Playlist
Show Playlist
Hide Playlist
Lymphadenopathy: Signs and Symptoms of Multiple Myeloma – White Blood Cell Pathology
-
Slides Lymph Nodes.pdf
-
Download Lecture Overview
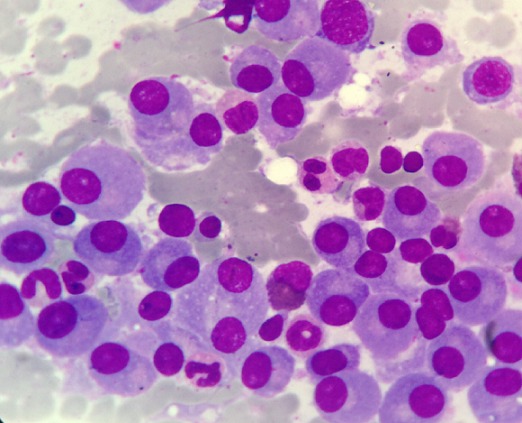
00:01 Continuing our discussion of multiple myeloma, apart from serum protein electrophoresis, what are the features that you expect to find? Well, if you take a look at the skull, you find that you have punched up lesions. 00:15 It's a monoclonal gammopathy, you expect there to be IgG or IgA, but that not IgM. 00:20 And these light chains. 00:22 Light chains are once again into kappa lambda, and majority of them will be kappa. 00:27 And as the picture would show you, oftentimes, actually almost on your boards, they have to give you. 00:33 If they want you to choose multiple myeloma, they'll give you lytic bone lesions, and these are punched out lesions, not wide areas of complete destruction of the bone. 00:44 The reason I bring that to your attention is when I talk about Langerhans cell histiocytosis There'll be a sub tab called eosinophilic granuloma test. 00:53 And that type is where you will also find destruction of the bone, but it's quite chaotic. 00:58 It's not so chaotic, in plasma cell multiple myeloma. 01:02 What I mean by that is the punched out legion almost looks as though that the skull was shot by a bullet going right through it. 01:12 Now, I have to be careful as to how I use the word chaotic though because it is going to cause chaos in your body. 01:19 So once you start having these lytic bone lesions. 01:23 The bone is very, very weak. 01:24 Your patient is not prone to pathologic fractures. 01:27 In addition, the bone which is the major reservoir for calcium. 01:34 The calcium is now being leaked into circulation in great quantity. 01:37 You can expect your patient, no doubt to have hypercalcemia. 01:41 That calcium is going to pass through the glomerulus. 01:44 You can absolutely expect your patient have hypercalciuria. 01:48 And with all this calcium that's now in your urine, who would you not expect there to be calcium stones? Everything is a story Makes you understand as to how the disease initiates from the bone marrow. 02:02 Well, plasma cells, IgG and IGA and how it wreaks havoc on the bone, specifically. 02:09 A couple other things in terms of symptoms. 02:11 I'm giving you the fundamentals of multi-myeloma. 02:14 There'll be other things such as Reuleaux formation, but that is nonspecific. 02:18 And I'll give you a little bit of detail about that. 02:21 And there could be issues with the kidney of Bence-Jones protein. 02:24 But Bence-Jones protein just means light chains. 02:27 You're gonna find light chains and other diseases. 02:29 Lytic bone lesion, bone marrow, plasma cell, multiple myeloma, IgG, IGA, M spike, nonspecific. 02:37 Is that enough information? Absolutely. 02:39 Get your question, right. 02:41 The picture that you're seeing here, upon histology would be from the bone marrow. 02:46 A bone marrow aspirate in which you would then find tons of plasma cells. 02:50 How can you identify these plasma cells? Rows upon, rows of rough endoplasmic reticulum, and if it's multiple myeloma, specifically from the bone marrow, and what kind of immunoglobulins are these den producing please? IgG or IGA? With all this being produced, then what wave is then going to be affected? Good. About M wave and now you have created a M-spike. 03:19 Signs and symptoms of multi-myeloma Talk about that bone. 03:23 So here you might have osteoclastic-activating factor. 03:26 Many times Interleukin-1or 6 might be involved to remember that from immunology? Interleukin 1 or 6, all that osteoclastic activity then causing bone infiltration. 03:38 That'd be chronic pain, the bone is now weakened, your patient is now susceptible to pathologic fracture. 03:44 With all the bone being destroyed, well, no doubt that the patient is suffering hypercalcemia, hypercalciuria, and perhaps calcium stones. 03:54 Renal failure in these patients can occur through one of two mechanisms. 03:58 The first is a result of a high level of immunoglobulin light-chains forming obstructing intratubular cast. 04:04 This is called myeloma cast nephropathy. 04:06 The other mechanism is through amyloid deposition. 04:10 You're going to have amyloid deposition. 04:13 And this amyloid then is stained with your Congo Red, which gives you what color? Good. 04:20 Apple green birefringence. 04:23 In addition, you have these Benjamin's proteins but then you also have Tamm-Horsfall casts. 04:30 And all of this is then going to cause major damage to the tubules eventually leading into renal failure. 04:36 Amyloid deposition. 04:41 What's interesting about plasma cell? Neoplasms or multi-myeloma. 04:46 You would think, you know, just by theory, Dr. Raj you're producing all these immunoglobulins how is it possible that the patient is susceptible to infection. 04:56 You completely lose the proper proper protocol, for isotypes switching of immunoglobulin, Remember you have to have IgM-1. 05:06 You have to have isotype switching into the type of immunoglobulin that's necessary to fend off the antigen or infection. 05:15 In plasma cell multi-myeloma, my goodness, you lose that isotype protocol. 05:21 So therefore, even though you might be producing all of these immunoglobulins, it doesn't mean that you're hyperimmune. 05:27 In fact, just the opposite. 05:30 Your immunity is impaired or compromised, your patient is susceptible to infection. 05:35 You're producing the wrong. 05:36 You've lost the proper organization of immunoglobulin. 05:44 Clinically, who's your patient? Almost always older. 05:48 Now, unfortunately, we don't have proper methods of controlling multi-myeloma, not yet. 05:54 Older the patient gets more to multi-myeloma, I can almost say guaranteed death, unfortunately. 06:01 A very scary. 06:02 Incidence increases with age, prognosis very poor. Look at this. 06:07 three years survival.
About the Lecture
The lecture Lymphadenopathy: Signs and Symptoms of Multiple Myeloma – White Blood Cell Pathology by Carlo Raj, MD is from the course Lymphadenopathy – White Blood Cell Pathology (WBC).
Included Quiz Questions
Which of the following radiographic features is associated with multiple myeloma?
- Lytic lesions in bone
- Scorbutic rosary
- Bone within a bone appearance
- Thinned cortices
- Empty box appearance
Which of the following age groups is more likely to have multiple myeloma?
- 50-70 years
- 20-30 years
- 40-50 years
- 35-40 years
- 25-35 years
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
simplified understanding i used to have difficult understanding Multiple myeloma but grateful to Dr Raj.