Endocarditis
- Otitis externa
Which type of lymph nodes are involved in tracheobronchitis caused by Mycoplasma pneumoniae?
- Cervical lymph nodes
- Axillary lymph nodes
- Inguinal lymph nodes
- Mediastinal lymph nodes
- Submandibular lymph nodes
Pharyngitis caused by Mycoplasma pneumoniae is associated with which autoimmune disease?
- Guillain-Barré syndrome
- Graves disease
- Rheumatoid arthritis
- Myasthenia gravis
- Systemic lupus erythematosus
Customer reviews
4,0 of 5 stars
| 5 Stars |
|
3 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
1 |
Well explained with all its components. Better than reading 30 slides of ppt
I dont understand the neg review. This is such a good lecture covering the key points. I found it very helpful
Clear, structured information. Up to date and well done! I would recommend this lecture.
xcvtth wh wtyhy hsh s s wedh dg hj wsj w y. 5 y5 j65e j